2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES
advertisement

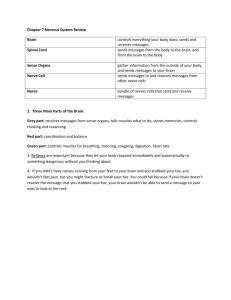
2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES INTRODUCTION TO PERIPHERAL NERVOUS SYSTEM The nervous system comprises the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS is surrounded and protected by the skull (neurocranium) and vertebral column and consists of the brain and the spinal cord. The PNS exists primarily outside these bony structures. One neuron communicates with other neurons or glands or muscle cells across a junction between cells called a synapse. Typically, communication is transmitted across a synapse by means of specific neurotransmitters, such as acetylcholine, epinephrine, and norepinephrine, but in some cases in the CNS by means of electric current passing from cell to cell. The central nervous system consists of the brain and spinal cord, and the peripheral nervous system consists of the sensory and motor nerves that are distributed throughout the body and that convey information to and from the brain (via 12 pairs of cranial nerves) and the spinal cord (via 31 pairs of spinal nerves). The peripheral nervous system is divided into the somatic nervous system and the autonomic nervous system. The somatic nervous system is the part of the PNS that innervates the skin, joints, and skeletal muscles. The autonomic nervous system (ANS) is the part of the PNS that innervates internal organs, blood vessels, and glands. The PNS encompasses the nervous system external to the brain and spinal cord. In the PNS, axons (fibers) are collected into bundles supported by connective tissue to form a nerve. The nervous system contains both the somatic system and the autonomic system, each with portions within the CNS and PNS. The somatic system mediates information between the CNS and the skin, skeletal muscles (voluntary movements), bones, and joints. The autonomic system, in contrast, mediates information between the CNS and organs (involuntary movements). In both the somatic system and autonomic system, neurons and their nerves are classified according to function. Individual neurons that carry impulses away from the CNS are called efferent, or motor neurons. The axons of these multipolar neurons are also referred to as efferent fibers and they synapse on muscles or glands. Neurons that carry impulses to the CNS are called afferent, or sensory, neurons. The term “peripheral nerve” such as sciatic nerve, ulnar nerve etc. should not be confused by the spinal nerve. Peripheral nerve is the last product of these somatic networks; somatic plexuses. The anterior rami form plexuses (network). All major somatic plexuses (cervical, brachial, lumbar, and sacral) are formed by anterior rami (ramus=branch, rami=branches). The spinal cord is a long tubular structure that is divided into a peripheral white matter (composed of myelinated axons) and a central gray matter (cell bodies and their connecting fibers). When viewed in cross section, the gray matter has pairs of horn-like projections into the surrounding white matter. These horns are called ventral horns, dorsal horns, and lateral horns, but in three dimensions they represent columns that run the length of the spinal cord. Ventral horn of the spinal cord: Motor neurons Lateral horn of the spinal cord: Thoracal and lumbar regions: sympathetetic system neurons S2-S4 (S=Sacral) segments: parasympathetic system neurons Dorsal horn of the spinal cord: Sensory neurons A spinal nerve contains motor and sensory fibers, as well as sympathetetic and parasympathetic fibers depending on the level of the segment. A spinal cord segment is the portion of the spinal cord that gives rise to a pair of spinal nerves. Thus, the spinal cord gives rise to 8 pairs of cervical nerves (C1–C8), 12 pairs of thoracic nerves (T1–T12), 5 pairs of lumbar nerves (L1–L5), 5 pairs of sacral nerves (S1–S5), and 1 pair of coccygeal nerves (Co1). The spinal cord segments are numbered in the same manner as these nerves. The first motor neuron is located in the precentral gyrus in the primary motor cortex. This cortex strip is located in the frontal lobe. The somatosensory cortex, or SI, in the postcentral gyrus of each hemisphere receives sensory information from the contralateral side of the body about touch, pain, temperature, vibration, proprioception (body position), and kinesthesis (body movement). 1 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES INTRODUCTION TO CARDIOVASVULAR SYSTEM Cardiovascular (Circulatory) System transports fluids throughout the body. The heart and blood vessels make up the blood transportation network, the cardiovascular system. The vascular system is divided for descriptive purposes into (a) the blood vascular system, which comprises the heart and blood vessels for the circulation of the blood; and (b) the lymph vascular system, consisting of lymph glands and lymphatic vessels, through which a colorless fluid, the lymph, circulates. The two systems communicate with each other and are intimately associated developmentally. The heart pumps blood throughout the body, and the blood vessels, which are a closed network of tubes that transport the blood. There are three types of blood vessels: arteries, which transport blood away from the heart; veins, which transport blood toward the heart; capillaries, which connect the arteries and veins, are the smallest of the blood vessels, and are where oxygen, nutrients, and wastes are exchanged within the tissues. Arteries are usually further subdivided into three classes, according to the variable amounts of smooth muscle and elastic fibers contributing to the thickness of the tunica media, the overall size of the vessel, and its function. a. Large elastic arteries contain substantial amounts of elastic fibers in the tunica media, allowing expansion and recoil. This helps maintain a constant flow of blood to the heart. An example is the aorta. b. Medium muscular arteries are composed of a tunica media that contains mostly smooth muscle fibers. This characteristic allows these vessels to regulate their diameter and control the flow of blood to different parts of the body. An example is the radial artery. c. Small arteries and arterioles control the filling of the capillaries and directly contribute to the arterial pressure in the vascular system. Veins also are subdivided into three classes. a. Large veins contain some smooth muscle in the tunica media, but