6.3 Notes - rufuskingscience
advertisement

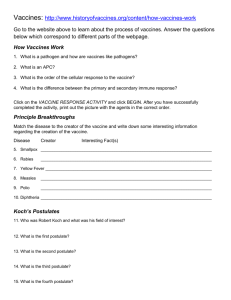
6.3 Defense Against Infectious Disease The human body has structures and processes that resist the continuous threat of invasion by pathogens. Q: What is a pathogen? Bacteria • Prokaryotes (no real nucleus) • Divide by binary fission Can cause: • Food poisoning (e.g. Salmonella) • Ear and eye infections http://en.wikipedia.org/wiki/File:Ericson_Type • Cholera, diarrhea _II_Conjunctivitis.JPG Viruses • Acellular (non-living?) • Need a ‘host’ cell to carry out functions of life, including reproduction • Can have DNA or RNA • Mutate, evolve and recombine quickly Cause: • Flu, HIV/AIDS, smallpox, measles, common cold, herpes, ebola The 1918 flu epidemic killed between 50 and 130 million people. http://en.wikipedia.org/wiki/1918_flu_pandemic Fungi • Eukaryotes, reproduce with spores Cause: • Athlete’s foot, mould, ringworm • Allergic reactions and respiratory problems Image from: http://en.wikipedia.org/wiki/Athlete's_foot Protozoa • Simple parasites Cause: • Malaria • Leishmaniasis • Toxoplasmosis Leishmaniasis image from: http://en.wikipedia.org/wiki/Leishmaniasis The skin and mucous membranes form a primary defence against pathogens that cause infectious disease. Q: What parts of the body have mucous membranes? Q: List two characteristics of mucous membranes that help them defend against pathogens. Cuts in the skin are sealed by blood clotting. Q: In numbered steps, explain how clotting occurs. • Clotting factors are released from platelets. • An enzyme called thrombin is produced. • Thrombin converts soluble fibrinogen to insoluble fibrin. • Fibrin forms a mesh that traps red blood cells. • The gel, if exposed to air, hardens into a scab. Application: Causes and consequences of blood clot formation in coronary arteries. CAUSES CONSEQUENCES Well known factors correlated with an increased risk of blood clot formation in coronary arteries. • Smoking • High blood cholesterol concentration • High blood pressure • Diabetes • Obesity • Lack of exercise If the coronary arteries become blocked by a blood clot: • Part of the heart is deprived of O2 and nutrients • Cardiac muscle cells can not produce ATP • Contractions become irregular and uncoordinated • Fibrillation • Heart does not pump blood effectively Review atherosclerosis Ingestion of pathogens by phago cytic white blood cells gives non-specific immunity to diseases. (“eating”) (“cell”) Q: Draw the process of phagocytosis. Why is this “non-specific immunity”? • Chemotaxis (movement in response to chemicals) attracts the phagocytes to the area of invasion as response to: • proteins produced by the pathogen • phospholipids released by damaged cells • The phagocyte attaches to the pathogen’s cell surface proteins and then engulfs it. The fluid nature of the plasma membrane allows this to happen. • A phagosome forms. This is a vesicle that contains the pathogen. Lysosomes – vesicles of digestive enzymes – deposit the enzymes into the phagosome. • The digestive enzymes break down the pathogen and the waste products are expelled from the cell by exocytosis. Q: Why do infected wounds become pus-filled? Phagocytic Leucocytes card sort game: order the images & outline the processes Images from: http://highered.mcgraw-hill.com/sites/0072495855/student_view0/chapter2/animation__phagocytosis.html Q: What is a lymphocyte? Q: What is an antibody? • Production of antibodies by lymphocytes in response to particular pathogens gives specific immunity. Some lymphocytes act as memory cells and can quickly reproduce to form a clone of plasma cells if a pathogen carrying a specific antigen is re-encountered. Q: Why does it take a couple of days for your body to be able to fight off a disease? Antibiotics block processes that occur in prokaryotic cells but not in eukaryotic cells. Q: List four processes in prokaryotes that are blocked by antibiotics. Viruses lack a metabolism and cannot therefore be treated with antibiotics. Antibiotics are ineffective against viruses! Analyse the graph below. Over time, outline what has happened to: • The number of new approved antibiotics • The diversity of new approved antibiotics Some strains of bacteria have evolved with genes that confer resistance to antibiotics and some strains of bacteria have multiple resistance. Q: List three measures that can be taken to reduce the development of antibiotic resistance in bacteria. Nature of science: Risks associated with scientific research— Florey and Chain’s tests on the safety of penicillin would not be compliant with current protocol on testing. • Application: Florey and Chain’s experiments to test penicillin on bacterial infections in mice. • They tested the drug on humans after only a very brief period of animal testing…. • How brief? • 8 mice. • There could have been severe side effects. • The samples they were using were not pure. • The patients they used were all at the point of death and several were cured. • Penicillin was introduced more quickly than it should have been, in time for the D-Day invasion and the number of soldier deaths was greatly reduced. Application: An understanding of immunity has led to the development of vaccinations. • LIVE, ATTENUATED VACCINES • Live, attenuated vaccines contain a version of the living microbe that has been weakened in the lab so it can’t cause disease. • Because a live, attenuated vaccine is the closest thing to a natural infection, these vaccines are good “teachers” of the immune system: They elicit strong cellular and antibody responses and often confer lifelong immunity with only one or two doses. • Vaccines against measles, mumps, and chickenpox, for example, are made by this method. Viruses are simple microbes containing a small number of genes, and scientists can therefore more readily control their characteristics. Application: An understanding of immunity has led to the development of vaccinations. • INACTIVATED VACCINES • Scientists produce inactivated vaccines by killing the diseasecausing microbe with chemicals, heat, or