Immune System Notes
advertisement

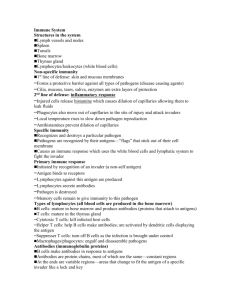
Immune System
Chapter 12
Immune System
• Definition: the body's defense against
infectious organisms and other invaders.
• Through a series of steps called the immune
response, the immune system attacks
organisms and substances that invade body
systems and cause disease
Antibiotics
• Antibiotics are substances or compounds that kill or inhibit the
growth of bacteria by targeting the metabolic pathways of
prokaryotes
• Specific prokaryotic features that may be targeted by antibiotics
include key enzymes, certain ribosomes and the bacterial cell wall
• Because eukaryotic cells do not have these features, antibiotics can
kill bacterial cells without harming humans (or viruses)
• Virus do not carry out metabolic reactions themselves but instead
infect host cells and take over their cellular machinery
• Viruses need to be treated with specific antiviral agents that target
features specific to viruses (e.g. reverse transcriptase in
retroviruses)
Function of the immune system:
– Fight infection through the production of cells that
inactivate foreign substances or cells.
– 2 general categories of defense mechanisms:
• Nonspecific defenses
– Like fortress walls of the system
• Specific defenses
– Work like security guards
Nonspecific Defenses
1st Line of Defense
• Skin
– Protects external structures (outer body areas)
– A dry, thick and tough region made of predominantly
dead surface cells
– Contains biochemical defense agents (sebaceous
glands secrete chemicals which inhibit the growth of
some bacteria)
– The skin also releases acidic secretions to lower pH
and prevent bacteria from growing
Nonspecific Defenses
1st Line of Defense
• Mucous Membranes
– Protect internal structures (externally accessible cavities
and tubes, such as trachea, vagina and urethra)
– A thin region containing living surface cells that release
fluids to wash away pathogens (mucus, tears, saliva, etc.)
– Contains biochemical defense agents (secretions contain
lysozyme, which can destroy cell walls and cause cell lysis)
– Mucous membranes may be ciliated to aid in the removal
of pathogens (along with physical actions such as coughing
or sneezing)
Nonspecific Defense
2nd line of defense
• Inflammatory response- a nonspecific defense
reaction to tissue damage caused by injury or
infection
• White blood cells multiply; blood vessels expand; phagocytes
(WBC) engulf and destroy bacteria
• Fever- elevated body temperature
– Important because many pathogens can survive only within a narrow
temperature range
• Interferon- proteins that help other cells resist
viral infections
• Function: inhibit the synthesis of viral proteins in infected cells and
help block viral replication
Phagocytic Leucocytes
• Phagocytic leucocytes circulate in the blood but may move into
body tissue in response to infection
– White blood cells, specifically neutrophils and macrophages
• They concentrate at sites of infection due to the release of
chemicals (such as histamine) from damaged body cells
• Pathogens are engulfed when cellular extensions (pseudopodia)
surround the pathogen and then fuse, sequestering it in an internal
vesicle
• The vesicle may then fuse with the lysosome to digest the pathogen
• Some of the pathogens antigenic fragments may be presented on
the surface of the macrophage, in order to help stimulate antibody
production
• This mechanism of endocytosis is called phagocytosis ('cell-eating')
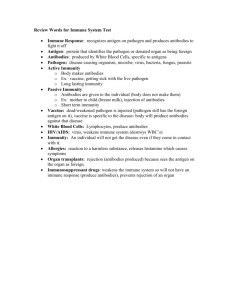
Antigens vs. Antibodies
• Antigen: A substance that the body recognizes as foreign and that
can evoke an immune response
• Antibody: A protein produced by certain white blood cells (B
lymphocytes, plasma cells) in response to an antigen
• Antibodies are made up of 4 polypeptide chains joined together by
disulphide bonds to form a Y-shaped molecule
• The ends of the arms are where the antigens bind and these areas
are called the variable regions, as these will differ between
antibodies
• Each type of antibody will recognize a unique antigenic fragment,
making this interaction specific (like enzyme-substrate interactions)
Specific Defenses
• Used if a pathogen gets past the nonspecific
defenses
– Immune response- series of specific defenses that attack
the particular disease-causing agent
