LPN-C - Faculty Sites
advertisement

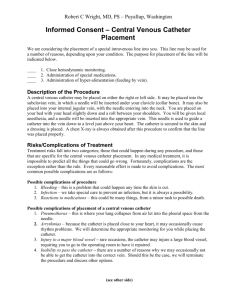
LPN-C Unit Five Peripheral Intravenous Therapy Nursing Interventions R/T Anxiety & Discomfort with IV Infusion Individuals typically experience anxiety related to intravenous therapy ◦ Illness ◦ Unfamiliar environment ◦ Need for complex services and procedures Extreme anxiety can have physiological effects ◦ Spasm or constriction of veins due to the sympathetic response Blood shunted from peripheral circulation to vital organs Inhibits venous access ◦ Syncope related to the vasovagal response Anxiety & Discomfort (cont’d) Psychological preparation increases coping ability ◦ Relaxes the client ◦ Facilitates initiation of IV therapy for the nurse Client teaching ◦ Time Building rapport and relaying caring Allowing time for questions ◦ Explanations Overcoming communication barriers ◦ Honesty How long the IV may be in place Why IV access is needed Acknowledge associated pain and discomfort Anxiety & Discomfort (cont’d) Pain reduction ◦ Advise patient of measures that may decrease distress ◦ Assure patient that you will be as efficient as possible ◦ Employ appropriate physical, pharmacological, and psychological measures to minimize discomfort Professionalism ◦ Express confidence and expertise ◦ Reinforce positive aspects of the procedure Latex Allergy Precautions Patients at risk for latex-related reactions – ◦ ◦ ◦ ◦ ◦ Women constitute 75% of all reported cases Asthma Allergy history Occupational exposure to latex Fruit and vegetable allergies Avocados Bananas Chestnuts Kiwis and other tropical fruits ◦ Intermittent catheterization ◦ Chronic genitourinary or abdominal conditions requiring multiple surgeries Latex Allergy Precautions (cont’d) Report incidents of adverse reactions to latex or other materials used in medical devices to the FDA FDA recommendations to health professionals - ◦ Assess latex sensitivity while obtaining history for all patients ◦ Use devices made with alternative materials ◦ Be alert for an allergic reaction whenever latexcontaining devices are used, especially when in contact with mucus membranes ◦ Alert clients with suspected allergic reaction to latex to possible latex sensitivity, and advise them to consider immunologic evaluation Latex Allergy Precautions (cont’d) FDA recommendations to health professionals (cont’d) -◦ Advise clients to tell health professionals and emergency personnel about latex sensitivity ◦ Consider advising clients with a latex allergy to wear a medical identification bracelet Other allergies ◦ Must assess for allergies to foods, animals and insect matter, and environmental substances ◦ Iodine Often used in skin antisepsis Client may only recognize this as a shellfish allergy ◦ Adhesive Used in dressing tape Caring for an IV at Home Many clients receive IV therapy at home ◦ Limitations by 3rd party payers ◦ Personal preference Several types of IV therapy can be maintained outside of the hospital ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Antibiotics Chemotherapy Hydration and hyperalimentation Pain control HIV-related therapies Growth hormone and immunoglobulins Dobutamine (for severe CHF) Tocolytic therapy (to ↓ premature contractions) Caring for an IV at Home (cont’d) Arm/hand movement may be limited, so client may need to relearn ADLs Ambulation with infusion equipment Instruct client against tampering with IV tubing, clamp, or dressing Advise client to keep the IV dry to minimize risk of infection ◦ Staphylococcus epidermis ◦ Staphylococcus aureus Teach client how to assess IV site for signs and symptoms of infection Provide list of symptoms or conditions for which client would need to call the doctor IV Preparation *Physical preparation of the client for initiation of intravenous therapy includes safety, comfort, and positioning Safety ◦ Verify IV order ◦ Verify correct patient identification ◦ Validate that the ordered infusion is appropriate for the patient ◦ Confirm that the patient is not allergic to anything that is to be administered ◦ Review documentation of significant laboratory and diagnostic reports ◦ Maintain strict asepsis when preparing all products to be used for venipuncture/infusion IV Preparation (cont’d) Safety (cont’d) -- ◦ Ensure that all supplies and equipment for venipuncture are sterile ◦ Check expiration dates ◦ Provide a safe environment for the patient during infusion therapy Bedrails Restraints Movement Ambulation ◦ Assess/select the vessel that is appropriate for the type of infusion ordered ◦ Instruct the client about what to report in terms of activity, discomfort, or signs/symptoms associated with a reaction Comfort IV Preparation (cont’d) ◦ Restrictions in mobility and sustaining ADLs Prevent dislodgement of the cannula Avoid disconnection of any part of the infusion setup If any portion of the closed IV system were disrupted, contamination and infection could occur ◦ Use nondominant hand for IV access ◦ Avoid using veins in areas of flexion unless immobilized ◦ Allow completion of ADLs prior to IV insertion ◦ Provide loose-fitting clothing/hospital gown Allows for less restricted movement Does not impede fluid flow Easily removed for changing ◦ Provide for privacy IV Preparation (cont’d) Correct positioning ◦ Fowler’s position ◦ Maintain intended venipuncture site below heart level to promote venous filling ◦ Follow institutional protocol with regards to armboards, restraints, or stabilization devices Can cause nerve and muscle damage Must be removed at frequent intervals to assess circulatory status ◦ Protect insertion site from moisture and contamination ◦ Hair may need to be removed prior to initiating IV therapy if it impedes vessel visualization, site disinfection, cannula insertion, or dressing adherence IV Preparation (cont’d) Correct positioning (cont’d) – ◦ Hair removal (cont’d) – Hair is to be removed by gently clipping it close to the skin Do not scratch the skin Do not shave the hair because of the potential for microabrasion and the introduction of contaminants Do not apply depilatories due to the possibility for skin irritation or allergic reactions An electric shaver may be used Check your institutional policy If the shaver does not belong to the patient, the shaving heads would need to be changed or disinfected between patient use IV Preparation (cont’d) *IV preparation involves using the correct site preparation/maintenance materials Obtain the appropriate dressing materials ◦ Sterile gauze ◦ Sterile transparent, semipermeable dressing Cleanse the skin ◦ Use an antimicrobial barrier 2% chlorhexidine or per institutional policy Available in the form of swab sticks, prep pads, or plastic, cotton-tipped squeezable vials These are one-time use only! ◦ Allow barrier to air dry Vein Selection *Intravascular access refers to entrance into arteries, veins, or capillaries The selected access site should provide the most appropriate access to the vessel ◦ Needs to be appropriate for intended therapy ◦ Must accommodate administration of the prescribed infusion ◦ Endeavor to minimize associated risks or complications Factors to consider with vein/site selection ◦ Patient’s age, health status, and diagnosis ◦ Condition of the site to be accessed ◦ Purpose, duration, and possible side effects of therapy Vein Selection (cont’d) *Peripheral intravenous routes should be achieved in an upper extremity Venous cannulation should begin at the distal-most area of the upper extremity and proceed proximally Examine the upper extremities ◦ Predict the ease or difficulty of venous access ◦ Predetermine measures to facilitate successful venipuncture Inspect the patient’s skin ◦ Assess for damaged areas ◦ Apply a tourniquet ◦ Use a flashlight for enhanced visualization Vein Selection (cont’d) *Peripheral intravenous routes (cont’d) – Palpate the patient’s veins ◦ Determine condition of the vessel ◦ Locate deeper, larger veins that are stronger and more suitable for initiation of IV therapy *The nurse needs to know which veins to avoid when preparing to perform venipuncture for purposes of peripheral intravenous therapy Do not use veins in an area with a recent infiltration Do not use veins in an area that has sustained 3rd degree burns Vein Selection (cont’d) *Veins to avoid (cont’d) – Avoid veins in the antecubital fossa Do not use veins that are irritated or sclerosed from previous use ◦ For a vein to be viable, it must be able to be blanched ◦ To check for blanching, apply downward pressure over, or on each side of, a vein ◦ If the vein disappears with the pressure, then reappears when the pressure is removed, the vein is viable ◦ A sclerotic vein will not blanch Avoid veins in an extremity that is partially amputated Vein Selection (cont’d) *Veins to avoid (cont’d) – Do not use veins in the lower extremities in ambulatory adults and children ◦ Use lower extremity sites only in an emergency ◦ Must have