radiation. • Such vaccines are more stable and safer than live vaccines: The dead microbes can’t mutate back to their disease-causing state. Inactivated vaccines usually don’t require refrigeration, and they can be easily stored and transported in a freeze-dried form, which makes them accessible to people in developing countries. • Most inactivated vaccines, however, stimulate a weaker immune system response than do live vaccines. • So it would likely take several additional doses, or booster shots, to maintain a person’s immunity. This could be a drawback in areas where people don’t have regular access to health care and can’t get booster shots on time. Application: An understanding of immunity has led to the development of vaccinations. • SUBUNIT VACCINES • Instead of the entire microbe, subunit vaccines include only the antigens that best stimulate the immune system. • In some cases, these vaccines use epitopes—the very specific parts of the antigen that antibodies or T cells recognize and bind to. • Because subunit vaccines contain only the essential antigens and not all the other molecules that make up the microbe, the chances of adverse reactions to the vaccine are lower. • A recombinant subunit vaccine has been made for the hepatitis B virus. – Scientists inserted hepatitis B genes that code for important antigens into common baker’s yeast. – The yeast then produced the antigens, which the scientists collected and purified for use in the vaccine. – Research is continuing on a recombinant subunit vaccine against hepatitis C virus. Application: An understanding of immunity has led to the development of vaccinations. • TOXOID VACCINES • For bacteria that secrete toxins, or harmful chemicals, a toxoid vaccine might be the answer. These vaccines are used when a bacterial toxin is the main cause of illness. • Scientists have found that they can inactivate toxins by treating them with formalin, a solution of formaldehyde and sterilized water. Such “detoxified” toxins, called toxoids, are safe for use in vaccines. • When the immune system receives a vaccine containing a harmless toxoid, it learns how to fight off the natural toxin. The immune system produces antibodies that lock onto and block the toxin. • Vaccines against diphtheria and tetanus are examples of toxoid vaccines. Application: An understanding of immunity has led to the development of vaccinations. • CONJUGATE VACCINES • If a bacterium possesses an outer coating of sugar molecules called polysaccharides, as many harmful bacteria do, researchers may try making a conjugate vaccine for it. • Polysaccharide coatings disguise a bacterium’s antigens so that the immature immune systems of infants and younger children can’t recognize or respond to them. Conjugate vaccines, a special type of subunit vaccine, get around this problem. • When making a conjugate vaccine, scientists link antigens or toxoids from a microbe that an infant’s immune system can recognize to the polysaccharides. The linkage helps the immature immune system react to polysaccharide coatings and defend against the disease-causing bacterium. • The vaccine that protects against Haemophilus influenzae type B (Hib) is a conjugate vaccine. Application: An understanding of immunity has led to the development of vaccinations. • • • • • • DNA VACCINES Still in the experimental stages, these vaccines show great promise, and several types are being tested in humans. DNA vaccines take immunization to a new technological level. These vaccines dispense with both the whole organism and its parts and get right down to the essentials: the microbe’s genetic material. In particular, DNA vaccines use the genes that code for those all-important antigens. A DNA vaccine against a microbe would evoke a strong antibody response to the free-floating antigen secreted by cells, and the vaccine also would stimulate a strong cellular response against the microbial antigens displayed on cell surfaces. The DNA vaccine couldn’t cause the disease because it wouldn’t contain the microbe, just copies of a few of its genes. In addition, DNA vaccines are relatively easy and inexpensive to design and produce. So-called naked DNA vaccines consist of DNA that is administered directly into the body. These vaccines can be administered with a needle and syringe or with a needle-less device that uses highpressure gas to shoot microscopic gold particles coated with DNA directly into cells. Sometimes, the DNA is mixed with molecules that facilitate its uptake by the body’s cells. Naked DNA vaccines being tested in humans include those against the viruses that cause influenza and herpes. Application: An understanding of immunity has led to the development of vaccinations. • • • • • RECOMBINANT VECTOR VACCINES Recombinant vector vaccines are experimental vaccines similar to DNA vaccines, but they use an attenuated virus or bacterium to introduce microbial DNA to cells of the body. “Vector” refers to the virus or bacterium used as the carrier. In nature, viruses latch on to cells and inject their genetic material into them. In the lab, scientists have taken advantage of this process. They have figured out how to take the roomy genomes of certain harmless or attenuated viruses and insert portions of the genetic material from other microbes into them. The carrier viruses then ferry that microbial DNA to cells. Recombinant vector vaccines closely mimic a natural infection and therefore do a good job of stimulating the immune system. Attenuated bacteria also can be used as vectors. In this case, the inserted genetic material causes the bacteria to display the antigens of other microbes on its surface. In effect, the harmless bacterium mimics a harmful microbe, provoking an immune response. Researchers are working on both bacterial and viral-based recombinant vector vaccines for HIV, rabies, and measles. Application: Effects of HIV on the immune system (a reduction in the number of active lymphocytes and a loss of the ability to produce antibodies, leading to the development of AIDS) and methods of transmission.