The Changing Climate of CME
advertisement

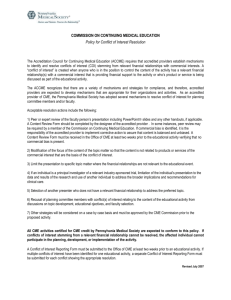
Sara Lovell, CPCS Education Coordinator Providence Alaska Medical Center Understand the history of CME and why it had to change Discuss the 22 accreditation criteria to ensure quality and value in a CME program What you can do to strengthen your CME program Using CME to continuously improve quality and patient care for your facility Continuing Medical Education Medical School Residency Fellowship CME www.accme.org 700 ACCME –accredited organizations Medical schools, nonprofit physician membership organizations (i.e. medical specialty and state medical societies, hospitals/ healthcare delivery systems, publishers and education companies, government and military organizations, and insurance and managed-care companies. 43 State and Territory Medical Societies as Accreditors for more than 1,300 local organizations, such as community hospitals, state specialty societies, and county medical societies, offering CME In total, there are more than 2,000 accredited CME providers, including organizations accredited by the ACCME and by ACCME recognized accreditors Each year accredited providers offer more than 125,000 activities across the country. Accredited education activities draw more than 23 million health care professionals annually. Activities include • Live meetings and courses • Medical Journals • The Internet Call from a drug rep “Mr. Pushy” “The speaker would love to bring his knowledge to Alaska!” “Our company will pay for everything!!!” “It’s a win win” OR… Administration “My friend the expert” Fishing trip to write off CME to our physicians Sound good??? 2002 - Clinical Content Validation Policy Ensuring that patient care recommendations are based on scientific evidence. Policy issued regarding clinical content validation in CME activities. All recommendations involving clinical medicine in CME activities must be based on evidence that is accepted within the profession of medicine. All scientific research used to support patient care recommendations must conform to generally accepted standards of experimental design, data connection and analysis. Providers are ineligible for ACCME accreditation or reaccreditation if their activities promote treatments that are known to have risks or dangers that outweigh the benefits or are known to be ineffective in patient treatment. 2004: Standards for Commercial Support: Standard to Ensure Independence in CME Activities The ACCME safeguards CME’s independence and freedom from commercial bias: Building on guidelines first issued in 1992, the 2004 Standards for Commercial Support: Standards to Ensure Independence in CME Activities impose stringent restrictions on CME providers’ interactions with drug /device companies and other companies the ACCME defines as commercial interests. The ACCME allows providers to accept company funding for CME activities, but prohibits any commercial influence, direct or indirect, over CME content. 2006 ACCME Accreditation Criteria Criteria call on accredited providers to offer educational activities that address physicians’ real-world practice needs, whether their scope of practice is in clinical care, research, health care administration, or other areas of medicine. Accredited CME is now strongly positioned to support US health care quality improvement efforts and to align with emerging continuing professional development systems 2006 ACCME Accreditation Criteria CME activities go beyond giving physicians new information—they help doctors translate knowledge into action that improves their performance and patient outcomes. CME providers evaluate the changes in physician competence, performance, or patient outcomes that result from their educational programs. The Accreditation Criteria foster leadership, collaboration and system-wide change by rewarding CME providers with Accreditation with Commendation if (among other requirements) they participate in quality improvement initiatives within their institution or health care system. Criterion 1 – Mission Statement CME purpose Content areas Target audience Type of activities Expected results Changes in competence Changes in performance Changes in patient outcomes Competence Knowledge into action Performance Will this change their practice? Patient Outcomes Partnering with quality to track and trend patient outcomes. What are the results? Did it work? What is next? Criterion Identifying PRACTICE GAPS of learners Criterion 2: Identifying Educational Needs 3: Designed to change Competence Performance Patient Outcomes Practice Gaps Where you are currently… Where you would like to be… Being pro-active and identifying these practice gaps and creating meaningful ideas and solutions to close the gap Criterion 4: Matching content to learners current and potential scope of professional activities Criterion 5: Educational format appropriate for the following Setting, objectives, and desired results Criterion 6: Context of desirable physician attributes Institute of Medicine (IOM) competencies ACGME competencies Criterion 7: Independent of commercial interests Criterion 8: Appropriately managing commercial support If applicable Standards of Commercial Support Criterion 9: Maintains a separation of promotion from education Vendors remain outside of the education room Criterion 10: Actively promotes improvement in health care and NOT proprietary interests of commercial support Criterion 11: Analyzes changes in learners as a result of the overall program’s activities/educational interventions Competence, performance, or patient outcomes Criterion 12: Analysis of program on the degree to which the CME mission has been met Ongoing review of the Mission Statement Criterion 13: Identifies, Plans and implements the needed or desired changes in the overall program Planners/ Teachers Infrastructure Methods Resources Facilities Interventions, etc. Criterion 14: Identified program changes/ improvements that are needed to improve in order to meet the mission are underway or completed. Criterion 15: Demonstrate that the impacts of the program improvements, that are required to improve on the provider’s ability to meet the CME mission, are measured. Criterion 16: Integrates CME into the process for improving professional practice. Criterion 17: Utilizes noneducation strategies to enhance change Criterion 18: Identifies factors outside provider’s control that impact patient outcomes Criterion 19: Implements strategies to remove, overcome or address barriers to physician change. Criterion 20: Builds bridges with other stakeholders Criterion 21: Participates with in a system framework for QI Criterion 22: Influence the scope and content of activity/educational interventions Mission Statement Needs Assessment Practice Gaps Plan with a Purpose Standards for Commercial Support Evaluate and follow up Track and Trend Resources in your own backyard -Bob Moawad