Urinary Incontinence - UNC School of Medicine
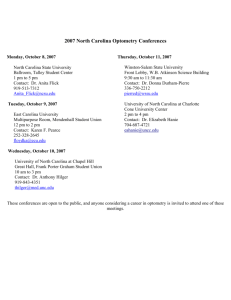
advertisement

Jan Busby-Whitehead, MD Chief, Division of Geriatric Medicine University of North Carolina Definition of Urinary Incontinence * The International Continence Society University of North Carolina School of Medicine Center for Aging and Health URINARY INCONTINENCE Common Treatable Significant Effect on Quality of Life (QoL) University of North Carolina School of Medicine Center for Aging and Health Prevalence • Community: 17% older men, up to 30% older women • Hospital: up to 50% older men and women • LTCF: 50-70% older men and women University of North Carolina School of Medicine Center for Aging and Health Hunskaar, et.al., Int Urogynecol J, 2000 University of North Carolina School of Medicine Center for Aging and Health Hunskaar, et.al., Int Urogynecol J, 2000 University of North Carolina School of Medicine Center for Aging and Health Reversible causes of UI D - Restricted mobility R - Infection, impaction I - Polyuria P - Delirium or Drugs University of North Carolina School of Medicine Center for Aging and Health Polyuria, frequency, urgency Alcohol Caffeine Diuretics Urinary retention Anticholinergics Alpha adrenergic agonists Beta adrenergic agonists Calcium channel blockers University of North Carolina School of Medicine Center for Aging and Health Bladder Anatomy Hollow, distensible, muscula organ Reservoir of urine • • • Capacity ~600 mL Desire ~200 mL Normal void ~300 mL Organ of excretion • • • • Behind symphysis pubis Female – against anterior wall of uterus Trigone Sphincter University of North Carolina School of Medicine Center for Aging and Health Physiology University of North Carolina School of Medicine Center for Aging and Health Aging Changes • Decreased bladder capacity • Reduced voiding volume • Reduced flow rates • Increased urine production at night * Nordling, J Experimental Gerontology, 2002, 37:991 University of North Carolina School of Medicine Center for Aging and Health Stress Overflow CAUSES OF PERSISTANT UI Urge/OAB Functional University of North Carolina School of Medicine Center for Aging and Health Stress UI Abrams P et al. Urology. 2003;61:37-49. The complaint of involuntary leakage with effort or exertion or on sneezing or coughing Sudden increase in abdominal pressure Urethral pressure University of North Carolina School of Medicine Center for Aging and Health Urge UI Abrams P et al. Urology. 2003;61:37-49. Ouslander J. N Engl J Med. 2004;350(8):786-799. The complaint of involuntary leakage accompanied by or immediately preceded by urgency Involuntary detrusor contractions Urethral pressure University of North Carolina School of Medicine Center for Aging and Health Overactive bladder • Includes urinary urgency with or without urge incontinence, urinary frequency, and nocturia • Associated with involuntary contractions of the detrusor muscle University of North Carolina School of Medicine Center for Aging and Health Mixed UI Abrams P et al. Urology. 2003;61:37-49. Chaliha C et al. Urology. 2004;63:51-57. The complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing Sudden increase in abdominal pressure Involuntary detrusor contractions Urethral pressure University of North Carolina School of Medicine Center for Aging and Health Overflow •Urethral blockage •The Bladder is not able to empty properly Neurogenic/Atonic Obstruction University of North Carolina School of Medicine Center for Aging and Health Functional Incontinence • Immobility • Diminished vision • Aphasia • Environment • Psychological University of North Carolina School of Medicine Center for Aging and Health Clinical Questions ? How do you evaluate for incontinence? ? Are behavioral techniques effective? For which patients? ? What drug treatments are useful and how do you use them? University of North Carolina School of Medicine Center for Aging and Health Office Evaluation of UI • Identify presence of UI • Assess for reversible causes and treat • If UI persistent, determine type and