the thickest layer is the tunica externa. Examples of large veins are the superior vena cava, and the inferior vena cava. b. Small and medium veins contain small amounts of smooth muscle, and the thickest layer is the tunica externa. Examples of small and medium veins are superficial veins in the upper and lower limbs and deeper veins of the leg and forearm. c. Venules are the smallest veins and drain the capillaries. The right side of the heart (right heart) receives poorly oxygenated (venous) blood from the body through the superior vena cava (SVC) and inferior vena cava (IVC) and pumps it through the pulmonary trunk and arteries to the lungs for oxygenation. The left side of the heart (left heart) receives welloxygenated (arterial) blood from the lungs through the pulmonary veins and pumps it into the aorta for distribution to the body. The right and left brachiocephalic veins are formed by the union of the internal jugular and subclavian veins. The brachiocephalic veins unite to form the superior vena cava (SVC). The superior vena cava (SVC) returns blood from all structures superior to the diaphragm, except the lungs and heart. It ends by entering the right atrium of the heart. The inferior vena cava (IVC) returns blood from the lower part of the body including the lower limbs right into the right atrium. The ascending aorta begins at the aortic orifice. Its only branches are the coronary arteries, arising from the aortic sinuses. The arch of the aorta (aortic arch) is the curved continuation of the ascending aorta. The usual branches of the arch are the brachiocephalic trunk, left common carotid artery, and left subclavian artery. The subclavian artery will continue as axillary artery, and later brachial artey on both arms. The brachial artery will then divide into two terminal branches: ulnar and radial arteries. What happens to descending aorta (thoracic aorta) which is the continuation of the arch of aorta is that after passing through the diaphragm, it becomes the abdominal aorta which finally terminates as common iliac arteries which will then bifurcate into the external and internal iliac arteries. The external iliac arteries, after passing below the inguinal ligament, will become femoral arteries. The femoral arteries will supply the lower limbs. On both sides, these arteries will continue as popliteal arteries which then will branch into anterior and posterior tibial arteries. The common carotid artery will divide into external carotid artery and 2 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES internal carotid artery. The external carotid artery basically supplies blood to the face and neck, and the internal one to the brain. The other artery of the brain is the vertebral artery which is a thick branch of the subclavian artery. AXILLA The axilla is the gateway to the upper limb from the trunk. It provides an area of transition between the neck and the arm. It is the pyramidal space inferior to the glenohumeral joint at the junction of the arm and thorax. The axilla provides a passageway, or “distribution center,” usually protected by the adducted upper limb, for the neurovascular structures that serve the upper limb. Formed by the clavicle, the scapula, the upper thoracic wall, the humerus, and related muscles, the axilla is an irregularly shaped pyramidal space with: four walls, an inlet (apex) and a floor (base). Gateways in the posterior wall Passing through the quadrangular space are the axillary nerve and the posterior circumflex humeral artery and vein. The triangular space is an area of communication between the axilla and the posterior scapular region. The circumflex scapular artery and vein pass into this space.The radial nerve passes out of the axilla traveling through this interval to reach the posterior compartment of the arm. The profunda brachii artery (deep artery of arm) and associated veins also passthrough the triangular interval. The axilla contains the axillary artery and its branches, which supply blood to the upper limb; the axillary vein and its tributaries, which drain blood from the upper limb; and lymph vessels and lymph nodes, which drain lymph from the upper limb and the breast and from the skin of the trunk, down as far as the level of the umbilicus. Generally, six branches arise from the axillary artery: 1 branch, the superior thoracic artery, originates from the first part; 2 branches, the thoraco-acromial artery and the lateral thoracic artery, originate from the second part; 3 branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part. BRACHIAL PLEXUS Most nerves in the upper limb arise from the brachial plexus, a major nerve network supplying the upper limb; it begins in the neck and extends into the axilla. Almost all branches of the brachial plexus arise in the axilla (after the plexus has crossed the 1st rib). The brachial plexus is formed by the union of the anterior rami of the last four cervical (C5-C8) and the first thoracic (T1) nerves, which constitute the roots of the brachial plexus. It originates in the neck, passes laterally and inferiorly over rib I, and enters the axilla. The parts of the brachial plexus, from medial to lateral, are roots, trunks, divisions, and cords. All major nerves that innervate the upper limb originate mostly from the cords. The roots of the brachial plexus are the anterior rami of C5 to C8, and most of T1. In the inferior part of the neck, the roots of the brachial plexus unite to form three trunks: • Superior trunk is formed by the union of C5 and C6 roots; •Middle trunk is a continuation of the C7 root; •Inferior trunk is formed by the union of the C8 and T1 roots. Each trunk of the brachial plexus divides into anterior and posterior divisions. The three cords of the brachial plexus originate from the divisions; lateral cord (C5-C7), medial cord (C8-T1), posterior cord (C5 to T1). Branches of the lateral cord Three nerves originate entirely or partly from the lateral cord. 1) Lateral pectoral nerve 2) Musculocutaneous nerve 3) Lateral root of median nerve Branches of the medial cord 1) Medial pectoral nerve. 