– Cells that recognize specific antigens
• B lymphocytes (B cells)- provide immunity against antigens and
pathogens in the body fluids; called humoral immunity
• T lymphocytes (T cells)- provide defense against abnormal cells
and pathogens inside living cells; called cell-mediated immunity
Humoral Immunity
• Antigens of pathogens are recognized by B cells
• B cells grow and divide producing plasma cells and memory B
cells
• Plasma cells release antibodies- proteins that recognize and
bind to antigens
• Antibodies attack the pathogen in the bloodstream
• Memory B cells remain capable of producing antibodies
specific to that pathogen
• Secondary response is much faster and greatly reduces that
chance that the disease would develop a second time
• Antibody structure has specific binding sites for antigens;
adults can produce about 100 million different types of
antibodies
Cell-Mediated Immunity
• T cells divide and differentiate into killer T cells (cytotoxic Tcells), helper T cells, suppressor T cells, and memory T cells
• Killer T cells track down and destroy the bacteria, fungi,
protozoan, or foreign tissue that contains the antigen
• Helper T cells produce memory T cells
• Memory T cells will cause a secondary response if the same
antigen enters the body again
• Suppressor T cells release substances that shut down the killer
T cells
• Rejection is a process in which an organ is recognized as a
foreign object and is attacked by the immune system
Antibody Production
• B lymphocytes (B cells) are antibody-producing cells that
develop in the bone marrow to produce a highly specific
antibody that recognizes one type of antigen
• When wandering macrophages encounter a pathogen, they
digest it and present the antigenic fragments on their
surface to helper T lymphocytes (T cells)
• These cells activate the appropriate B cell which divides
and differentiates into short-lived plasma cells that produce
massive quantities of antibody (~2,000 molecules per
second for ~4 - 5 days)
• A small proportion of B cell clones develop into memory
cells, which may survive for years providing long-term
immunity
Blood Clotting
• Clotting (haemostasis) is a mechanism that
prevents the loss of blood from broken vessels
• Damaged cells and platelets release chemical
signals called clotting factors which trigger a
coagulation cascade:
• Clotting factors also cause platelets to become
sticky, which then adhere to the damaged region
to form a solid plug called a clot
• The clot prevents further blood loss and blocks
entry to foreign pathogens
Challenge and Response
• When the body is challenged by a foreign pathogen it
will respond with both a non-specific and specific
immune reaction
• The body is capable of recognizing invaders as they do
not possess the molecular markers that designated all
body cells as 'self'
• Non-specific immune cells (macrophages) present the
foreign antigens to lymphocytes as examples of 'nonself'
• These lymphocytes can then respond with the
production of antibodies to destroy the foreign
invaders
Clonal Selection
• Each B lymphocyte has a specific antibody on its
surface that is capable of recognizing a specific antigen
• When antigens are presented to B cells (and T cells) by
macrophages, only the B cell with the appropriate
antibody will become activated and clone
• The majority of B cell clones will differentiate into
antibody-producing plasma cells, a minority will
become memory B cells (BM cells)
• Because pathogens may contain several antigenic
determinants, several B cell clones may become
activated
Memory Cells
• Because the adaptive immune response is dependent on clonal
expansion to create sufficiently large amounts of antibodies, there
is a delay between initial exposure and the production of antibodies
• When a B cell does divide and differentiate into antibody-secreting
plasma cells, a small proportion of clones will differentiate into
memory cells
• Memory cells remain in the body for years (or even a lifetime)
• If a second infection with the same antigen occurs, the memory
cells react faster and more vigorously than the initial immune
response, such that the symptoms of the infection do not normally
appear
• Because the individual no longer presents with the symptoms of
infection upon exposure, the individual is thus said to be immune
