Fluid & Electrolyte Therapy Acid
advertisement

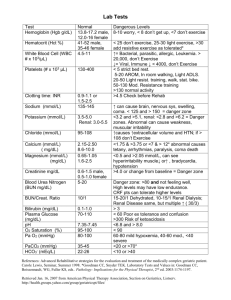
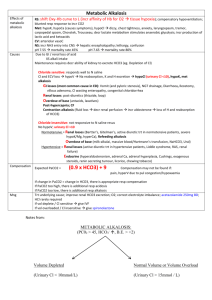
• ACID – BASE BALANCE: • Normal total body A-B balance is when the arterial pH is between 7.35 - 7.45 • Large amounts of acid are added to the body daily mainly in the form of CO2, by: a) cellular metabolism, b) energy generation, & c) protein metabolism *Some H ions & weak organic & inorganic nonvolatile acids also are generated. • The pCO2 is maintained within the normal range because CO2 generated is continuously diffused & eliminated across the lungs. • The kidneys maintain serum[HCO3] within normal by: a) reabsorbing HCO3 ions from the glomerular filtrate & b) by generating new HCO3 ions in renal tubular cells. • Acid-base disturbances are caused by serum [CO2] or [HCO3] changes. • If the problem originates with CO2→ pH change is of resp. origin. • If it begins with HCO3 → pH change is of metabolic origin. • Plasma pH < 7.35 →acidosis ( respiratory or metabolic ) • plasma pH >7.45 →alkalosis (respiratory or metabolic) • When plasma pH goes outside the normal range → lungs & kidneys act to compensate & normalize the pH value. • • • • PRIMARY ACID-BASE DISTURBANCES METABOLIC ACIDOSIS plasma pH < 7.35 as a result of a low blood [HCO3] Possible Causes: 1. losses from the body, 2. ↓’d renal regeneration of HCO3, 3. ↑’d amounts of acid added to the body by ingestion or metabolic processes. * As the [HCO3] ↓→ lungs try to ↓ pCO2 & maintain normal pH by ↑’ing depth & rate of respiration • SxS of metabolic acidosis are clinically sig. @ pH ≤ 7.1 • # of (+) charged ions in body must always = # of ( - ) charged ions * Electrical neutrality in plasma is achieved by dissolved electrolytes & proteins Na = Cl + HCO3 + Unmeasured anions *Unmeasured ions: plasma proteins & small amounts of SO4 & PO4 not measured by tests in clinical labs • The usual amounts of these anions in the blood have a combined ionic strength of 8-16 mmol/L (8-16 mEq/L). • This value is called the anion gap, & it rarely changes. • Assuming that Na remains constant, a change in the number of any one of the anions necessitates a change in one or both of the others to maintain electrical neutrality. • Because the # of unmeasured anions is fixed, the Cl & HCO3 are alterable. • Metabolic Acidosis: A) Nonanion Gap Metabolic Acidosis: • The # of unmeasured anions is the same as usual, & so ↓’d [HCO3] may be due to: *Cl loading (NS infusion, NaCl overload) *actual HCO3 loss from the body (prolonged diarrhea) Or *↓’d HCO3 generation (renal failure) • Important to determine which type of Metabolic Acidosis before Tx is started. • Treatment of Nonanion Gap Met. Acidosis: 1. Correct underlying cause 2. Replace HCO3 deficit ** The kidneys generate sufficient HCO3 & normalize pH when acidosis cause is corrected, EXCEPT in Renal Failure or profound & continuous GI loss. • Acute HCO3 replacement is needed only when: 1. pH ≤ 7.1 or 2. Life-threatening SxS of acidosis • Amount of HCO3 deficit: • HCO3 deficit (mmol)= [24-Measured HCO3(mmol/L)]Xbody wt(kg)X 0.5 • ½ the calculated dose is given → (usually↑pH by 0.2) • Goal of emergency HCO3 replacement: to correct existing cardiac or CNS disturbances by reaching pH ≥ 7.2 * Because acidosis onset is gradual → CNS is slowly equilibrated to low pH→ Rapid changes in plasma pH relative to CNS pH → may cause seizures & death because CNS pH may lag behind • In addition to the risk of