Coding for Billing
©2013 MFMER | slide-1
REMINDER:
Please fill out unit
evaluations
Copyright © The REACH Institute. All rights reserved.
The presenter gratefully acknowledges the
utility of the AAP Coding for Pediatrics 2013
in the preparation of this presentation!
Copyright © The REACH Institute. All rights reserved.
Learning Objectives
To increase understanding of adapting E/M
& procedure codes to primary care-based
child mental services
To describe basic applications of essential
FTF procedure codes and strategies:
96110, Billing based on “Time spent
counseling”, & Prolonged Service Codes
To review the key non-FTF codes relevant
to PC-based child mental services
Copyright © The REACH Institute. All rights reserved.
Why Should I Worry?
Proper coding enables higher quality,
evidence-based care and practices
Proper coding -> over time, results in
increased coverage & reimbursement of
widely used codes
Codes change regularly
– Coders, practice managers often out-of-date!
Experience of past PPP participants
– $10-$15K of practice income recouped
Copyright © The REACH Institute. All rights reserved.
96127
(for rating scales)
Copyright © The REACH Institute. All rights reserved.
Rating Scales
Must be standardized
Informal checklists don’t qualify
Ex: ASQ-SE, PEDS, M-CHAT, Vanderbilt
ADHD, SCARED, PSC, PHQ-9, Connor’s
ADHD, CBCL, BASC-2, BRIEF, CDS
May assign one unit of 96110 for each form
completed, scored, interpreted and noted in
the medical record
Copyright © The REACH Institute. All rights reserved.
96127 Facts
No physician work included: premise is
the scales are given to respondent,
explained and scored by nonphysician
The physician work of interpreting the
results and recording the results is
included in the accompanying E/M
work
Copyright © The REACH Institute. All rights reserved.
Using 96127 w/ E/M
Most insurer’s computer software requires
a modifier to get the procedure through their
system
Modifier may be appended to the E/M code
or to the procedure code, but modifiers are
E/M and procedure specific
If at first you don’t succeed, try another
tactic!
Copyright © The REACH Institute. All rights reserved.
Modifiers: An Overview
-25: Significant, separately identifiable E/M
service by the same physician on the
same date of the procedure or other
service
- 59: “modifier of last resort”, & indicates
distinct service from others on same day
- 76: also indicates distinct service from
others on same day. Not used by Medicaid
Copyright © The REACH Institute. All rights reserved.
Coding 96127
Examples
Copyright © The REACH Institute. All rights reserved.
Sue’s Visit: Option 1
99383 (well-child, ages 7-11)
99214-25 (99214 – Elements, MDM)
(2) 96127 (PSC, SCARED)
This is for insurers who allow -25 and
multiple units of a procedure
Copyright © The REACH Institute. All rights reserved.
Sue’s Visit: Option 2
99383
99214-25
96127
96127-76
This is for insurers who permit -25, but want
each procedure on a separate line AND who
do not adhere to CMS guidelines
Copyright © The REACH Institute. All rights reserved.
Sue’s Visit: Option 3
99383
99214
96127-59
96127-59
This could be used for payers who do
not permit -25 use and who also follow
CMS guidelines regarding -76.
Copyright © The REACH Institute. All rights reserved.
Sue: Next Steps
Behavioral rating scales sent to Sue’s
teacher and request for interim grades
Possible telephone call from family
before next visit
Is this all post-service work? Can this
work be captured for payment?
Copyright © The REACH Institute. All rights reserved.
Good News!: Non Face-to-Face
Codes
• 99339-99340: Home Care Plan Oversight
• 99441-99449: Telephone Care
• 0074T: Online E/M Services
• 99080: Special reports such as insurance
forms, more than the information conveyed
in the usual medical communications or
standard reporting forms
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: I
99339-99340 Individual physician supervision of a
patient (patient not present) in home (or group
home) requiring complex and multi-disciplinary
care modalities
These 2 codes are for children w/ complex and
chronic special healthcare needs living at home
Describes the work a physician provides on a
monthly basis while performing complex
supervision services to a patient in a home – (not
skilled nursing facility)
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: II
Recurrent physician supervision of a complex patient
or pt. who requires multidisciplinary care and ongoing
physician involvement
Non-face-to-face
Reflect the complexity and time required to supervise
the care of the pt.