2) Medial cutaneous nerve of arm (medial brachial cutaneous nerve) 3 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES 3) Medial cutaneous nerve of forearm (medial antebrachial cutaneous nerve) 4) Ulnar nerve 5) Median nerve Branches of the posterior cord 1) Superior subscapular nerve 2) Thoracodorsal nerve 3) Inferior subscapular nerve 4) Axillary nerve 5) Radial nerve INTRODUCTION TO MYOLOGY The muscular system consists of all the muscles of the body. The disciplined related to the study of muscles is myology. Three types of muscle are described based on distinct characteristics relating to: • Whether it is normally willfully controlled (voluntary vs. involuntary). • Whether it appears striped or unstriped when viewed under a microscope (striated vs. smooth or unstriated). • Whether it is located in the body wall (soma) and limbs or makes up the hollow organs (viscera) of the body cavities or blood vessels (somatic vs. visceral). There are three muscle types: skeletal striated muscle, cardiac striated muscle and smooth muscle (unstriated muscle). All skeletal muscles commonly referred to simply as “muscles,” have fleshy, reddish, contractile portions (one or more heads or bellies) composed of skeletal striated muscle. Some muscles are fleshy throughout, but most also have white non-contractile portions (tendons), composed mainly of organized collagen bundles, that provide a means of attachment. When referring to the length of a muscle, both the belly and the tendons are included. In other words, a muscle's length is the distance between its attachments. Most skeletal muscles are attached directly or indirectly to bones, cartilages, ligaments, or fascias or to some combination of these structures. Muscles are organs of locomotion (movement), but they also provide static support, give form to the body, and provide heat. Many terms provide information about a structure's shape, size, location, or function or about the resemblance of one structure to another. When a muscle contracts and shortens, one of its attachments usually remains fixed while the other (more mobile) attachment is pulled toward it, often resulting in movement. Attachments of muscles are commonly described as the origin and insertion. Types of contractions of a muscle are; reflexive, tonic and phasic contractions. SUPERFICIAL MUSCLES OF THE BACK There are two major groups of muscles in the back: The extrinsic back muscles include superficial and intermediate muscles that produce and control limb and respiratory movements, respectively. The intrinsic (deep) back muscles include muscles that specifically act on the vertebral column, producing its movements and maintaining posture. Muscles in the superficial and intermediate groups are extrinsic muscles because they originate embryologically from locations other than the back. They are innervated by anterior rami of spinal nerves: •Superficial group consists of muscles related to and involved in movements of the upper limb; •Intermediate group consists of muscles attached to the ribs and may serve as a respiratory function. Muscles in the superficial group include: Trapezius Latissimus dorsi Rhomboid major Rhomboid minor Levator scapulae 4 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES Rhomboid major, rhomboid minor, and levator scapulae are located deep to trapezius in the superior part of the back. Although located in the back region, for the most part these muscles receive their nerve supply from the anterior rami of cervical nerves and act on the upper limb. The trapezius receives its motor fibers from a cranial nerve, the spinal accessory nerve (CN XI). The trapezius attaches the pectoral girdle to the cranium and vertebral column and assists in suspending the upper limb. Descending (superior) fibers elevate the scapula (e.g., when squaring the shoulders). Middle fibers retract the scapula (i.e., pull it posteriorly). Ascending (inferior) fibers depress the scapula and lower the shoulder. The name latissimus dorsi (L. widest of back) was well chosen because the muscle covers a wide area of the back. Latissimus dorsi is a large, flat triangular muscle that begins in the lower portion of the back and tapers as it ascends to a narrow tendon that attaches to the humerus anteriorly. Movements associated with this muscle include extension, adduction, and medial rotation of the upper limb. Latissimus dorsi can also depress the shoulder, preventing its upward movement. The thoracodorsal nerve of the brachial plexus innervates the latissimus dorsi muscle. From the transverse processes of the upper cervical vertebrae, the fibers of the levator of the scapula pass inferiorly to the superomedial border of the scapula. True to its name, the levator scapulae acts with the descending part of the trapezius to elevate the scapula, or fix it (resists forces that would depress it, as when carrying a load. Levator scapulae is innervated by branches from the anterior rami of spinal nerves C3 and C4 and the dorsal scapular nerve. The rhomboids (major and minor), which are not always clearly separated from each other, have a rhomboid appearance. The two rhomboid muscles lie deep to the trapezius, inferior to levator scapulae and form broad parallel bands that pass inferolaterally from the vertebrae to the medial border of the scapulae. Rhomboid minor is superior to rhomboid major. The rhomboids retract and rotate the scapula, depressing its glenoid cavity. The dorsal scapular nerve innervates both rhomboid muscles. The muscles in the intermediate group of back muscles consist of two thin muscular sheets in the superior and inferior regions of the back, immediately deep to the muscles in the superficial group; serratus posterior superior and serratus posterior inferior muscles. These muscles are related to the movements of the thoracic cage, as the superficial muscles are related to the movements of the shoulder (girdle). These two muscles are innervated by the anterior rami of upper thoracic nerves. THORACIC WALL Thorax is the region between the neck and the abdomen. The terms chest and thorax are used interchangebly. Thoracic wall: bounds the thoracic cavity which mainly includes the heart and the lungs. The throracic wall is formed by the skin, bones, fasciae, and muscles. Thoracic cage: the bony portion of the thoracic wall, also known as thoracic skeleton. Thoracic cavity: The cavity between neck and abdomen and is protected by the thoracic wall. Skeleton of the thoracic wall is formed by by the 12 thoracic vertebræ and the posterior parts of the ribs posteriorly, sternum and costal cartilages anteriorly and ribs, separated from each other by the intercostal spaces laterally. The thorax includes the primary organs of the respiratory and cardiovascular systems. The thorax is one of the most dynamic regions of the body. Although the joints between the bones of the thorax have limited movement ability, the whole outcome of these movements permits expansion of the cavity during inspiration. During inspiration, the thoracic cavity can expand in antero-posterior, vertical and transverse dimensions. While the thoracic cage provides a complete wall peripherally, it is open superiorly and inferiorly; superior and inferior thoracic apertures. 