alkalosis & hypernatremia with rapid replacement with NaHCO3 • In Renal Failure: • Due to the ↓’d ability of damaged kidneys to generate HCO3 → Nonanion gap metabolic acidosis is usually chronic, mild & asymptomatic • With severe renal failure → severe acidosis → Require hemodialysis • If diarrheal losses > ability of kidneys to generate HCO3 → HCO3 must be given (Na or K Bicarbonate or Acetate) *Composition of the fluid lost must be determined by lab * Amount of base given must be enough to: a. correct initial deficit & b. maintain the daily loss B. Anion Gap Metabolic Acidosis: • ↑# of unmeasured anions (nonvolatile acids) in plasma →↓[HCO3] to maintain electrical neutrality • Possible causes (Abnormal metabolic processes): 1. Diabetic ketoacidosis 2. Prolonged starvation 3. Hypoxia→ lactic acidosis 4. Anaerobic carbohydrate metabolism 5. Accumulation of ingested acids (salicylate/methanol poisoning) 6. Normally produced acid in the body that can not be eliminated • Treatment of Anion-Gap Met. Acidosis: 1. Correct underlying cause e.g. Diabetes → IV insulin lactic acidosis → restoration of app. circulating vol. or plasma O2 carrying capacity poisoning → hemodialysis or gastric lavage 2. HCO3 Tx → *reserved for pH < 7.1 or *severe SxS of acidosis • • • • Metabolic Alkalosis: Plasma pH > 7.45 by ↑’d blood [HCO3] Anion gap: Never affected Lungs compensate by↓’ing resp. depth & rate to ↑ pCO2 & normalize pH • Significant SxS seen @ pH≥ 7.6 • Most Common Causes: 1. Cl ion loss (NG suction, loop diuretics, mineralcorticoid excess→Na retention with K & H loss) 2. ECF depletion (↑[HCO3]→contraction alkalosis) 3. Hepatic failure → 2⁰Hyperaldosteronism → K & H losses • Treatment of Metabolic Alkalosis: 1. From Volume Depletion: NS →Tx of Choice: • Na & Cl loss & ↑HCO3 with volume contraction → Saline Responsive • NS: a)Replaces Na →stops aldost.-stimulated exchange of H & Na in renal tubules b)Replaces Cl →stops generation of HCO3 needed for elect. neutrality c)Vol. expansion →↓[HCO3] in vascular space 2) Met. Alk. associated with TBW overload (i.e. in hepatic failure) →can NOT tolerate NS Tx →IV infusion of HCl acid *Dosage HCl to replace H & Cl deficit: HCl (mmol) = [103 - Measured Cl (mmol/L)] Xbody wt(kg) X 0.2 *Give ½ HCl deficit IV over 12-24 hrs → ↓pH by 0.2 *This should not cause CNS pH gradient * IV infusion in central venous catheter NOT peripheral → ↓phlebitis risk 3) Metabolic alk. From Hypokalemia 2⁰ to ICF/ECF exchange of H for K & mineralcorticoid excess→ Saline resistant →Treatment: Potassium Replacement 4) Met. Alk. Caused by ↓’d aldosterone degradation (i.e., in hepatic failure) →Treatment: Spironolactone 5) Mineralcorticoid-producing tumors of adrenal/pit. gland →Treatment: Aminoglutethamide or surgery • Respiratory Acidosis: • Plasma pH < 7.35 from pCO2 > 40mmHg • Slow HCO3 generation in kidney→↑[HCO3] → Normalize plasma pH • CO2 excretion capacity of normal lungs → always > metabolic production of CO2 → Resp. Acidosis only results from severe pulmonary disease • Treatment of Respiratory Acidosis: 1) Correcting underlying Pulm. Dz. (i.e. Antibiotics, broncodilators, steroids) 2) Intubation & mechanical ventilation if resp. depression **Avoid rapid correction of pH 3) HCO3: ONLY if pH≤7.1 4) Chronic Respiratory Acidosis with COPD: develops slowly & rarely requires Tx ( many adapt) Acute in ↓ pCO2 &↑pO2 →Not recommended due to risk of apnea • Respiratory Alkalosis: • Plasma pH >7.45 from pCO2< 