Reported separately from E/M services
Reported by the MD who has the supervisory role in
the pt’s. care or is the sole provider
Reported based on the amount of time spent/calendar
month
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: III
Services less than 15 minutes reported
for the month should not be billed
99339: 15-29 minutes/month
99340: greater than 30 minutes/month
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: IV
Services might include:
– Regular physician development and/or revision of
care plans
– Review of subsequent reports of patient status
– Review of related laboratory and other studies
– Communication (including telephone care) for
purposes of assessment or care decisions w/
healthcare professionals, family members, legal
guardians or caregivers involved in patient care
– Integration of new information into the medical tx.
plan and/or adjustment of medical tx.
– Attendance at team conferences/meetings
– Development of extensive reports
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: V
Services NOT included in care plan
oversight:
– Travel time to and from the facility or place of
domicile
– Services furnished by ancillary or incident-to staff
– Very low-intensity or infrequent supervision services
included in the pre- and post-encounter work for an
E/M service
– Interpretation of lab or other dx. studies associated
w/ a face-to-face E/M service
– Informal consultations w/ health professionals not
involved in the pt’s. care
– Routine post-operative care
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: VI
This code should not be used for
intermittent telephone care to discuss a
single topic, such as one lab result or care
change.. That would not be “complex and
multidisciplinary care modalities.”
Copyright © The REACH Institute. All rights reserved.
Home Care Plan Oversight: Log
Date Last
Appt.
Date of
Service
Service
Action
After
Service
Time
2/8/10
2/20/11
TC: Talked
w/mother
re: severity
of sxs
Offered to
see Nora
12 min.
2/8/10
2/21/10
TC:
Explained
need for
scale to
teacher
Waiting for
scales
13 min.
2/8/10
2/24/10
Reviewed
Teacher
scale
Moved up
Nora’s
appt.
4 min.
Copyright © The REACH Institute. All rights reserved.
Total Time/
month
--
29 min.
Non-Face-To-Face Service
Coding: Telephone Care
• 9944x: Telephone E/M service provided by a physician to
an established patient, parent or guardian NOT
originating from a related E/M service provided within the
previous 7 days nor leading to an E/M service or
procedure within the next 24 hours or soonest available
appt.
• 99441: 5-10 min. medical discussion
• 99442:11-20 min. medical discussion
• 99443:21-30 min. medical discussion
• 99449: CAP-PCP medical consultation (Minnesota)
Copyright © The REACH Institute. All rights reserved.
Telephone Care
Telephone care levels may represent three
levels of complexity –need to document this
to support charge
Documentation should:
–
–
–
–
–
Be thorough
Fulfill the need for continuity of care
Describe the complexity of the call
Meet the requirements of the typical E/M visit
A general note including the key elements of hx. and
medical decision-making
– Time spent on call
Copyright © The REACH Institute. All rights reserved.
Telephone Care
The call from the physician must be in
response to a request from the patient or
the family for this code to be used
– (This rule does NOT apply to MN 99449
CAP-PC medical consultation codes)
Copyright © The REACH Institute. All rights reserved.
School-Based Meetings
Code w/ 99211-15 (est. Patient E/M codes) –
On the basis of time; add prolonged services
face-to-face if patient is present –and non-FTF
if patient is not present if needed: payers may
not pay for this, however
If teachers are the principal attendees, these
should not be coded with the Medical Team
Conference codes (99366-99368) as these
descriptors specify interdisciplinary team of
health care providers
Copyright © The REACH Institute. All rights reserved.
Time Reporting:
CPT Counseling Rule
• As of 2010, time must be used for code selection when
the time spent in ‘counseling and coordination of care’
> 50% of the E&M visit
• The 3 key components of history, PE, MDM may be
ignored
– Only time is used to select the level of care
• A summary of the ‘counseling’ discussion should be
included with the note
• Does not include screening time
– Reported separately, with modifier (-25) appended to E/M
Copyright © The REACH Institute. All rights reserved.