a written order ◦ Ensure agency has policy in place that upholds this procedure Never access an arteriovenous fistula, graft, or shunt that has been surgically placed for hemodialysis ◦ Do not use the affected arm itself for IV therapy Do not use veins in an extremity that is impaired as a result of a CVA Vein Selection (cont’d) *Veins to avoid (cont’d) – Do not use veins on the side of the body where a radical mastectomy with lymph node dissection/stripping has been performed Bypass veins in an extremity that has undergone reconstructive or orthopedic surgery Avoid edematous extremities Cannula Selection *Types of peripheral venous devices Steel needles Winged needles Catheters *Steel needles are very rarely used anymore *Winged needles, referred to as butterflies, have one or two “wings” Connect with a needle on one side and a segment of infusion tubing that ends in a hub and protective cap on the other ◦ Tubing varies in length from 3½ to 12 inches ◦ Tubing is primed with NS prior to insertion to prevent entry of air into the circulation Cannula Selection (cont’d) *Butterflies (cont’d) – Wings are held upright during insertion to facilitate movement into the vein Once the needle is in the vein, the wings are taped to the skin to secure the device If secured properly, winged needles stay in the vein well Good means of venous access under certain circumstances ◦ ◦ ◦ ◦ Short-term infusions (24 hours or less) Seldom used for adult infusion therapy Can be used for one-time IV push medications May be used to draw blood Cannula Selection (cont’d) *Peripheral venous access catheters are the most commonly used IV device Used to enter superficial or deep veins ◦ Extremity ◦ Neck ◦ Head Two-part flexible cannula in tandem with a rigid needle or stylet ◦ Stylet is used to puncture and insert the catheter into the vein ◦ Connects with a clear chamber Allows for visualization of blood return Indicates successful venipuncture Facilitates removal of the needle Cannula Selection (cont’d) *Catheters (cont’d) - Color-coded plastic cannula hub ◦ Indicates length and gauge of catheter Length ranges from ¼ inches to 12 inches Catheter is radiopaque ◦ Easily detected by radiology in case of embolus *Types of catheters include the over-theneedle peripheral catheter (ONC) and the through-the-needle peripheral catheter (TNC) The ONC is a flexible cannula that encases a steel needle or stylet device ◦ Most commonly used peripheral IV device Cannula Selection (cont’d) *Types of catheters (cont’d) - ONC (cont’d) – ◦ Once the vein is accessed, the catheter is threaded into the vessel and the stylet is withdrawn The TNC is the opposite of the ONC, as the flexible cannula is encircled by the steel needle ◦ Infrequently used ◦ The needle is withdrawn once venous access is achieved ◦ Secured in a protective shield outside the body on the skin Cannula Selection (cont’d) *Factors to consider when selecting a cannula – Use the smallest cannula that will deliver the prescribed infusate ◦ Adequate blood flow and hemodilution ◦ Causes minimal discomfort Delivery rate ◦ ◦ ◦ ◦ 24 gauge cannula → approx 15-25mL/min 22 gauge cannula → approx 26-36mL/min 20 gauge cannula → approx 50-65mL/min 18 gauge cannula → approx 85-105mL/min Achieving Venous Distention Apply a tourniquet ◦ A tourniquet is an encircling device consisting of a segment of rubber tubing that temporarily arrests blood flow to or from a distal vessel ◦ Apply tightly enough that venous blood flow is suppressed, but not so tight that it obstructs arterial flow Should be able to palpate pulse distal to the tourniquet ◦ Do not leave a tourniquet in place longer than four to six minutes Tourniquet paralysis from injury to a nerve can occur if the tourniquet is applied too tightly or left for too long a period Apply warm compresses for 10-15 minutes Achieving Venous Distention (cont’d) Place the extremity intended for venipuncture below the level of the patient’s heart for several minutes Have the patient open and close his or her fist, or squeeze and release the lowered bedrail Use an alcohol pad to gently rub the skin over the vein intended for venipuncture ◦ Alcohol and friction creates heat ◦ Enhances venous distention Pat the area of skin over the intended vein using light to moderate force to engorge the vein with blood IV Equipment and Supplies *Infusate containers and IV administration sets Infusate containers – ◦ Flexible plastic ◦ Semirigid plastic ◦ Glass