40mmHg • Possible Causes: 1) Voluntary hyperventilation 2) Respiratory Stimulants & mechanical vent. 3) Hypoxemia → ↑ RR →↓pCO2 • Treatment of Respiratory Alkalosis: • Correct disorder→↑[CO2] of inspired air by: 1. ↑inspired CO2 by a ventilator Or 2. Rebreathe pt’s own expired air (bag placed loosely over nose & mouth) • Compensatory Responses to A/B disturbances: • All 1⁰ A/B disturb. → compensatory response. • May be difficult to determine 1⁰ if plasma pH is within normal • Two 1⁰ A/B problems can occur together EXCEPT Resp. acidosis & Resp. Alkalosis • Correct diagnosis with pt’s hx are important for starting therapy • Electrolytes ( Cont.): • POTASSIUM (3.5-5 mEq/L), (3.5-5.0 mmol/L): • Changes in acid-base status alter the distribution of K+ in the body. • Serum [K] ↑’s with acidosis or ↓’s with alkalosis by 0.6 mEq/L for every 0.1 change in pH from 7.4. • Hyperkalemia: • may be a medical emergency manifesting as sudden cardiac arrhythmias usually @ serum [K+] > 6 mEq/L. • Treatment of Hyperkalemia: • Any exogenous sources of K i.e., IV fluids or drugs that contain K should be discontinued immediately. • Measures used to correct hyperkalemia act by: a) normalizing neuromuscular membrane potential, b) shifting ions back into the intracellular space, c) removing K from the body. a) If the K-induced arrhythmia is life threatening: *Give 2.5-5 mmol (5 to 10 mEq) Calcium over several minutes to temporarily correct the K:Ca ratio & eliminate the cardiac problem. *A constant IV infusion of Ca @ a rate determined by simultaneous ECG monitoring may be necessary to maintain cardiac function until measures that permanently normalize serum [K] take effect. • Ca gluconate (2.3 mmol/g) or Ca Cl (6.8 mmol/g) is used • Therapy cannot be continued for long periods because hypercalcemia may occur. b) Shifting of K from ECF→ ICF through adm. of : *Glucose & insulin: Potassium ions move with glucose across cell membranes in the presence of insulin. • 2 – 3 g glucose/ unit of insulin is needed to maintain a normal [BG] • E.g., administered solutions include 25 - 30 U of R insulin/ L of 10% dextrose solution • Or 10 units in 50 mL 50% dextrose. *Beta 2-agonists : A total of 10 - 20 mg of albuterol may be adm. by nebulizer, in combination with glucose &insulin. * NaHCO3 : A temporary alkalosis is caused, • Recommended in combination with insulin & glucose because of its poor efficacy when used alone • Cannot be continued for long periods because Na overload & metabolic alkalosis may occur. • All these are temporary because they do NOT remove K from the body • 3 Different treatments may be used to remove K from the body: • Should be initiated as soon as possible, • They may not correct cardiac arrhythmias soon enough • Not considered acute treatment for hyperkalemia. 1) Cationic-anionic exchange resin Na polystyrene sulfonate (SPS): *po or rectally ( po preferred due to longer contact time with GI mucosa) *Binds K to itself through exchange with Na in GI tract (may cause Na overload). * 1Gm of SPS removes ~ 1mmol K & adds 2-3 mmol Na. *Very constipating, so it is given with sorbitol, an osmotic cathartic, & water to prevent fecal impaction. *The initial dosage : 30-60 g resin in 20% sorbitol & can be repeated Q 1- 2 hrs if the serum [K] remains high. 2)Loop diuretics,(furosemide): • Have been used as Tx for pts. with hyperkalemia 3)Hemodialysis: • Can be used to remove K from the body. • Immediate but very invasive • Should