initiate treatment • Identify patient who needs further evaluation and referral University of North Carolina School of Medicine Center for Aging and Health Basic Evaluation of UI • History: Bladder diary • Physical examination, especially Genitourinary and Neurological • Bladder stress test • Postvoid residual • Urinalysis, urine culture if indicated • BUN, creatinine, fasting glucose University of North Carolina School of Medicine Center for Aging and Health Referral Criteria Recurrent urinary tract infections Hematuria Elevated postvoid residual or other evidence of possible obstruction Recent gynecological or urological surgery or pelvic radiation Failed treatment of stress or urge UI University of North Carolina School of Medicine Center for Aging and Health Cystometry • Gold standard for diagnosis • New definition for detrusor overactivity: Any rise in detrusor pressure during filling cystometry associated with symptoms and not related to abnormal bladder compliance • Provocative stimuli • Ambulatory monitoring University of North Carolina School of Medicine Center for Aging and Health Treatment Options • Behavioral • Pharmacological • Functional Electrical Stimulation • Surgery University of North Carolina School of Medicine Center for Aging and Health Are behavioral techniques effective? For whom? • Behavioral techniques are effective for treatment of stress and urge UI, and overactive bladder, but generally do not cure • Behavioral techniques are effective in community dwelling men and women • Behavioral techniques are most appropriate for cognitively intact, motivated persons University of North Carolina School of Medicine Center for Aging and Health BEHAVIORAL TREATMENTS FOR UI Self management techniques Timed or scheduled voiding Pelvic floor muscle exercise with or without biofeedback University of North Carolina School of Medicine Center for Aging and Health Self Management • Fluid Intake – Don’t reduce amount – Do not drink fluids 2 hr before bedtime – Avoid: caffeine, alcohol, nicotine University of North Carolina School of Medicine Center for Aging and Health Scheduled Voiding • Scheduled voiding with systematic delay of voiding – Schedule based on time interval pt can manage in daytime – Void at scheduled time even if urge not present; suppress urge if not time with “Quick Kegels” – Increase voiding interval by 30 min each week until continent for up to 4 hr University of North Carolina School of Medicine Center for Aging and Health Pelvic Muscle Exercises • Isolation of the pelvic muscles • Avoidance of abdominal, buttock or thigh muscle contractions • Moderate repetitions of strongest contraction possible • Ability to hold contraction 10 seconds, repeat in groups of 10-30 TID University of North Carolina School of Medicine Center for Aging and Health 100 PMFE Without Biofeedback 90 80 PMFE With 98% Biofeedback 91% 70 60 50 40 50% 30 38% 20 10 0 Range of Improvement Range of Improvement University of North Carolina School of Medicine Center for Aging and Health Randomized Trials of Behavioral Treatment for Stress UI • 24 RCTs, but only 11 of high quality • Pelvic floor exercises were effective (up to 75%)in reducing symptoms of stress UI • Limited evidence for high vs low intensity • Benefits of adding biofeedback unclear * Berghmans et al. Br J Urol 1998:82:181-191 University of North Carolina School of Medicine Center for Aging and Health Behavioral Treatment for Urge/OAB • Bladder training – Initial approach – 3 RCT: 47-90% cure rate with 6 mo f/u – Recurrence in 43-58% after 2-3 yr – 35% fewer UI episodes vs controls: Cochrane Review 2004 University of North Carolina School of Medicine Center for Aging and Health Limitations of Behavioral Treatment Studies • Studies varied in – types of UI – characteristics of subjects – intervention strategies – outcome measures used – duration of follow-up • Few studies compared the efficacy of PFME performed with and without biofeedback University of North Carolina School of Medicine Center for Aging and Health NIH Treatment Trial