IV administration set = tubing that delivers fluid/medication from the infusate container to the patient *All administration sets have a spike insert that fits into the administration set port of the infusate container, as well as a drip chamber, clamps, and an adapter IV Administration Sets On an administration set, the drip chamber is where the solution flows after leaving the infusate container and before entering the tubing A screw and roller clamp allows for flow regulation A slide clamp functions as an on-off clasp A cannula hub can be attached to the sterile adapter at the end of the tubing ◦ The adapter can be straight, fitting directly into the cannula hub with a push ~OR~ ◦ The adapter can be screwed on to the cannula hub, providing a firm attachment (Luer-Lok) IV Administration Sets (cont’d) The administration set determines the rate at which fluid can be delivered to the patient (i.e. the drop factor) Specialized tubings are used in specific settings and circumstances ◦ Extra large (macrobore) tubings Used in emergency surgical and trauma situations Rapid infusion of large volumes of blood or fluid ◦ Extra small (microbore) tubings Used for the delivery of small amounts of precisely controlled fluid or medication Special volume restriction (neonatal care, epidural infusions) IV Administration Sets (cont’d) Types of administration sets: ◦ Vented systems Used for vacuum infusate containers that don’t have their own built-in mechanisms for air displacement Glass and some semirigid bottles ◦ Nonvented systems Used with flexible plastic bags and other nonvacuum receptacles ◦ Primary administration sets ◦ Secondary administration sets *Primary administration sets are also known as basic, or standard, sets Carries fluid directly to the patient through one tube IV Administration Sets (cont’d) *Primary administration sets (cont’d) - Spiked into one (single line) or two (Y-type) main infusate container(s) May terminate in straight, flashtube, or Luer-Lok male adapters Available in macrodrip or microdrip in varying lengths Available with or without check valves, which prevent retrograde blood flow May contain one or several injection ports Can accept attachments ◦ Secondary administration tubings, extension tubings, flow control devices, filters, adapters IV Administration Sets (cont’d) *Single line primary administration sets have one spike that is inserted into one infusate container; the tubing terminates with an adapter that connects to the cannula hub at the IV access site *Y-type primary administration sets have two equal-length tubings that can each access an infusate container Access can be simultaneous or alternately ◦ Each tubing has its own roller clamp ◦ Each tubing may or may not have its own drip chamber Frequently used in emergency, surgical, and critical care situations IV Administration Sets (cont’d) *Y-type administration sets (cont’d) – The solution reaches the patient via one common tubing ◦ Necessitates compatibility between the infusates Blood administration tubings are Y-type sets, but differ from standard Y-type primary administration sets Should be used only with nonvacuum, flexible infusion containers where venting is unnecessary ◦ If vented containers are used, air can be drawn into the circulatory system, resulting in an air embolism IV Administration Sets (cont’d) *Secondary administration sets are referred to as piggyback sets Used to deliver continuous or intermittent doses of fluid or medication Widely used because they negate the need for additional venipunctures and interruption of the primary infusion Usually connected with a needle or needleless adapter into an injection port immediately distal to the back-check valve of the primary tubing Some primary administration sets have a closed-system connection to a second line IV Administration Sets (cont’d) *Whenever an infusion line is breached, the possibility for introduction of contaminants exists IV line should not be broken to add accessory equipment unless absolutely necessary Refer to your institution’s policy for adding equipment such as filters, extension sets, adapters, and connectors to infusion lines *Needleless systems and needlestick safety systems are state-of-the-art in IV therapy Used to connect IV devices, administer fluids and medications, and sample blood IV Administration Sets (cont’d) *Needleless systems (cont’d) – Eliminates up to 80% of needles ◦ Other than the initial stick to