be used only when the patient’s condition is life threatening & other Tx methods have failed. • Hypokalemia: • Can also be a cardiac medical emergency, with rhythm disturbances appearing at serum [K] < 3 mEq/ L. . • Correction of underlying dz. or discontinuation of drug therapy that contributes to hypokalemia is a basic part of the initial Tx. * Hypokalemia 2⁰ to hyponatremia is almost always accompanied by hypochloremic alkalosis. * Renal reabsorption of Na→ K & H ions secretion * The dissociation of Carbonic acid in renal tubular cells → H & HCO3. * The H ion needed for exchange with Na is secreted into the urine, & HCO3 is resorbed into the blood. * HCO3 accumulation in serum → alkalosis * Any concomitant hyponatremia & alkalosis must be corrected for hypokalemia Tx to be successful. * KCl salt : The Tx of choice because alkalosis must be corrected. • Cl loading → ↑’s elimination & ↓’s generation of HCO3 by the kidneys → alkalosis resolves. • If a nonchloride salt of K is used → hypokalemia will not be corrected . • Treatment of Hypokalemia: • ICF deficit of K almost always precedes & accompanies an ECF deficit → requires large amounts of K • po or IV K shifts slowly into the ICF to correct that deficit → slow IV infusion of KCl to avoid hyperkalemia. • IV KCl @ 10 mEq/ hr in pts with serum [K] < 3.5 mEq/ L, & 30-40 mEq given over 3- 4 hrs in D5W or NS is a common rate of K replacement. • Serum [K] should be reassessed & K administered until normal (3.8 to 4.0 mEq/L). • In profound hypokalemia & continued K wasting, replacing K deficit may need to be given in very large doses → 20 - 40 mEq/ hr given centrally to avoid pain & phlebitis @ infusion site. • Oral administration of potassium chloride can cause GI irritation → IV replacement may be needed for large K • CHLORIDE:(95-105 mmol/L) • Major anion in the ECF, • It usually ↑’s or ↓’s with total body sodium, • A change in [Cl] → acid-base disturbance. *Hyperchloremia: • Results from: *metabolic acidosis, *respiratory alkalosis, * hypernatremia, or *Cl loading. • Treatment: • Correcting the underlying disorder. • If the cause is metabolic acidosis or respiratory alkalosis → correcting them is the only Tx. • Changing NS infusion to 0.45% saline infusion or replacing NaCl with Na acetate may resolve it. • If caused by overingestion of NaCl → Tx :free H2O replacement & diuresis. * In hypernatremia caused by H2O loss → Tx: TBW fluid replacement • • • • Hypochloremia: Hyponatremia → hypochloremia (to maintain electrical neutrality); Cl normalizes with correction of the ECF [Na] Most common causes: *NG suction, *vomiting, *diuretic therapy. • Treatment: • Replacing with high-Cl solutions i.e., NS or LR. • Liberalizing sodium chloride intake, reducing the diuretic dose, & correcting symptomatic hyponatremia and hypokalemia with saline and KCL solutions. • • • • CALCIUM: (8.8-10.3 mg/dL or 2.2- 2.6 mmol/L ) Only 1% of the total is in the fluid spaces. 