Kincade, Dougherty, Busby-Whitehead Purpose: • Compare pelvic floor muscle exercises alone to PFME plus biofeedback in women with stress and mixed urge and stress UI • Design – 315 women randomized to 3 groups, including an attention control group – Followup up at 2 weeks, 6 months, 1 year University of North Carolina School of Medicine Center for Aging and Health Drug Treatment for UI: What Works • Stress UI – Alpha adrenergic agents? – Estrogen? – Combination therapy? University of North Carolina School of Medicine Center for Aging and Health Alpha Adrenergic Drugs • Phenylpropanoloamine – – – – – • Once a first line drug 8 randomized controlled trials Study duration: 2-6 weeks % cure: 0-14 % side effects: 5-33% WITHDRAWN FROM MARKET due to report of hemorrhagic stroke University of North Carolina School of Medicine Center for Aging and Health Duloxetine (Cymbalta) • FDA application for stress UI withdrawn • Warning for liver dysfunction, alcohol University of North Carolina School of Medicine Center for Aging and Health Estrogen • Combined study with Phenylpropanolamine suggested improvement in combination • Improves urogenital atrophy • Heart and Estrogen/Progestin Replacement Study 2001: 4 yr, randomized trial, 2763 postmenopausal women <80 given combined HRT or placebo for ischemic heart disease. – 55% had >1 episode UI/week – HRT group had worsening stress and urge UI sx University of North Carolina School of Medicine Center for Aging and Health Drug Treatment of Overactive Bladder • Anticholinergic Drugs are mainstay – Oxybutynin IR 2.5-5 mg bid-qid – Ditropan XL 5-20 mg daily – Oxytrol patch TDS 3.9 mg 2x/wk – Tolterodine tartrate IR 1-2 mg bid – Detrol LA 2-4 mg daily New Drugs: – Trospium chloride (Sanctura) 20 mg bid – Darifenicin (Enablex) 7.5-15 mg daily – Solefenicin (Vesicare) 5-10 mg daily University of North Carolina School of Medicine Center for Aging and Health Muscarinic Receptors • M1 – Brain (cortex, hippocampus), salivary • glands, sympathetic ganglia • M2 – Heart, hindbrain, smooth muscle (80% of detrusor) • M3 – Smooth muscle (20% of detrusor), salivary glands, brain, eye (lens, iris) • M4 – Brain (forebrain, striatum) • M5 – Brain (substantia nigra), eye University of North Carolina School of Medicine Center for Aging and Health Hepatic metabolism • Oxybutynin CYP 3A4 • Tolterodine CYP 3A4, CYP 2D6 • Darifenacin CYP 3A4, CYP 2D6 • Solifenacin CYP 3A4 • CYP 3A4: Interactions with macrolides, ketoconazole, nefazadone • CYP 2D6: interactions with TCAs, fluoxetine University of North Carolina School of Medicine Center for Aging and Health Behavioral vs Drug Rx for Urge UI in Older Women • Randomized, controlled trial by Burgio et al JAMA 1998; 280; 1995-2000 • 197 women aged 55-92 • 8 weeks of BFB, 8 weeks of oxybutynin • 2.5 to 5 mg qd to tid, or placebo control • All 3 groups reduced UI frequency • Effectiveness: BFB>drug>placebo University of North Carolina School of Medicine Center for Aging and Health Burgio et al JAMA 1998; 280:1995-2000 16 14 12 10 Leaks per 8 week 6 Pre Post 4 2 0 Behavioral Control University of North Carolina School of Medicine Center for Aging and Health Oxybutynin • Both anticholinergic and smooth muscle relaxant properties • 6/7 RCTs show benefit • 15-58% greater reduction in urge UI than placebo • Dose: 2.5 -5 mg qd-qid, 20 mg/d maximum University of North Carolina School of Medicine Center for Aging and Health Oxybutynin Controlled Release • Once daily dosing • RCT showed rate of daytime continence similar to that for immediate release (53 vs 58%) • Lower rate of dry mouth than immediate release form University of North Carolina School of Medicine Center for Aging and Health Tolterodine tartrate • Pure muscarinic receptor antagonist • Dry mouth most common side effect • 3 RCT compared tolterodine (2 mg bid) to oxybutynin (5 mg tid): Equally effective and superior to placebo • Decreased urge U(I in study of 293 pts:47% tolterodine, 71% oxybutynin, 19% placebo, dry mouth 86% oxybutynin, 50% tolerodine University of North Carolina