Clinical Pathology of Respiratory Diseases
advertisement

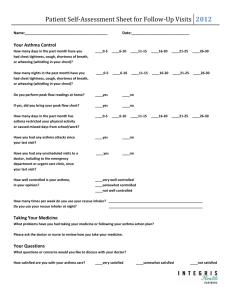
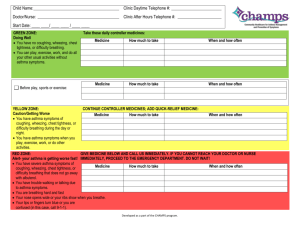
Clinical Management Respiratory Diseases Judith Coombes University of Queensland Brisbane, Australia Pathology • major international cause of morbidity and mortality • In Australia single biggest cause of days lost from work • generate largest number of GP visits Judith Coombes UQ and PAH Objectives • Be able to interpret Spirometry as a lung function test and monitoring tool • Be able to interpret Peake Expiratory Flow rate (PEFR) as a monitoring tool • Understand goals of treatment and be able to communicate pharmaceutical care plan in asthma • Understand goals of treatment of and be able to communicate pharmaceutical care plan in COPD Not discussing infections, neoplasms or TB The Lungs Trachea Trachea Bronchus(L&R) Bronchi Bronchiole Alveoli Respiratory Symptoms • • • • • cough sputum production/haemoptysis dyspnoea wheezing chest/lung pain Measurement of ventilatory function • • • • • Spirometry PEFR Blood Gas Exercise test-6 min chest Xray- normal is asthma and COPD Spirometry • Spirometer – FVC = Forced Vital Capacity – FEV1= Forced Expiratory Volume over 1 second – FEV1/FVC is forced expiratory ratio • should be >75% • useful for diagnosis • accurately measures degree of impairment Normal PEFR • Peak Flow Meter – maximum flow rate which can be forced during an expiration – may differ between meters – Submaximal effort invalidates reading – Not a substitute for spirometry – most useful for regular monitoring to detect variation – warning signs • sustained reduction • >20-25% diurnal variation Chest X ray • Diagnosis is uncertain (PE, pneumonia, heart failure) • symptoms may not be explained by asthma or COPD • physical evidence of complicationspneumothorax, atelectasis (lung collapse) • failure to respond to treatment Blood Gas (arterial) • H+ rises with Pco2 • In acute hypoventilation CO2 rises and so does H+ causing respiratory acidosis • In acute hyperventilation CO2 drops as does H+ causing respiratory alkalosis • (in acute no time for metabolic process so bicarbonate is not changed) Oximetry • • • • Measure oxygen saturation Non invasive Light emiting diodes Expressed as % where normal is 100% Asthma • a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role, in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils and epithelial cells. In susceptible individuals this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly, at night or in the early morning. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment. The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli. USA97 Airflow obstruction (Excessive airway Narrowing) • Smooth muscle hypertrophy and hyperplasia • Inflammatory cell infiltration • Oedema • Goblet cell and mucous gland hyperplasia • Mucus hypersecretion • Protein deposition • Epithelial desquamation Asthma Diagnosis-1 • No Gold Standard – Consensus of respiratory physicians • History, physical examination, supportive diagnostic testing • History – Wheeze – Chest tightness – Shortness of breath – cough Asthma Diagnosis-2 • Physical examination – Expiratory wheeze suggests asthma (not pathonomonic) – Absence of physical signs doesn’t exclude asthma – Crackles indicate concurrent or alternate diagnosis Asthma diagnosis -3 • Diagnostic testing –Spirometry • Pay Attention to technique – Pre and post bronchodilator – Baseline FEV1>1.7L and increase of 12% post bronchodilator is significant – Or 200ml greater than baseline – Or same rules for FVC • Also % predicted from tables in the Asthma guidelines Spirometry for asthma management Assessment of severity • Severe acute attack <50% predicted or < 1litre • Back titration of medication • Check symptomatic assessment • Maintain best lung function Asthma PEFR with asthma • Diagnosis-not a substitute for spirometry – PEF increases >15% with bronchodilator – PEF in adult varies >20% for 3 days in a week over several weeks • Severe Acute – <50% predicted or < 100 L/min • Useful for daily home measurement • Useful in action plan • >80% OK, 60-80% increase preventer, 40-60% oral steroids, <40% no relief 000 Asthma treatment National Asthma Council in Australia – www.nationalasthma.org.au/cms/index.php – Reduce mortality &morbidity of asthma • • • • • Education Patient self monitoring Appropriate drug therapy Regular medical review Written asthma action plan Asthma management • Acute asthma management – Treatment depends on severity • Mild, moderate, life threatening • Requires emergency care • Hospital admission • Long term asthma management-chronic • • • • Minimise symptoms and need for reliever No exacerbations No limitation on physical activity Normal Lung Function Asthma Management • Medications to treat bronchospasm – ACUTE – RELEIVERS • Short acting ß2-adrenergic agonists eg salbutamol terbutaline • Anticholinergic eg ipratropium Relievers Asthma Management • Medications to treat bronchospasm – Chronic – SYMPTOM CONTROLLER • Inhaled long acting ß2-adrenergic agonists eg salmeterol • Also use – Theophylline – Oral ß2-adrenergic agonists (salbutamol syrup) Asthma Management • Medications to treat inflamation PREVENTERS Inhaled sodium cromoglycate Inhaled nedocromil sodium Inhaled cortocosteroids eg beclomethasone Oral corticosteroids eg prednisolone Leukotrienne receptor antagonists eg montelukast Beclomethasone dipropionate Asthma Action plans • Developed by doctor with patient • Added role for pharmacist to give advice to patient • Individualised Action for Deterioration in asthma – ↑ in frequency, severity of symptoms – ↑ use of bronchdilator – Drop in peak flow Misuse of Home Nebulizers High Among Inner-City Children with Asthma October 25, 2006 (Salt Lake City) A study of asthma-related deaths among inner-city children and young adults shows that only about half use their home nebulizers as prescribed and rarely have an asthma action plan to manage disease exacerbations, or if they do have a written plan in the home, they rarely use it. The findings were presented here yesterday at CHEST 2006, the 72nd annual meeting of the American College of Chest Physicians. COPD • smoking is major cause but susceptibility is variable • directly related to exposure to tobacco smoke – pack years=cigarettes/day x years of smoking /20 • relatively fixed airway obstruction with minimal reversibility from bronchodilators COPD • Chronic bronchitis- productive cough for >3 months in 2 successive years • emphysema-abnormal permanent enlargement of air-spaces distal to terminal bronchioles caused by destruction of alveolar walls. • Most have a combination of both • Elderly with reversibility has all 3 COPD = shaded bit Diagnosis of COPD • symptoms – breathlessness doesn’t occur until obstruction is advanced (unless intercurrent infection) • physical examination – little until disease is severe-over inflated chest • chest x rays – over inflation, enlarged heart, bullae • spirometry – mild check FEV1/FVC<75% – moderate check FEV1 % of predicted COPD Show ceases smoking figure Progression Severity Symptoms Treatment Mild FEV1<80 Smokers cough Little breathlessness Not known to GP Moderate FEV1<60 Breathlessness on moderate exertion, hypoxaemic, sputum, known to GP Breathlessness on any exertion, some hypercapnic, known to hospital Cease smoking, Antibiotics, Occasional bronchodilator Bronchodilators, trial of steroids Severe FEV1<50 Flu vaccine, pulmonary rehabilitation, assess for LTOT COPD Management – Acute exacerbations – – – – Bronchodilators Oxygen Corticosteroids Antibiotics – Long term treatment- chronic – – – – – Stop smoking Bronchodilators Corticosteroids Immunisation-Pneumonia and flu Pulmonary rehabilitation Bronchiectasis defined as dilation of the bronchi• bronchial walls become inflamed, thickened and irreversibly damaged. • Mucociliary transport is impaired-bacterial infections • cough productive of sputum Cystic Fibrosis • dysfunction of exocrine glands -abnormal mucus production – recurrent bronchopulmonary infection – finger clubbing – haemoptysis Interstitial lung disease • heterogeneous group involving alveolar walls and peri alveolar tissue • insidious onset, chronic disease • inflammatory process probably initiated by an antigen • eventual interstitial fibrosis will cause a restrictive pattern Restrictive Severe Obstructive Sleep Apnoea • 2% women , 4% men • Recurrent episodes of airway occlusion in sleep – Apnoea – Arousal – Daytime sleepiness – Increased CO2 – Sleep lab – Weight loss, CPAP