5 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES Muscles of the thoracic wall are; serratus posterior, levator costarum, intercostal (external, internal and innermost), subcostal, and transverse thoracic. These muscles either elevate or depress the ribs helping to increse the volume of the thoracic cavity. The arterial supply to the thoracic wall derives from the: • Thoracic aorta, through the posterior intercostal and subcostal arteries. • Subclavian artery, through the internal thoracic and supreme intercostal arteries. • Axillary artery, through the superior and lateral thoracic arteries. The intercostal veins accompany the intercostal arteries, nerves and lie most superior in the costal grooves (VAN). The 12 pairs of thoracic spinal nerves supply the thoracic wall. 1st intercostal nerve, 2nd intercostal nerve, 7th-11th intercostal nerve and 12th intercostal nerve are considered as atypical intercostal nerves. BREASTS The female breast rests on a bed that extends transversely from the lateral border of the sternum to the midaxillary line and vertically from the 2nd through 6th ribs. A small part of the mammary gland may extend along the inferolateral edge of the pectoralis major toward the axillary fossa, forming an axillary process or tail (of Spence). The mammary gland is firmly attached to the dermis of the overlying skin, especially by the suspensory ligaments (of Cooper). Most lymph (>75%), especially from the lateral breast quadrants, drains to the axillary lymph nodes, initially to the anterior or pectoral nodes for the most part. Most of the remaining lymph, particularly from the medial breast quadrants, drains to the parasternal lymph nodes or to the opposite breast, whereas lymph from the inferior quadrants may pass deeply to abdominal lymph nodes (subdiaphragmatic inferior phrenic lymph nodes). SHOULDER The shoulder is the region of upper limb attachment to the trunk. Shoulder is the proximal segment of the limb that overlaps parts of the trunk (thorax and back) and lower lateral neck. It includes the pectoral, scapular, and deltoid regions of the upper limb, and the lateral part (greater supraclavicular fossa) of the lateral cervical region. It overlies half of the pectoral girdle. The bone framework of the shoulder consists of: • the clavicle and scapula, which form the pectoral girdle (shoulder girdle); and • the proximal end of the humerus. The superficial muscles of the shoulder consist of the trapezius and deltoid muscles, which together form the smooth muscular contour over the lateral part of the shoulder. These muscles connect the scapula and clavicle to the trunk and to the arm, respectively. The three joints in the shoulder complex are the sternoclavicular, acromioclavicular, and glenohumeral joints. The two most superficial muscles of the shoulder are the trapezius and deltoid muscles. Together, they provide the characteristic contour of the shoulder: • trapezius attaches the scapula and clavicle to the trunk; • deltoid attaches the scapula and clavicle to the humerus. The superficial posterior axioappendicular (extrinsic shoulder) muscles are the trapezius and latissimus dorsi. The deep posterior thoracoappendicular (extrinsic shoulder) muscles are the levator scapulae and rhomboids. These muscles provide direct attachment of the appendicular skeleton to the axial skeleton. The six scapulohumeral muscles (deltoid, teres major, supraspinatus, infraspinatus, subscapularis, and teres minor) are relatively short muscles that pass from the scapula to the humerus and act on the glenohumeral joint. All the intrinsic muscles but the deltoid and the subscapularis are muscles of the posterior scapular region. The deltoid muscle is large and triangular in shape, with its base attached to the scapula and clavicle and its apex attached to the humerus. It originates along a continuous U-shaped line of attachment to the clavicle and the scapula, mirroring the adjacent insertion sites of the trapezius muscle. The major function of the deltoid muscle is abduction of the arm beyond the initial 15° accomplished by the supraspinatus muscle. 6 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES The subscapularis is the primary medial rotator of the arm and also adducts it. It joins the other rotator cuff muscles in holding the head of the humerus in the glenoid cavity during all movements of the glenohumeral joint (i.e., it helps stabilize this joint during movements of the elbow, wrist, and hand). The posterior scapular region occupies the posterior aspect of the scapula and is located deep to the trapezius and deltoid muscles. It contains four muscles, which pass between the scapula and proximal end of the humerus: supraspinatus, infraspinatus, teres minor, and teres major muscles. The supraspinatus, infraspinatus, and teres minor muscles are components of the rotator cuff, which stabilizes the glenohumeral joint. The suprascapular nerve passes through the suprascapular foramen; the suprascapular artery and the suprascapular vein follow the same course as the nerve, but normally pass immediately superior to the superior transverse scapular ligament and not through the foramen. Quadrangular space, triangular space and triangular interval are other gateways in the posterior scapular region. The two major nerves of the posterior scapular region are the suprascapular and axillary nerves, both of which originate from the brachial plexus in the axilla. Three major arteries are found in the posterior scapular region: the suprascapular, posterior circumflex humeral, and circumflex scapular arteries. These arteries contribute to an interconnected vascular network around the scapula. Veins in the posterior scapular region generally follow the arteries and connect with vessels in the neck, back, arm, and axilla. ARM The arm is the region of the upper limb between the shoulder and the elbow. The superior aspect of the arm communicates medially with the axilla. Inferiorly, a number of important structures pass between the arm and