Pearl
Time is your friend in reporting
mental health/ behavioral health/
developmental-focused services.
ALWAYS think of time first as the
appropriate basis for valuing the visit.
Copyright © The REACH Institute. All rights reserved.
Time: Basis for
Parent-Only Meetings
• How to code for counseling and care
coordination:
– May be used when the patient is present or when
counseling a parent when the patient is not physically
present
– Document the discussion’s topic
– When time spent in counseling and/or care
coordination is over 50% of face-to-face time, CPT
now says you must use this as the critical factor to
qualify for a particular E/M service level
– Pediatricians spends the majority of parent-only
conference on counseling→code based on time!
Copyright © The REACH Institute. All rights reserved.
Documentation Requirements to
Bill Based on Time
• The total length of time of the encounter should be
documented and the record should describe the
counseling and/or activities to coordinate care
• The medical record must reflect the extend of counseling
and/or coordination of care
• Resident/NP/PA face to face time can not be included
(except under specialty specific Medicaid contracts)
• It is a good idea to document in a separate paragraph
what documentation is supporting the
counseling/coordination of care. This will make it easy to
justify the time spent.
Copyright © The REACH Institute. All rights reserved.
Time Examples
• Good
• Bad
– “I spent 40 minutes total time
and 25 minutes was spent in
counseling and coordination
of care with the patient.”
– “I spent 40 minutes total time
and more than 50% of the
visit was spent in counseling
and coordination of care with
the patient.”
– “I spent 10 minutes talking
with the patient about her
diagnosis”
Why? Fails to show whether
more than half the time of
the visit was dedicated to
counseling
Assume elaboration in
documentation of what was
discussed with the patient.
Copyright © The REACH Institute. All rights reserved.
Prolonged Services
(99354-99359)
• No longer add-on codes-put on separate line
• Reported in addition to other physician services,
including E/M services at any level
• Code series defining prolonged services by:
– Site of service
– Direct or without direct patient contact
– Time
• Total time for a given date, even if the time is not
continuous
• Time must be of 30 minutes or more
Copyright © The REACH Institute. All rights reserved.
Prolonged Services
Direct Patient Care
Outpatient
Face-to-Face
99354: first 30-74 min
Face-to-Face
99355: each add 30 min >75
99358: first 30-74 min of non
Before or after Face-to-Face
face-to-face
Before or after Face-to-Face
99359: each add 30 min >75
min
Copyright © The REACH Institute. All rights reserved.
Prolonged Visit Coded on
Complexity
• If your E/M level was made based on
complexity, AND
• visit runs more than 30 minutes over the
code time description, AND
• total counseling/care coordination time is
not > 50%
• THEN you may add the prolonged service
code to account & describe the extra time.
Copyright © The REACH Institute. All rights reserved.
Panel & Discussion
Q&A
Copyright © The REACH Institute. All rights reserved.
Summary
Understanding Coding & Billing is essential to
enable doing quality PC mental healthcare
services – someone has to “mind the store”!
Business managers, coders, etc., often out-ofdate. How will I ensure continued updating in my
practice setting?
– Codes vary setting to setting, company by company,
state-by-state, and year-to-year
Which of these 4 key coding opportunities need
to be further investigated, and possibly put into
my practice?
Copyright © The REACH Institute. All rights reserved.
Resources
www.aap.org/sections/schoolhealth
www.aap.org/mentalhealth
www.aacap.org
www.schoolpsychiatry.org
http://www.mnpsychconsult.com
(for Minnesota PCPs and CAPs!!)
Lwegner@med.unc.edu
Copyright © The REACH Institute. All rights reserved.
Appendix of Basic Coding
Information
Copyright © The REACH Institute. All rights reserved.
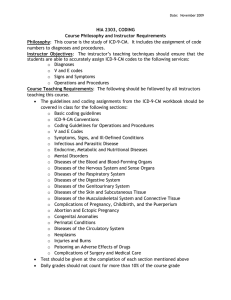
CPT and ICD-9-CM
• ICD-9-CM: International Classification of Diseases,
Ninth Revision, Clinical Modification
– Why the service was done
– Information collected by payers to manage risk
(preexisting conditions; refused diagnoses)
• CPT: Current Procedural Terminology
– What was done
– Provides the basis for payment
Copyright © The REACH Institute. All rights reserved.