50% is protein bound PTH, vit. D, & calcitonin regulates GI absorption, renal excretion, & skeletal deposition or resorption of Ca & determine its serum [Ca] • An inverse relationship occurs between serum [Ca] & [PO4] • Corrected, measured total serum Ca can be calculated by accounting for a patient’s ↓’d albumin on the basis of a normal value of 4 g/dL. Corrected serum Ca = [4 g/dL - Measured albumin(g/dL)] X 0.8 + Serum calcium measured • Either monitor the reported ionized Ca or the corrected measured total serum Ca • Acid-base disturbances affect the ionized:bound Ca ratio but not the total serum Ca. • In acidosis, hydrogen ions displaces Ca ions from their protein binding sites, & ↑’s free Ca in the blood. • The converse is true in alkalosis. • For each 0.1 change in pH, the ionized Ca changes by 0.42 mmol/ L in the opposite direction. • Hypercalcemia: (corrected total serum Ca > 2.6 mmol/L (10.3 mg/dL) or ionized Ca > 1.15 mmol/L). • *Any sources of exogenous Ca should be discontinued immediately. • Treatment: • 1) Shifting Ca ions into the bone • Or 2) Eliminating Ca from the body. 1) Therapies administered to remove Ca from the body are given first because they work faster & are generally more effective in acute situation. • Loop diuretics, such as furosemide and bumetanide, ↑ renal Ca excretion. • The initial furosemide dosage is 1mg/ kg & is given with of NS to maintain normal body H2O & [Na] • Electrolytes must be carefully monitored & K & Mg administration may be needed to prevent hypokalemia & hypomagnesemia . • This washout therapy may need to be continued for extended periods if the cause of the hypercalcemia is severe or if abnormally large amounts of Ca continue to appear in the vascular compartment. 2) • • • • • • • • • • • • • • • Treatments that shift Ca back into bone are slow & may become ineffective because of tachyphylaxis. Parenteral Calcitonin: Rapidly ↑’s bone uptake of Ca Rapid onset but short duration, and tachyphylaxis develops within days. The initial parenteral dose 4 IU/ kg Q 12 hrs SQ or IM . Etidronate disodium: a bisphosphonate that inhibits osteoclastic bone resorption by binding hydroxyapatite. Initial treatment 7.5 mg/kg/day IV QD X 3days The infusion time: @ least 2 hrs to avoid renal damage (renal disease) Once serum [Ca] is normalized, po therapy 20 mg/kg/d Pamidronate disodium: May be > effective than etidronate Faster onset & longer duration of action than etidronate Dose: 60-90 mg given IV over @ least 2 hrs. May be repeated as often as every 7 days if needed Calcitonin in combination with bisphosphonates is used in the acute management of hypercalcemia. • • • • • Steroids i.e. prednisone: useful in managing chronic mild hypercalcemia. Initial prednisone dose15-100 mg/d Onset of action 3-10 days. Steroids antagonize activation of vit.D in the liver & reduce bone resorption. • For these reasons, steroids are not effective in hypercalcemia secondary to hyperparathyroidism • Oral phosphate: • Not Tx option in this type of hypercalcemia because the amount of serum Ca falls when [P] rises usually is small & because of the risk of soft tissue calcification exceed benefit of this therapy. • Mithramycin: • Cancer chemotherapeutic agent that acts by inhibiting DNA-dependent bone osteoclast RNA synthesis → slows or stops bone resorption. • An effective but potentially toxic therapy for hypercalcemia • Indicated only when other therapies fail. • Doses smaller than those used in cancer but hematologic & GI toxicity remain • OA 12-48 hrs, DA 3-7 days • Hypocalcemia: Corrected [Ca] < 8.8 mg/dL (2.20 mmol/L) or an ionized [Ca] <1 mmol/L. • • • • Acute Tx: IV Ca. Ca chloride contains 6.8mmol/gm (13.5 mEq Ca/gm), Ca gluconate & gluceptate 2.3 mmol/gm (4.6 mEq Ca/gm) The initial dose 2.5-5 mmol Ca followed by an infusion of 0.075-0.1 mmol Ca/kg/hr • Monitor [Ca], BP, & ECG • If hypocalcemia SxS do not resolve, evaluate for hypomagnesemia • Treatment of Chronic hypocalcemia: • Correct the underlying cause. • Mostly, the cause of chronic hypocalcemia is a low concentration of biologically active vit. D in advanced hepatic or renal dz. because of ↓’d transformation of cholecalciferol (D3) → active 1,25dihydroxycholecalciferol (1,25-DHC). • The serum [Ca] will not normalize until conc. of 1,25-DHC is normal. • • • • • Therapy: Ca & vit. D supplements. Ergocalciferol (D2) 1.25-5 mg (50,000-200,000 IU/d) Dihydrotachysterol (DHT) 0.25-1 mg/day (30,000-120,000 IU of D2) The onset of action can take several weeks & effect may be prolonged because of the long t1/2 of vit. D. • Activated forms of vit. D must be given when renal or hepatic failures. • 25-Hydroxycholecalciferol (calcifediol) or 1,25-DHC (calcitriol) • Active forms of vit D OA 3-7 days and are preferred because their shorter half-lives reduce the risk of prolonged hypercalcemia. • Ca supplements 25-100 mmol/ day (1 to 4g) elemental Ca is begun simultaneously. • Ca carbonate contains the highest amount of elemental Ca 400 mg/ 1,000 mg • Other salts: Ca lactate contains, Ca gluceptate & Ca gluconate • Ca carbonate is preferred because lower # of tablets used. • When hypocalcemia is caused by hypoparathyroidism → parathyroid hormone replacement is indicated & is the only therapy that raises [Ca] • MAGNESIUM: 1.6-2.4mEq/L(0.8-1.2 mmol /L) • 99% in bone & intracellular & 1% in vascular space ( 25% is PB & 75% ionized) • Hypermagnesemia is rarely seen without severe renal dysfunction. * Mg-containing antacids are often a contributing factor in this situation. • All sources of exogenous Mg should be discontinued. • Treatment of Hypermagnesemia: Treatment of Hypermagnesemia: • Similar as Tx of hyperkalemia • Hypomagnesemia • usually appears with hypokalemia, hypocalcemia, & hypophosphatemia. • Concentrations of these electrolytes should be measured • Therapy of hypomagnesemia: • • • • • IV MgSO4 or oral MgO or Mg gluconate salts. IV MgSO4 dose 1 mEq/kg/day if [Mg] < 0.6 mmol/L, & 0.5 mEq/kg/day if [Mg] is 0.7-1.2 mmol /L. IV MgSO4 is administered slowly @ 0.5-1 g/hr. Serum [Mg] may take up to 48 hrs to equilibrate with intracellular shifting. • The oral replacement of large deficits can be difficult (may cause diarrhea) • MgO capsules are most commonly given (6.2 mmol/250 mg MgO) because of pt. convenience, but solutions of magnesium sulfate & gluconate are also available. • • • • PHOSPHORUS: 2.5-5 mg/dL ( 0.8-1.6 mmol/ L) 99.99% in bone & the intracellular space. Hyperphosphatemia: Almost always from ↓ excretion in the presence of severe renal dysfunction • Treatment of Hyperphosphatemia: a) ↓ P intake Or b) ↓P absorption from the GI by binding it with Ca salts, or Al-containng antacids, or sevelamer (polymeric compound). **Careful from accumulation of Ca or Al in renal failure • Hypophosphatemia: • Abnormality usually is the result of starvation & appears • with simultaneous deficits in other intracellular ions. • Therapy: • Replacement with Na or K salts of PO4. • Initial PO4 dose 0.64 mmol/kg/day if serum [P] < 0.5 mmol /L (1.5 mg/dL) 0.32 mmol/kg/day if [P] is 0.5 -0.7 mmol/L (1.6-2.2 mg/dL). • Therapy should be given over @ least 6 hrs to allow for equilibration into • the intracellular space. • Oral Na & K PO4 replacement (as capsules, packets, or solution) • Large oral dosages → not recommended. • Dosages of 8-16 mmol PO4 (250-500 mg) 4X/day after meals & @ bedtime are usually tolerated * Large doses may be given IV