King Fahad Medical City 3rd Pediatric ID Course and Workshop
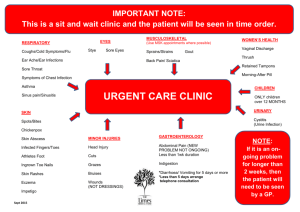
advertisement

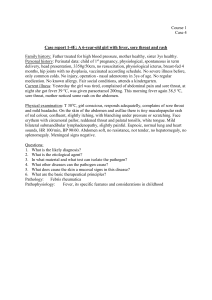
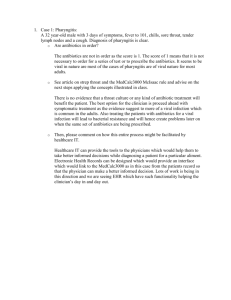
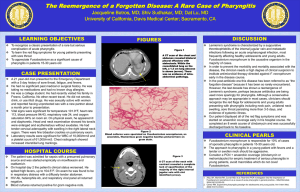
Professor Fahad Abdullah Al Zamil Professor and Consultant, Pediatric Infectious Diseases Head of Pediatric Infectious Diseases Unit King Khalid University Hospital King Saud University November 7, 2012 Clinical scenario: 18 month year old child with H/O fever for 2 days with poor sleeping time. His mother notices that he is pulling his right ear. • What is the diagnosis? •What do you expect to see in the physical examination? Normal Tympanic Membrane Otitis media (in Latin) is the inflammation of the middle ear, or middle ear infection. It occurs in the area between the tympanic membrane and the inner ear, including a duct known as the eustachian tube. It is one of the two most common causes of earache - the other being otitis externa. Diseases other than ear infections can also cause ear pain, including cancers of any structure that shares nerve supply with the ear and shingles which can lead to herpes zoster oticus. Though painful, otitis media is not threatening and usually heals on its own within 2–6 weeks. Diagnosis Acute otitis media is usually diagnosed via visualization of the tympanic membrane in combination with the appropriate clinical history. The use of a monocular otoscope and perhaps a tympanometer may not be able to distinguish bacterial versus viral etiology, especially if the canal is small and there is wax in the ear that obscures a clear view of the eardrum. Also, an upset child's crying can cause the eardrum to look inflamed due to distension of the small blood vessels on it, mimicking the redness associated with otitis media. The occurrence, duration, or severity of symptoms is not predictive of an ear infection in the absence of examination of the eardrum. Clinical scenario An 18-month-old girl is seen by her GP. A mild fever of 38.0 degrees Celsius, hoarseness, a barking cough, and symptoms over the last 48 hours, which are worse at night, have been noted. 1.) What is the diagnosis? 2.) What three organisms are most likely to be responsible 3.) What are your immediate actions in the Emergency Department? 4.) What three drugs may be useful in treatment? Streptococcus Pharyngitis Granular Pharyngitis Pharyngitis Pharyngitis comes from the Greek word pharynx meaning throat and the suffix -itis meaning inflammation. It is an inflammation of the throat. In most cases it is quite painful, and is the most common cause of a sore throat. Like many types of inflammation, pharyngitis can be acute – characterized by a rapid onset and typically a relatively short course – or chronic. Pharyngitis can result in very large tonsils which cause trouble swallowing and breathing. Pharyngitis can be accompanied by a cough or fever, for example, if caused by a systemic infection. Most acute cases are caused by viral infections (40–80%), with the remainder caused by bacterial infections, fungal infections, or irritants such as pollutants or chemical substances. Treatment of viral causes are mainly symptomatic while bacterial or fungal causes may be amenable to antibiotics and anti-fungal respectively. Cause The majority of cases are due to an infectious organism acquired from close contact with an infected individual. Infectious Viral These comprise about 40–80% of all infectious cases and can be a feature of many different types of viral infections.[2][3] •Adenovirus – the most common of the viral causes. Typically the degree of neck lymph node enlargement is modest and the throat often does not appear red, although it is very painful. •Orthomyxoviridae which cause influenza – present with rapid onset high temperature, headache and generalised ache. A sore throat may be associated. •Infectious mononucleosis ("glandular fever") caused by the Epstein-Barr virus. This may cause significant lymph gland swelling and an exudative tonsillitis with marked redness and swelling of the throat. The heterophile test can be used if this is suspected. •Herpes simplex virus can cause multiple mouth ulcers. •Measles •Common cold: rhinovirus, coronavirus, respiratory syncytial virus, parainfluenza virus can cause infection of the throat, ear, and lungs causing standard cold-like symptoms and often extreme pain. Bacterial A number of different bacteria can infect the human throat. The most common is Group A streptococcus, however others include Corynebacterium diphtheriae, Neisseria gonorrhoeae, Chlamydophila pneumoniae, and Mycoplasma pneumoniae. Streptococcal pharyngitis A case of strep throat Streptococcal pharyngitis or strep throat is caused by group A beta-hemolytic streptococcus (GAS). It is the most common bacterial cause of cases of pharyngitis (15–30%). Common symptoms include fever, sore throat, and large lymph nodes. It is a contagious infection, spread by close contact with an infected individual. A definitive diagnosis is made based on the results of a throat culture. Antibiotics are useful to both prevent complications and speed recovery.[8] Diagnostic approach Modified Centor score Points Probability of Strep Management 1 or less <10% No antibiotic or culture needed 2 11–17% Antibiotic based on culture or RADT 3 28–35% 4 or 5 52% Empiric antibiotics It is hard to differentiate a viral and a bacterial cause of a sore throat based on symptoms alone. Thus often a throat swab is done to rule out a bacterial cause. The modified Centor criteria may be used to determine the management of people with pharyngitis. Based on 5 clinical criteria, it indicates the probability of a streptococcal infection. One point is given for each of the criteria: •Absence of a cough •Swollen and tender cervical lymph nodes •Temperature >38.0 °C (100.4 °F) •Tonsillar exudate or swelling •Age less than 15 (a point is subtracted if age >44) •The McIsaac criteria adds to the Centor: •Age less than 15: add one point •Age greater than 45: subtract one point The Infectious Disease Society of America however recommends against empirical treatment and considers antibiotics only appropriate following positive testing. Testing is not needed in children under three as both group A strep and rheumatic fever are rare, except if they have a sibling with the disease Management The majority of time treatment is symptomatic. Specific treatments are effective for bacterial, fungal, and herpes simplex infections. Medications •Analgesics such as NSAIDs and acetaminophen can help reduce the pain associated with a sore throat. (Note: Don't use salicylates, like aspirin, for influenza: Increased risk of Reyes Syndrome) •Steroids (such as dexamethasone) have been found to be useful for severe pharyngitis. •Viscous lidocaine relieves pain by numbing the mucus membranes. •Antibiotics are useful if a bacterial infection is the cause of the sore throat. For viral infections, antibiotics have no effect.[22] •Oral analgesic solutions, the active ingredient usually being Phenol, but also less commonly Benzocaine, Cetylpyridinium chloride and/or Menthol. Chloraseptic and Cēpacol are two examples of brands of these kinds of analgesics. Alternative Alternative medicines are promoted and used for the treatment of sore throats. However, they are poorly supported by evidence; UpToDate, an evidence-based peer-reviewed resource, recommends that they not be used to treat pharyngitis. Epidemiology Acute pharyngitis is the most common cause of a sore throat and sore throat and cough is diagnosed in more than 1.9 million people a year in the United States. Diarrheal disease •Diarrheal disease is the second leading cause of death in children under five years old. It is both preventable and treatable. •Diarrheal disease kills 1.5 million children every year. •Globally, there are about two billion cases of diarrhoeal disease every year. •Diarrheal disease mainly affects children under two years old. •Diarrhea is a leading cause of malnutrition in children under 5 years old. Diarrheal diseases affect people of all ages throughout the world. Children, however, are the most vulnerable; diarrhea is the second leading causes of death worldwide in children under the age of five, accounting for approximately 1.5 million deaths per year.1 More than 80% of these deaths occur in Africa and Southeast Asia.2