insert the cannula into the patient’s vein, there is no need for needles during IV therapy *Blood exposure protocol – ◦ Wash needlestick punctures with soap & water ◦ Flush splashes to the nose, mouth, or skin with water ◦ Irrigate splashes to the eyes with clean water, NS, or sterile ophthalmic irrigants ◦ Report the incident to the department responsible for managing exposures ◦ Start post-exposure treatment ASAP Mechanical Gravity Control Devices *Mechanical gravity control devices are flowregulating mechanisms that attach to the primary infusion administration set Manually set to deliver specified volumes of fluid per hour Available as dials or cylindrical controls Includes approximate flow markings that must be verified (i.e. counting gtt/min) Accuracy varies ◦ Discrepancies can be up to ± 25% ◦ Dependent upon patient’s condition, activity level, positioning, and venous pressure Mechanical Gravity Control (cont’d) Should generally be used for only short periods, such as transporting the patient ◦ IV tubing kinking/obstruction can restrict fluid flow ◦ Must be checked frequently for infusion accuracy Electronic Infusion Control Devices (EID) *EIDs are state-of-the-art infusion-regulating mechanisms that deliver fluids and medications Powered by electricity and/or battery Safe and accurate (± 5%) Programmable for several infusates at different rates and volumes at the same time Sensors detect air in the line and pressure changes Signals infusion termination Alerts the nurse to problems via readouts, alarms, and flashing lights EIDs (cont’d) Most newer EID models have built-in safety flow mechanisms ◦ Prevents unintended free flow of infusate into the patient if the administration set were to be removed from the machine NOTE: No EID is a substitute for regular patient observation and evaluation Initiation of Infusion Therapy *Gather the necessary equipment/supplies to be optimally prepared for venipuncture Check the order ◦ Identify that the order is for the right patient Read the label on the infusate container to verify correct medication and dose ◦ Container should be compared directly with the physician’s order to be sure it is correct ◦ Verify pharmacy admixtures Verify infusate compatibility Check the expiration date of the infusate Evaluate the infusate container to ensure seals are intact Initiation of Infusion Therapy (cont’d) *Gather equipment/supplies (cont’d) – Check the infusate fluid for clarity and presence of particulate matter *Equipment preparation and setup should be completed away from the patient’s room in an environment that minimizes the chance for contamination Prior to starting an infusion, the correct infusate should be set up with a primary administration set If secondary infusions are ordered or anticipated, choose a primary set with a check valve and injection ports Initiation of Infusion Therapy (cont’d) *Equipment preparation(cont’d) – The interior of the tubing, both ends of the tubing, and the infusate must be kept sterile NOTE: The nurse must obtain permission from the adult patient before performing venipuncture or it may constitute assault and battery Step 1 Step 2 Step 3 Step 4 Step 5 Step 6 Step 7 Step 8 Venipuncture Introduce yourself to the patient Ask the patient to state his/her full name, verifying identity with chart and ID bracelet Provide privacy Explain proposed procedure in terms the patient can understand Elevate the bed to prevent strain Place the patient in a semiFowler’s or Fowler’s position Protect clothing/bedding with a pad or towel Wash your hands Venipuncture (cont’d) Step 9 Step 10 Step 11 Step 12 Step 13 Step 14 Set up all necessary supplies near the bed in the order they will be used Select an appropriate vein based on the type of therapy and anticipated duration Apply a tourniquet 2-3 inches below the antecubital fossa for venous access in the arm or hand Prepare the site Apply gloves while the final antiseptic is drying Cannulate the vein Catheter Immobilization Once in place, the IV device must be secured ◦ Must allow for regular site assessment ◦ Need to prevent cannula movement or dislodgement ◦ Maintain asepsis ◦ Prevent catheter-related infection Transparent, semipermeable dressings are most common ◦ ◦ ◦ ◦ Secures the vascular access device Allows for continuous visual inspection of site Allows bathing without saturating the dressing Requires less frequent changes than others Special Considerations Patients with altered