ICD-9-CM
• ICD-9-CM: International Classification of Diseases, Ninth
Revision, Clinical Modification
– Why the service was done
– Information collected by payers to manage risk
(preexisting conditions; refused diagnoses)
• Important point: The Health Insurance Portability and
Accountability (HIPAA) Act of 1996 requires payers and
physicians to use ICD-9-CM. As revised ICD-9-CM codes are
activated, you must use these updated codes. Obviously,
these codes explain to payers the specific reason a patient
was seen.
Copyright © The REACH Institute. All rights reserved.
ICD-9-CM
• The reason for the service (visit)
• The first diagnostic code reflects the condition the
professional is actively managing:
– “the reason for the visit”
• Subsequently listed codes
– Factors important to condition #1
– Coexisting conditions tx. and mgment of #1
• If a child is seen for a residual condition (e.g.
hearing deficit), code this first with the cause of
the condition as a secondary ICD-9-CM code
(e.g. meningitis)
Copyright © The REACH Institute. All rights reserved.
ICD-9-CM
“The Top→Down View”
• Code to the highest degree of specificity
• Code to the highest degree of certainty for the encounter
such as symptoms, signs, abnormal test results
• Probable, suspected, questionable, or rule out should not
be coded
• List the ICD-9-CM code that is identified as the main
reason for the service first, then list co-existing conditions
• Chronic disease treated on an ongoing basis may be
coded
• Do not code for conditions previously tx that no longer
exist
Copyright © The REACH Institute. All rights reserved.
ICD-9-CM
• Do code only the conditions/problems you are
actively managing at the time of the visit and
diagnoses affecting the current status of the child
• Do not code for previously treated conditions
• May include conditions existing at the time of the
patient’s initial contact as well as conditions
developing subsequently affecting treatment
• Dx. relating to a pt.’s previous medical problems
w/ no bearing on the present condition are not
coded.
Copyright © The REACH Institute. All rights reserved.
ICD-9-CM
• Do not code dx. listed as “rule out,”
“probable” or “suspected” –they are not
established in out-patient practice
• Do code to the highest degree of certainty
• Do not code symptoms if a dx. has been
made: Ex.: If a child w/ dx’d ADHD is seen for
routine med. monitoring and headaches are
reported w/ meds.: code 314.01 first, then
headache as #2.
Copyright © The REACH Institute. All rights reserved.
NEC and NOS
• Residual Categories
– NEC: Not elsewhere classifiable: conditions
specifically named in the medical record but not
specifically listed under a code description
– NOS: Not otherwise specified: a diagnostic
statement lacking detail in describing a specific
condition (e.g. 314.9 unspecified hyperkinetic
syndrome)
Copyright © The REACH Institute. All rights reserved.
Pearls
• Code the diagnosis to the highest level of
certainty (the words in the descriptor)
• Code the diagnosis to the highest level of
specificity (the numbers in the descriptor)
Copyright © The REACH Institute. All rights reserved.
Pearls
• Remember, a chronic condition, such as
ADHD or depression, managed on an ongoing
basis may be coded and reported as many
times as applicable to the patient’s treatment.
• The level of the E/M visit may change as the
complexity of the child’s needs change.
Copyright © The REACH Institute. All rights reserved.
CPT and MH Coding
• Current Procedure Terminology = CPT
– A tabular listing of almost all known encounters
w/patients
– Published annually (Oct. 1) by the AMA
– Includes codes for cognitive, procedural and
supplies
– Services may be provided in any location
– Codes not limited to specialty: ANY physician
may use any code
– Codes should be chosen most accurately
describing the service provided
Copyright © The REACH Institute. All rights reserved.
RVU Components of
Medical Provider Work
• Pre-, intra-, post- service work
– Time to perform the service
– Technical skill and physical effort
– Mental skill and judgment
– Psychological stress associated with iatrogenic
risk
Copyright © The REACH Institute. All rights reserved.