School of Medicine Center for Aging and Health OBJECT Study Appel et al Mayo Clin Proc 2001:76 • Compared efficacy and tolerability of extended release oxybutynin and tolterodine tartrate • 12 weeks • Prospective randomized,double-blind, parallel group study • 276 women and 56 men • Oxybutynin more effective for weekly urge UI, total incontinence, and urinary frequency University of North Carolina School of Medicine Center for Aging and Health Trospium • Dose 20 mg bid • Renal metabolism • Nonselective for muscarinic receptors • Effective for detrusor overactivity in placebocontrolled double-blind studies: • Trospium 20 mg bid vs tolterodine 2 mg bid in 232 pts reduced voiding frequency and number of UI episodes • Dry mouth 7% and 9% respectively University of North Carolina School of Medicine Center for Aging and Health Darifenicin • Dose 7.5 to 15 mg daily • Selective M3 receptor antagonist • Several RCTs • Mundy et al 2001 Randomized double-blind trial compared darifenacin 15 mg and 30 mg to oxybutynin 5 mg tid in 25 pts , similar efficacy • Side effects: Dry mouth, constipation(<2%) University of North Carolina School of Medicine Center for Aging and Health Solefenacin • Dose 5 to 10 mg daily • Long acting muscarinic receptor antagonist, selective for M3 • Undergoes hepatic metabolism involving cytochrom P450 • Several multinational trials with over 800 pts, vs placebo, showed efficacy low side effects (2% dry mouth) University of North Carolina School of Medicine Center for Aging and Health Urinary retention Gastric retention Cardiac arrhythmias Contraindications for Anticholinergics Bladder outlet obstruction Narrow angle glaucoma University of North Carolina School of Medicine Center for Aging and Health Desmopressin • Decreases urine production • Helps nocturia • Dose: 20-40 mcg intranasal spray q hs • Double-blind crossover trial showed decreased nighttime voids vs placebo, 1.9 vs 2.6 • Contraindications: CHF, HTN, ASCVD University of North Carolina School of Medicine Center for Aging and Health Functional Electrical Stimulation • Frequency of 10-50 Hertz for 15-20 minutes daily • RCT: 50% cured after 8 weeks compared to sham controls • 52-77% symptomatic improvement in short-term studies, non RCT • Implantable electrodes at S2-3, 76% improvement for refractory urge UI x 18 mo • BUT 33% required surgical revision University of North Carolina School of Medicine Center for Aging and Health Surgery for Urge/OAB • If behavioral and pharmacological treatments don’t work • Augmentation enterocystoplasty • One series of 267 patients had a 93% continence rate with 3 yr f/u • Complications: urinary retention, stones, small bowel obstruction, reservoir rupture University of North Carolina School of Medicine Center for Aging and Health Treatment of Overflow UI Due to Mild BPH • Alpha adrenergic antagonists – Possibly relaxes prostate smooth muscle and stroma and urethra smooth muscle to increase urine flow – Tamsulosin, doxazosin, terazosin – Tamsulosin trials: 53 weeks, 31% and 36% improvement in maximal flow rate with 0.4mg and 0.8 mg/day vs 21% placebo – Uroselective alfuzosin in late stage clinical trials University of North Carolina School of Medicine Center for Aging and Health Drug Treatment of Mild BPH • Type II 5 alpha reductase inhibitor – Results in atrophy of the prostatic glandular epithelium due to decreased synthesis of dihydrotestosterone – Slow onset, 20-30% reduction in prostate volume and LUTS over time – Side effects: Ejaculatory dysfunction (8%), loss of libido (10%), erectile dysfunction (16%) – Finasteride , Dutasteride University of North Carolina School of Medicine Center for Aging and Health Summary • Behavioral treatment is effective for treating stress and urge UI and OAB • Drugs are effective for treating urge UI and OAB and mild BPH • New selective agents for urge and OAB based on new understanding of bladder and urethral function • Caution needed in dosing, especially in older patients University of North Carolina School of Medicine Center for Aging and Health