the forearm through the cubital fossa, which is positioned anterior to the elbow joint. The arm is divided into two compartments by medial and lateral intermuscular septa, which pass from each side of the humerus to the outer sleeve of deep fascia that surrounds the limb. Two types of movement occur between the arm and the forearm at the elbow joint: flexion-extension and pronation-supination. The muscles performing these movements are clearly divided into anterior and posterior groups, separated by the humerus and medial and lateral intermuscular septae. The anterior compartment of the arm contains muscles that predominantly flex the elbow joint; the posterior compartment contains muscles that extend the joint. Major nerves and vessels supply and pass through each compartment. The chief action of both groups is at the elbow joint, but some muscles also act at the glenohumeral joint. The skeletal support for the arm is the humerus. The anterior compartment of the arm contains three muscles-coracobrachialis, brachialis, and biceps brachii muscles-which are innervated predominantly by the musculocutaneous nerve. The posterior compartment contains one muscle-the triceps brachii muscle-which is innervated by the radial nerve. The flexor muscles of the anterior compartment are almost twice as strong as the extensors in all positions; consequently, we are better pullers than pushers. The biceps is a “three-joint muscle,” crossing and capable of effecting movement at the glenohumeral, elbow, and radio-ulnar joints, although it primarily acts at the latter two. The biceps brachii muscle is a powerful flexor of the forearm at the elbow joint; it is also the most powerful supinator of the forearm when the elbow joint is flexed. The brachialis is the main flexor of the forearm. The coracobrachialis helps flex and adduct the arm and stabilize the glenohumeral joint. The only muscle of the posterior compartment of the arm is the triceps brachii muscle. The triceps brachii muscle has three heads: long head, medial and lateral heads. Because its long head crosses the glenohumeral joint, the triceps helps stabilize the adducted glenohumeral joint by serving as a shunt muscle, resisting inferior displacement of the head of the humerus. The long head also aids in extension and adduction of the arm. The medial head is the workhorse of forearm extension. The lateral head is strongest but is recruited into activity primarily against resistance. 7 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES The major artery of the arm, the brachial artery, is found in the anterior compartment. Beginning as a continuation of the axillary artery at the lower border of the teres major muscle, it terminates just distal to the elbow joint, opposite to the neck of the radius where it divides into the radial and ulnar arteries. Branches of the brachial artery in the arm include those to adjacent muscles and two ulnar collateral vessels (superior and inferior ulnar collateral arteries). Additional branches are the profunda brachii artery and nutrient arteries to the humerus.The deep artery of the arm (L. arteria profunda brachii) is the largest branch of the brachial artery. The superficial veins are in the subcutaneous tissue, and the deep veins accompany the arteries. The two main superficial veins of the arm, the cephalic and basilic veins. The cephalic vein ascends in the superficial fascia on the lateral side of the biceps and drains into the axillary vein. Four main nerves pass through the arm: median, ulnar, musculocutaneous, and radial. The musculocutaneous nerve leaves the axilla and enters the arm by passing through the coracobrachialis muscle. It passes diagonally down the arm in the plane between the biceps brachii and brachialis muscles. The musculocutaneous nerve provides: motor innervation to all muscles in the anterior compartment of the arm; and sensory innervation to skin on the lateral surface of the forearm. The median nerve enters the arm from the axilla at the inferior margin of the teres major muscle. It passes vertically down the medial side of the arm in the anterior compartment. The median nerve has no major branches in the arm or in the axilla. Like the median nerve, the ulnar nerve has no branches in the arm, but it also supplies articular branches to the elbow joint. The radial nerve in the arm supplies all the muscles in the posterior compartment of the arm (and forearm). The radial nerve originates from the posterior cord of the brachial plexus and enters the arm by crossing the inferior margin of the teres major muscle. Accompanied by the profunda brachii artery, the radial nerve enters the posterior compartment of the arm by passing through the triangular interval. ANTERIOR ASPECT OF THE FOREARM The forearm is the part of the upper limb between the elbow wrist joints. Proximally, most major structures pass between the arm and forearm through, or in relation to, the cubital fossa, which is anterior to the elbow joint. The exception is the ulnar nerve, which passes posterior to the medial epicondyle of the humerus. Muscles in the anterior compartment of the forearm flex the wrist and digits and pronate the hand. Muscles in the posterior compartment extend the wrist and digits and supinate the hand. Major nerves and vessels supply or pass through each compartment. The flexors and pronators of the forearm in the anterior compartment are served mainly by the median nerve; the one and a half exceptions are innervated by the ulnar nerve. The extensors and supinators of the forearm are in the posterior compartment and are all served by the radial nerve (directly or by its deep branch). Muscles in the anterior (flexor) compartment of the forearm occur in three layers: • Superficial layer (pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris) • Intermediate layer (flexor digitorum superficialis) • Deep layer (flexor digitorum profundus, flexor pollicis longus, and pronator quadratus) Generally, these muscles are associated with: movements of the wrist joint; flexion of the fingers including the thumb; andpronation. The main arteries of the forearm are the ulnar and radial arteries, which usually arise opposite the neck of the radius in the inferior part of the cubital fossa as terminal branches of the brachial artery. The superficial veins of the forearm lie in the superficial fascia. The cephalic vein arises from the lateral side of the dorsal venous arch on the back of