CPT Updates
• Documentation guideline revisions by CMS
and AMA: www.cms.hhs.gov/MLNProducts
• AAP updates on these: www.aap.org; AAP
News; AAP Pediatric Coding Companion
newsletter
• AACAP updates published in their newsletter
Copyright © The REACH Institute. All rights reserved.
Selecting a Procedure Code
• First, you must select a procedural code
appropriately reflecting the service provided
based on:
• Your knowledge of the patient (new vs
established)
• The complexity of your encounter
• Face-to-face time spent on your encounter
• The ‘nature’ of the encounter
Copyright © The REACH Institute. All rights reserved.
Coding the Visit
• When selecting a procedure code, the ideal
goal is to completely describe all the services
provided to the patient at that visit. Evaluation
and Management (“E&M”) procedure codes
are the basic physician visit codes. E&M
codes include:
– Consultation codes: 99241-99245
– New patient visits: 99201-99205
– Established patient visits: 99211-99215
– Preventive care visit (primary care, not specialty
service)
Copyright © The REACH Institute. All rights reserved.
History
Type of
Visit
Problem
focused
Expanded
problem
focused
Detailed
Comprehensive
HPI
ROS
PFSH
Brief 1-3
N/A
N/A
Brief 1-3
Brief (1)
N/A
Extended 4+ Extended (2-9)
Pertinent (1)
Extended 4+ Complete (10+) Complete
(2/3 or 3/3)
Copyright © The REACH Institute. All rights reserved.
Physical Exam
• Problem Focused
– Limited to affected body area or organ system
– 1 body area/organ system
• Expanded Problem Focused
– Affected body or organ system and other symptomatic or related
organ system
– 2-4 body areas/organ systems
• Detailed
– Extended exam of affected body area(s) and other symptomatic or
related organ systems
– 5-7 body areas /organ systems
• Comprehensive
– Complete single system specialty exam or
– Complete multi-system exam
– 8 or more body areas/organ systems
Copyright © The REACH Institute. All rights reserved.
Medical Decision Making
• Number of possible diagnoses and/or
management options
• Amount and/or complexity of medical records,
diagnostic tests, and/or other information that
must be reviewed
• Risk of complications, morbidity and/or mortality,
associated with the patient’s presenting
problem. Includes need for diagnostic
procedures and management options
Copyright © The REACH Institute. All rights reserved.
Medical Decision Making
Decision Making
Number of
Diagnoses
Straight forward
Minimal
Min. or None
Minimal
Low Complexity
Limited
Limited
Low
Moderate
Complexity
Multiple
Moderate
Moderate
Extensive
Extensive
High
High Complexity
Amount of
Data
Copyright © The REACH Institute. All rights reserved.
Risk of
Complication
E/M Documentation
• Read the CPT descriptor to identify the
documentation needs of your code
– E.g. E/M codes: “Key elements:”
– Date of service
– Name of referring professional (if consultation)
– Time spent in encounter (if counseling and care
coordination is > 50% of total face-to-face time)
– Chief complaint
– Pertinent history
– Physical exam
– Laboratory or developmental testing results (if done)
– Impression w/ differential diagnosis
– Treatment recommendations, including medications
– Follow-up plans
Copyright © The REACH Institute. All rights reserved.
Office Visit: New Patient
Codes
99201
99202
History
Problem
Focused
99203
99204
99205
Expanded
Problem
Detailed
Focused
Comprehensive
Comprehensive
Exam
Problem
Focused
Expanded
Problem
Detailed
Focused
Comprehensive
Comprehensive
Decision
Making
Straight
Forward
Straight
Forward
Low
Complex
Moderate
Complex
High Complex
Time FF
10
20
30
45
60
Key #
3 of 3
3 of 3
3 of 3
3 of 3
3 of 3
Copyright © The REACH Institute. All rights reserved.
Office Consultation: New
Code
History
Exam
99241
99242
99243
Expanded
Problem
Problem
Detailed
Focused
Focused
Expanded
Problem
Problem
Detailed
Focused
Focused
99244
99245
Comprehensive
Comprehensive
Comprehensive
Comprehensive
Decision
Making
Straight
Forward
Straight
Forward
Low
Complex
Mod Complex
High Complex
Time FF
15
30
40
60
80
Key # 3/3 3/3
3/3
3/3
3/3
3/3
Copyright © The REACH Institute. All rights reserved.
