5th cranial Nerve
advertisement

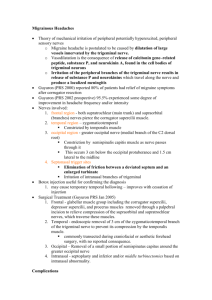
5th Cranial Nerve (Trigeminal Nerve) Dr D V Siva Kumar Asso Professor Gen Medicine Anatomy of the Trigeminal Nerve 5th Nerve subserves facial sensation and innervates muscles of mastication Anatomy : Trigeminal central connections are complex Anatomy of the Trigeminal Nerve Dissociated sensory loss : Def : loss of pain and temperature sensation with preservation of light touch The separate location of the main sensory nucleus and nucleus of the descending trigeminal tract account for dissociated sensory loss i.e., a low pontine or medullary lesion will result in this loss Low pontine medullary and cervical lesions produce a characteristic ‘onion skin’ distribution of pinprick and temperature loss. An ascending lesion spares the muzzle area until last. Anatomy of the Trigeminal Nerve Peripheral course of 5th Nerve : The motor and sensory nerve roots emerge separately from the lateral aspect of the brain stem at the mid pontine level. The gasserian ganglean of the sensory root contains bipolar sensory nuclei and lies on the apex of the petrous bone in the middle fossa. Here the 3 divisions of the 5th nerve emerge. Each passes through its own foremen and carries sensation from a specific area of the face Ophthalmic division passes through the superior orbital fissure divides into branches with in the orbit and emerges from the supra orbital foramen to innervate the forehead. Maxillary division passes through the foramen rotundum into the pterygo palatine fossa, then through the infro orbital foramen to become the infra orbital nerve The mandibular division exists from the foramen ovale the anterior division incorporates the motor branch of the 5th nerve innervating the muscles of mastication – massater, pterygoids and temporalis – as well as innervating the cheeks and gums (buccal nerve) The lingual branch of the posterior trunk innervates the anterior 2/3rd of the tongue and is joined by the chordi tympani from the facial nerve carrying salivary secreto motor fibers and taste from the anterior 2/3rd of the tongue. Diseases of the 5th Nerve Causes of the 5th nerve lesions : At the level of pons : - When associated with other cranial nerve palsies and long tract signs * Vascular * Neoplastic * Demyelination * Syringobulbia (especially dissociated sensory loss) At the level of petrous apex : - 6th nerve palsy - Petrositis (gradenigo’s syndrome) At the level of cerebello pontine angle - Associated with other cranial nerve palsies with or without long tract signs - Acoustic neuroma - Trigeminal neuroma - Subacute (chronic) meningitis At the level of - orbital fissure - orbit - cavernous sinus 1st division of the 5th nerve with or without 3rd, 4th, 6th nerver palsies At the level of skull base : one or more 5th nerve divisions will be involved - Nasopharyngeal or metastatic carcinoma - Trauma Syndromes of 5th nerve lesions : Sensory trigeminal neuropathy Mental neuropathy Infra orbital neuropathy Gradenigo’s syndrome Neuropathic Keratitis Trigeminal neuralgia (tic douloureux) Symptoms : Paroxysmal attacks of severe, sharp, stabbing pain affecting one or more divisions of the 5th nerve The pain involves 2nd or 3rd divisions more often than the 1st. It rarely occurs bilaterally and never simultaneously on each sign Paroxysmal attacks last for several days or weeks, they are often super imposed on a more constant ache. When attacks settle the patients may remain pain free for many months. Chewing, speaking, washing the face, tooth brushing, cold winds are touching a specific ‘trigger spot’. Eg., Upper lip or gum may precipitate an attack of pain. Trigeminal neuralgia more commonly affects females and patients over 50 years of age. Aetiology : Trigeminal pain may be symptomatic or disorders which affect the nerve root or its entry zone. - Root or root entry zone compression * Arterial vessels often abut and some times clearly indent the 5th nerve root at the entry zone into the pons causing ephaptic transmission (short circuiting) * Tumours of the CP angle lying the against the 5th nerve roots. Eg., Meningioma, frequently present with trigeminal pain - Demyelination * Such a lesion in the pons should be considered in a young person with trigeminal neuralgia Investigations : CT or preferably MR Scan Management : Drug Therapy - Carbamazepine throughs affective in most patients and helps confirm the diagnosis. Dosage is increased until the pain relief occurs (600mg – 1600 mg / day) - Toxicity - drowsiness, ataxia - When remission established drug treatment can be discontinued. - If the pain control is limited other drugs. Eg., Baclofen, Lamotrigine, Gabapentin, Phenytoin may benefit. Other Therapies : Operative therapy - Peripheral nerve techniques – Nerve block with alcohol or phenol provides temporary relief. Avulsion supra or infra orbital nerves gives more prolonged relief - Radio surgical lesion of the trigeminal ganglion provides another alternative for high risk surgical patients - Trigeminal root section through either a subtemporal or posterior fossa approach, the appropriate trigeminal root is identified and divided - Microvascular decompression – exploration of the cp angles reveals blood vessels in contact with the trigeminal nerve root or root entry zone, separation of these structures and insertion of a non-absorbable sponge produces pain relief. - Radio frequency thermocoagulation – under general anaesthetic produces a permanent lesion usually resulting in analgesia of the appropriate area with retention of light touch. Results & Complications : Pain relief – approximately 80-85% patients remain pain free for a 5 year period. Although some may relapse in the long term particularly after balloon compression or glycerol injection. Results of peripheral nerve avulsion or less satisfactory with pain recurring in 50% within 2 years Dysaesthesia / Anaesthesia Dolorosa – This troublesome sensory disturbance follows any destructive technique to the nerve or root in 5-30% of the patients. Microvascular decompression avoids this problem. Cornial anaesthesia – This occurs when root section or thermo coagulation involves the first division and keratitis may result. Mortality – Microvascular decompression and open roof section carry a very low mortality < 1%. Treatment Selection : In most centers absence of sensory complications make microvascular decompression the procedure of choice particularly for first division pain and for younger patients. Frail and elderly patients may tolerate glycerol injection balloon compression and thermo coagulation more easily.