the hand and winds around the lateral border of the forearm; it then ascends into the cubital fossa and up the front of the arm on the lateral side of the biceps. It terminates in the axillary vein in the deltopectoral triangle. The basilic vein arises from the medial side of the dorsal venous arch on the back of the hand and winds around the medial border of the forearm; it then ascends into the cubital fossa and up the front of the arm on the medial side of the biceps. Its terminates, by joining the venae comitantes of the brachial artery to form the axillary vein. 8 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES Nerves in the anterior compartment of the forearm are the median and ulnar nerves, and the superficial branch of the radial nerve. The median nerve is the principal nerve of the anterior compartment of the forearm. It supplies muscular branches directly to the muscles of the superficial and intermediate layers of forearm flexors (except the flexor carpi ulnaris), and deep muscles (except for the medial [ulnar] half of the flexor digitorum profundus; ring and little fingers) via its branch, the anterior interosseous nerve. The median nerve has no branches in the arm other than small twigs to the brachial artery. Its major branch in the forearm is the anterior interosseous nerve. Like the median nerve, the ulnar nerve does not give rise to branches during its passage through the arm. In the forearm it supplies only one and a half muscles, the flexor carpi ulnaris muscle (as it enters the forearm by passing between its two heads of proximal attachment) and the ulnar (medial) part (ring and little fingers) of the flexor digitorum profundus muscle. Unlike the medial and ulnar nerves, the radial nerve serves motor and sensory functions in both the arm and the forearm (but only sensory functions in the hand). However, its sensory and motor fibers are distributed in the forearm by two separate branches, the superficial (sensory or cutaneous) and deep radial/posterior interosseous nerve (motor). The lateral cutaneous nerve of the forearm (lateral antebrachial cutaneous nerve) is the continuation of the musculocutaneous nerve after its motor branches have all been given off to the muscles of the anterior compartment of the arm. CUBITAL FOSSA The pronator teres makes the medial border, whereas the brachioradialis makes the lateral border of the cubital fossa. The contents of the cubital fossa are the: • Terminal part of the brachial artery and the commencement of its terminal branches, the radial and ulnar arteries. The brachial artery lies between the biceps tendon and the median nerve. • (Deep) accompanying veins of the arteries • Biceps brachii tendon • Median nerve • Radial nerve POSTERIOR ASPECT OF THE FOREARM Muscles in the posterior compartment of the forearm occur in two layers: a superficial and a deep layer. The muscles are associated with: -movement of the wrist joint; -extension of the fingers and thumb; and -supination. All muscles in the posterior compartment of the forearm are innervated by the radial nerve. The seven muscles in the superficial layer are the brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, and anconeus. The deep layer of the posterior compartment of the forearm consists of five muscles: supinator, abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis. Except for the supinator muscle, all these deep layer muscles originate from the posterior surfaces of the radius, ulna, and interosseous membrane and pass into the thumb and fingers. The blood supply to the posterior compartment of the forearm occurs predominantly through branches of the radial, posterior interosseous, and anterior interosseous arteries. The nerve of the posterior compartment of the forearm is the radial nerve. Most of the muscles are innervated by the deep branch, which originates from the radial nerve in the lateral wall of the cubital fossa deep to the brachioradialis muscle and becomes the posterior interosseous nerve after emerging from between the two heads of the supinator muscle in the posterior compartment of the forearm. 9 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES The deep branch innervates the extensor carpi radialis brevis, then supplies the supinator muscle and then emerges, as the posterior interosseous nerve. The posterior interosseous nerve supplies the remaining muscles in the posterior compartment. ANATOMY OF THE HAND The hand is a mechanical and sensory tool. Many of the features of the upper limb are designed to facilitate positioning the hand in space. The hand is the region of the upper limb distal to the wrist joint. It is subdivided into three parts: • the wrist (carpus); • metacarpus • digits (five fingers including the thumb). There are three groups of bones in the hand: • eight carpal bones are the bones of the wrist; • five metacarpals (I to V) are the bones of the metacarpus; • phalanges are the bones of the digits-the thumb has only two, the rest of the digits have three. The carpal tunnel is formed anteriorly at the wrist by a deep arch formed by the carpal bones and the flexor retinaculum. The base of the carpal arch is formed medially by the pisiform and the hook of the hamate and laterally by the tubercles of the scaphoid and trapezium. The extensor tendons pass into the hand on the medial, lateral, and posterior surfaces of the wrist in six compartments defined by an extensor retinaculum (dorsal carpal ligament) and lined by synovial sheaths. The palmar aponeurosis is a triangular condensation of deep fascia that covers the palm and is anchored to the skin in distal regions. After exiting the carpal tunnel, the tendons of the flexor digitorum superficialis and profundus muscles cross the palm and enter fibrous sheaths on the palmar aspect of the digits. These fibrous sheaths begin proximally, anterior to the metacarpophalangeal joints, and extend to the distal phalanges; are formed by fibrous arches and cruciate (cross-shaped) ligaments and hold the tendons to the bony plane and prevent the tendons from bowing when the digits are flexed. The tendons of the extensor digitorum and extensor pollicis longus muscles pass onto the dorsal aspect of the digits and expand over the proximal phalanges to form complex "extensor hoods" or "dorsal digital expansions". The intrinsic muscles of the hand are the palmaris brevis, interossei (palmar interossei adduct, dorsal interossei abduct the fingers), adductor