Antibody Production
• Antigens stimulate an immune response via the production of
antibodies
• When a pathogen invades the body, it is engulfed by wandering
macrophages which present the antigenic fragments on its surface
• This macrophage becomes an antigen-presenting cell, and presents
the antigen to helper T cells (TH cells)
• The TH cells bind to the antigen and become activated, and in turn
activate the B cell with the specific antibody for the antigen
• This B cell clones and differentiates into plasma cells and memory
cells
• The plasma cells produce high quantities of specific antibody to the
antigen, whereas memory cells survive in the bloodstream for years
• Upon re-exposure to the antigen, memory cells initiate a faster and
stronger response and thus confer long-term immunity
Monoclonal Antibodies
• Monoclonal antibodies (mAb) are antibodies
derived from a single B cell clone
• An animal (typically a mouse) is injected with an
antigen and produces specific plasma cells
• The plasma cells are removed and fused
(hybridised) with tumor cells capable of endless
divisions (immortal cell line)
• The resulting hybridoma is capable of
synthesising large quantities of specific antigen,
for use in diagnosis and treatment
Diagnostic Use
• Monoclonal antibodies can be used to test for pregnancy
via the presence of human chorionic gonadotrophin (hCG)
• An antibody specific to hCG is made and is tagged to an
indicator molecule (e.g. chromatophore or pigment
molecule)
• When hCG is present in the urine it binds to the anti-hCG
monoclonal antibody and this complex will move with the
fluid until it reaches a second group of fixed antibodies
• When the complex binds to the fixed antibodies, they will
appear as a blue line (positive result) due to the presence
of the indicator molecule
Treatment Use
• Monoclonal antibodies can be used for the
emergency treatment of rabies
• Because the rabies virus is potentially fatal in
non-vaccinated individuals, injecting purified
quantities of antibody is an effective
emergency treatment for a very serious viral
infection
Acquired Immunity
• Edward Jenner made observations of cowpox and smallpox
infections; infected a boy with cowpox; watched the reaction
take place; infected him with smallpox; no development of
disease
• Active immunity- type of immunity produced by the body’s
reaction to a vaccine
– More than 20 serious diseases can be prevented through vaccinations
• Passive Immunity- short-term immunity caused when
antibodies produced by other animals for a pathogen are
injected into the body
– Natural immunity example- mother to fetus
– Deliberate exposure example- travelers to other countries or rabies
Vaccination
• Vaccinations induce artificial active immunity by stimulating the
production of memory cells
• A vaccine contains weakened or attenuated forms of the pathogen
and is (usually) injected into the bloodstream
• Because a modified form of the pathogen is injected, the individual
should not develop disease symptoms
• The body responds to the vaccine by initiating a primary immune
response, resulting in the production of memory cells
• When exposed to the actual pathogen, the memory cells trigger a
secondary immune response that is much faster and stronger
• Vaccines confer long-term immunity, however because memory
cells may not survive a life time, booster shots may be required
Benefits of Vaccinations
• Vaccination results in active immunity
• It can limit the spread of infectious diseases
(pandemics / epidemics)
• Diseases may be eradicated entirely (e.g. smallpox)
• Vaccination programs may reduce the mortality rate of
a disease as well as protect vulnerable groups (e.g.
youth, elderly)
• Vaccinations will decrease the crippling effects of
certain diseases (e.g. polio)
• It will decrease health care costs associated with
treating disease conditions
Risks of Vaccinations
• Vaccinated individuals may produce (mild)
symptoms of the disease
• There may be human error in the preparation,
storage or administration of the vaccine
• Individuals may react badly to vaccines (e.g.
hypersensitive / allergic reactions)
• Immunity may not be life long - booster shots
may be required
• There may be possible toxic effects of mercurybased preservatives used in vaccines