Consultation/New Pt. Requirements:
Complexity
• 99244
• 99245
• HPI-4 elements, ROS-10+,
PFSH-3
• HPI-4 elements, ROS-10+,
PFSH-3
• PE-8 elements, must be
organ systems: Const,
Eyes, ENT, Resp, CV, GI,
GU, MS, Skin, Neuro,
Psych, Heme/Lymph
• PE-8 elements, must be
organ systems: Const,
Eyes, ENT, Resp, CV, GI,
GU, MS, Skin, Neuro,
Psych, Heme/Lymph
• Medical Decision MakingMODERATE
• Medical Decision MakingHIGH
The difference between a level 4 and a level 5 is
only the Medical Decision Making
Copyright © The REACH Institute. All rights reserved.
Office Visit: Consultations
• Consultation is a service provided by a physician
whose opinion or advice is requested by another
physician or other appropriate source**
• Consultant may initiate diagnostic and/or
therapeutic services
• Consultant must document:
– Request for consultation (written or verbal)
– Need for consultation
– Opinion and services ordered and performed
– Communication by written report back to the referring
source
– The patient was returned to the requesting
physician’s care
Copyright © The REACH Institute. All rights reserved.
“In House” Consultations
• If you accept an ‘in house’ consult, you still
must adhere to the “3 R’s”!
– You and the requesting physician must document the
medical necessity and reason for the consult.
– You must render an opinion.
– After you see and evaluate the patient, you must give
the requesting physician a report – but this ‘report’
may be your summary in the group chart if you’re
sharing a group chart.
Copyright © The REACH Institute. All rights reserved.
Medical Services to Remember!
69210 Removal impacted cerumen, one or both ears
– e.g. Child w/ ADD eval and questionable hearing: can’t get reliable
OAE due to impaction in one ear
• Must report different dx. for the removal and the E/M
service and should have two separate notes for the
two procedure codes, both notes should clearly
describe the separate nature of the services
– 99244-25 New pt. consultation w/ separate procedure
– 314.01 Attention Deficit Disorder-Combined Type
– 69210 Removal impacted cerumen, one or both ears
– 380.4 Impacted cerumen
Copyright © The REACH Institute. All rights reserved.
References
Lear, JG, Isaacs, Stephen L, Knickman, JR. School
Health Services and Programs. Princeton,NJ:
Robert Wood Johnson Foundation, 2006.
US Department of Health and Human Services.
Mental Health: A Report of the Surgeon General—
Executive Summary. Rockville, MD: US Department
of Health and Human Services, Substance Abuse
and Mental Health Services Administration, Center
for Mental Health Services, National Institutes of
Health, National Institute of Mental Health; 1999
Copyright © The REACH Institute. All rights reserved.
References
American Academy of Pediatrics. Bright Futures: Guidelines for
Health Supervision of Infants, Children, and Adolescents,
Third Edition. Elk Grove Village, IL: American Academy of
Pediatrics, 2008.
AAP Committee on Coding and Nomenclature. Coding for
Pediatrics: A Manual for Pediatric Documentation and
Payment, Fifteenth Edition. Elk Grove Village, IL: Academy of
Pediatrics, 2010.
AAP Committee on Coding and Nomenclature. aappediatric
coding newsletter .Elk Grove Village, IL: Academy of
Pediatrics, 2010.
Copyright © The REACH Institute. All rights reserved.
Resources
Committee on Children with Disabilities et al. Identifying Infants
and Young Children With Developmental Disorders in the
Medical Home: An Algorithm for Developmental Surveillance
and Screening. Pediatrics. 116 (1), July 2006; 405-420.
Child and Adolescent Health Measurement Initiative. 2007
National Survey of Children’s Health. Data Resource Center
for Child and Adolescent website: www.nschdata.org
RUC Database: www.catalogue.ama-assn.org or call 800/6218335
Copyright © The REACH Institute. All rights reserved.