pollicis, thenar, hypothenar, and lumbrical muscles (participate in flexing the metacarpophalangeal joints and extending the interphalangeal joints). All of the intrinsic muscles of the hand are innervated by the deep branch of the ulnar nerve except for the three thenar and two lateral lumbrical muscles, which are innervated by the median nerve. The blood supply to the hand is by the radial and ulnar arteries, which form two interconnected vascular arches (superficial and deep) in the palm. Vessels to the digits, muscles, and joints originate from the two arches and the parent arteries. The ulnar artery and ulnar nerve enter the hand on the medial side of the wrist. Distally, the ulnar artery swings laterally across the palm, forming the superficial palmar arch. Branches from the superficial palmar arch include: • a palmar digital artery • three large, common palmar digital arteries The radial artery curves around the lateral side of the wrist, passes over the floor of the anatomical snuffbox and into the deep plane of the palm by penetrating anteriorly through the back of the hand. It accesses the deep plane of the palm and forms the deep palmar arch. The deep palmar arch gives rise to: • three palmar metacarpal arteries • three perforating branches 10 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES The cephalic vein originates from the lateral side of the dorsal venous network and passes over the anatomical snuffbox into the forearm. The basilic vein originates from the medial side of the dorsal venous network and passes into the dorsomedial aspect of the forearm. Motor innervation of the hand The hand is supplied by the ulnar, median, and radial nerves. All three nerves contribute to cutaneous or general sensory innervation. The ulnar nerve innervates all intrinsic muscles of the hand except for the three thenar muscles and the two lateral lumbricals, which are innervated by the median nerve. Sensory innervation of the hand Ulnar nerve medial side of the palm, medial half of the dorsum of the hand, the 5th finger, and the medial half of the 4th finger, anterior surfaces of the medial one and a half digits, Median nerve thumb, index, middle fingers, lateral side of the ring [distal parts on the dorsum of the hand] Radial nerve dorsolateral side. CLINICAL ANATOMY OF THE UPPER LIMB (IV. COMMITTEE) Upper Lesions of the Brachial Plexus (Erb-Duchenne Palsy): Upper lesions of the brachial plexus are injuries resulting from excessive displacement of the head to the opposite side and depression of the shoulder on the same side. This causes excessive traction or even tearing of C5 and 6 roots of the plexus. The limb will hang limply by the side, medially rotated by the unopposed sternocostal part of the pectoralis major; the forearm will be pronated because of loss of the action of the biceps. The position of the upper limb in this condition has been likened to that of a porter or waiter hinting for a tip (waiter’s tip position). Lower Lesions of the Brachial Plexus (Klumpke Palsy) injury of the inferior trunk of the brachial plexus Injuries to inferior parts of the brachial plexus (Klumpke paralysis) are much less common. Inferior brachial plexus injuries, usually traction injuries, may occur when the upper limb is suddenly pulled superiorly. The nerve fibers from this segment run in the ulnar and median nerves to supply all the small muscles of the hand. “Clawed hand” Long Thoracic Nerve Injuries: The long thoracic nerve can be injured by blows to or pressure on the posterior triangle of the neck or during the surgical procedure of radical mastectomy. “Winged scapula”. Axillary Nerve Injuries: The axillary nerve can be injured by the pressure of a badly adjusted crutch pressing upward into the armpit. Paralysis of the deltoid and teres minor muscles occurs. Impaired shoulder abduction, shoulder weakness, difficulty in lifting the objects on the side of the injury, difficulty in lifting the arm above the head are among the clinical symptoms in addition to sensory loss in the outer (lateral) part of the arm. Radial Nerve Injuries: The radial nerve is commonly damaged in the axilla and in the spiral groove. Wristdrop, or flexion of the wrist, occurs as a result of the action of the unopposed flexor muscles of the wrist. The deep branch of the radial nerve can be damaged in fractures of the proximal end of the radius or during dislocation of the radial head. Wristdrop will not occur. No sensory loss occurs because this is a motor nerve. Division of the superficial radial nerve results in a variable small area of anesthesia over the dorsum of the hand and the dorsal surface of the roots of the lateral three and a half fingers. The musculocutaneous nerve is rarely injured because of its protected position beneath the biceps brachii muscle. Flexion of the elbow joint and supination of the forearm are greatly weakened but not lost. Weak supination is also still possible. There is also sensory loss along the lateral side of the forearm. Injuries to the Median Nerve at the Elbow: The forearm is kept in the supine position; wrist flexion is weak and is accompanied by adduction. Flexion of the proximal interphalangeal joints of the 1st-3rd digits is lost and flexion of the 4th and 5th digits is weakened. Flexion of the distal interphalangeal joints of the 2nd and 3rd digits is also lost. The ability to flex the metacarpophalangeal joints of the 2nd and 3rd digits is affected. Hand of Benediction (Pope’s Blessing) while trying to make a fist. Ape hand deformity Injuries to the Median Nerve at the Wrist: The muscles of the thenar eminence are paralyzed and wasted so that the eminence becomes flattened. The thumb is laterally rotated and adducted. The hand looks flattened and “ape-like.” At both levels, skin sensation is lost on the lateral half or less of the palm of the 11 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES hand and the palmar aspect of the lateral three and a half fingers. Sensory loss also occurs on the skin of the distal part of the dorsal surfaces of the lateral three and a half fingers. Carpal Tunnel Syndrome is the most common peripheral nerve injury seen in the upper limb. The second most common, the cubital syndrome h is related to the ulnar nerve. The syndrome consists of a burning pain or “pins and needles” along the distribution of the median nerve to the lateral three and a half fingers and weakness of the thenar muscles as well. As would be expected, no paresthesia occurs over the thenar eminence because this area of skin is supplied by the palmar cutaneous branch of the median nerve. The ulnar nerve is most commonly injured at the elbow, where it lies behind the medial epicondyle, and at the wrist, where it lies with the ulnar artery in front of the flexor retinaculum. The injuries at the elbow are usually associated with fractures of the medial epicondyle. Injuries to the Ulnar Nerve at the Elbow (Cubital Tunnel Syndrome): Cubital Tunnel is a fibro-osseus tunnel between the medial epicondyle and flexor carpi ulnaris. The flexion deformity at the interphalangeal joints of the fourth and fifth fingers is obvious because the first and second lumbrical muscles of the index and middle fingers are not paralyzed. In longstanding cases the hand assumes the characteristic “claw” deformity (main en griffe). Wasting of the paralyzed muscles results in flattening of the hypothenar eminence and loss of the convex curve to the medial border of the hand. Examination of the dorsum of the hand will show hollowing between the metacarpal bones caused by wasting of the dorsal interosseous muscles. Loss of skin sensation will be observed over the anterior and posterior surfaces of the medial third of the hand and the medial one and a half fingers. NEUROLOGICAL EXAMINATION- UPPER LIMB To test the deltoid , the arm is abducted, starting from approximately 15°, against resistance. To test the supraspinatus, abduction of the arm is attempted from the fully adducted position against resistance, while the muscle is palpated superior to the spine of the scapula. To test the infraspinatus, the person flexes the elbow and adducts the arm. The arm is then laterally rotated against resistance. To test the function of the suprascapular nerve, which supplies the supraspinatus and infraspinatus, both muscles must be tested as described. The two lateral rotator muscles; the infraspinatus and teres minor are tested together. To test for degenerative tendonitis of the rotator cuff, the person is asked to lower the fully abducted limb slowly and smoothly. From approximately 90° abduction, the limb will suddenly drop to the side in an uncontrolled manner if the rotator cuff (especially the supraspinatus part) is diseased and/or torn.To test the biceps brachii, the elbow joint is flexed against resistance when the forearm is supinated. To test the brachialis, the forearm is semipronated and flexed against resistance. To test the triceps (or to determine the level of a radial nerve lesion), the arm is abducted 90° and then the flexed forearm is extended against resistance provided by the examiner. To test the flexor carpi ulnaris, the person puts the posterior aspect of the forearm and hand on a flat table and is then asked to flex the wrist against resistance. To test the palmaris longus, the wrist is flexed and the pads of the little finger and thumb are tightly pinched together. To test the flexor carpi radialis, the person is asked to flex the wrist against resistance. To test the pronator teres, the person's forearm is flexed at the elbow and pronated from the supine position against resistance provided by the examiner. To test the flexor digitorum superficialis, one finger is flexed at the proximal interphalangeal joint against resistance and the other three fingers are held in an extended position to inactivate the flexor digitorum profundus. To test the flexor digitorum profundus, the proximal interphalangeal joint is held in the extended position while the person attempts to flex the distal interphalangeal joint. The integrity of the median nerve in the proximal forearm can be tested by performing this test using the index finger, and that of the ulnar nerve can be assessed by using the little finger. To test the flexor pollicis longus, the proximal phalanx of the thumb is held and the distal phalanx is flexed against resistance. 12 2013-2014 PHASE I ANATOMY IV. COMMITTEE OVERVIEW PAGES To test the brachioradialis, the elbow joint is flexed against resistance with the forearm in the midprone position.Totest the extensor carpi radialis longus, the wrist is extended and abducted with the forearm pronated.To test the extensor digitorum, the forearm is pronated and the fingers are extended. The person attempts to keep the digits extended at the metacarpophalangeal joints as the examiner exerts pressure on the proximal phalanges by attempting to flex them. To test the extensor carpi ulnaris, the forearm is pronated and the fingers are extended. The extended wrist is then adducted against resistance. To test the extensor digiti minimi, the little finger is extended against resistance while holding digits 2-4 flexed at the metacarpophalangeal joints. To test the abductor pollicis longus, the thumb is abducted against resistance at the metacarpophalangeal joint. To test the extensor pollicis brevis, the thumb is extended against resistance at the metacarpophalangeal joint. To test the extensor pollicis longus, the thumb is extended against resistance at the interphalangeal joint. If the extensor pollicis longus is acting normally, the tendon of the muscle can be seen and palpated on the medial side of the anatomical snuff box. To test the abductor pollicis brevis, abduct the thumb against resistance. To test the flexor pollicis brevis, flex the thumb against resistance. To test the lumbrical muscles, with the palm facing superiorly the patient is asked to flex the metacarpophalangeal joints while keeping the interphalangeal joints extended. The examiner uses one finger to apply resistance along the palmar surface of the proximal phalanx of digits 2-5 individually. To test the dorsal interossei, the examiner holds adjacent extended and adducted fingers between thumb and middle finger, providing resistance as the individual attempts to abduct the fingers (the person is asked to “spread the fingers apart”). To test the palmar interossei, a sheet of paper is placed between adjacent fingers. The individual is asked to “keep the fingers together” to prevent the paper from being pulled away by the examiner. To test the trapezius, the shoulder is shrugged against resistance. To test the latissimus dorsi, the arm is abducted 90° and then adducted against resistance provided by the examiner. To test the rhomboids, the individual places his or her hands posteriorly on the hips and pushes the elbows posteriorly against resistance provided by the examiner. 13