skin and vessels ◦ Burns, fragile veins ◦ Do not use a tourniquet ◦ Use alternative measures per institutional policy for skin antisepsis to prevent further irritation and discomfort Patients with peripheral edema ◦ May need to use landmarks to identify a vein ◦ Client is at risk for unidentified infiltration due to edema ◦ Vein may collapse due to pressure from excess fluid Obese patients ◦ May have deeply imbedded vessels Special Considerations (cont’d) Obese Patients (cont’d) -◦ May need to use landmarks to identify a vein ◦ May need to employ a longer cannula to reach an appropriate vein Patients receiving anticoagulant therapy ◦ Avoid using a tourniquet, or, if necessary, apply as loosely as possible ◦ Avoid excess pressure when applying the skin preparation ◦ Use the smallest cannula that will accommodate the vein and deliver the ordered infusate ◦ Remove dressings gently and use an adhesive solvent Converting a Peripheral IV Converting a peripheral IV to an intermittent access device is necessary when discontinuing peripheral infusions while retaining venous patency ◦ IV access remains available in case it is needed ◦ Administration of intermittent medications Conversion is completed by attaching an intermittent infusion plug to the hub of the cannula ◦ Also called a male adapter plug ◦ Formerly referred to as a heparin lock Heparin is no longer recommended for intermittent flushing because bacterial growth on the catheter may be intensified in its presence Converting a Peripheral IV (cont’d) Intermittent line maintenance is achieved by assessing the IV site, checking for cannula patency, and flushing with 2cc NS every 8-12 hours Check for patency of the intermittent line by attaching the syringe to the intermittent plug and pulling back the plunger to elicit blood return ◦ If there is no blood return, gently inject the saline while palpating the infusion site If the cannula is out of the vein, the saline will infiltrate the surrounding tissue, causing it to rise and be cool to the touch If the cannula is placed correctly, the saline will enter the cannula and vein, maintaining patency Converting a Peripheral IV (cont’d) When any medication is administered into an intermittent infusion device, the protocol to be followed is the S-A-S method ◦ Slowly instill 2mL NS to clear the lock (S) ◦ Administer the prescribed medication (A) ◦ Flush with NS to clear the lock (S) Prior to implementing the S-A-S method – ◦ ◦ ◦ ◦ ◦ Wash your hands Assess the IV access site Don gloves Disinfect the cannula port Verify cannula and venous patency If resistance is met, do not exert pressure on the syringe plunger to restore patency Converting a Peripheral IV (cont’d) Multiple medication orders – ◦ Instill NS between the administration of each medication ◦ Always flush with NS after all medications are injected in order to clear the cannula and maintain patency Maintain positive pressure during and after saline flushes ◦ Achieved by withdrawing the blunt cannula or needle as the last 0.5mL of NS is flushed inward ◦ Prevents the reflux of blood Adding a Fluid/Medication *During infusion therapy, fluids or medications can be added in the following ways – Added to the primary infusate container Via secondary administration set Through an injection port in the primary administration tubing By direct injection into a vein that is not concurrently receiving infusates (bolus) NOTE: For all but the last method, the nurse must check for chemical, physical, and therapeutic compatibility between the medications and delivery systems Adding a Fluid/Medication (cont’d) Adding fluid/medication to the primary infusate container – ◦ This is usually done as an admixture by the pharmacy under asepsis ◦ If the nurse would need to add a medication, you would need to check for compatibility, additive concentration, and stability of the new solution ◦ Never add a medication to an existing infusion container while it is hanging and infusing Drug would be delivered to the base of the container Bolus dose would be infused to the patient May result in serious complications, or even death Adding a Fluid/Medication (cont’d) Adding fluid/medication via secondary administration set (piggyback) – ◦ This method involves administering a medication or fluid that is initiated after the primary infusion is already in progress ◦ This is the most common means to administer intravenous medications concurrently with the primary infusion ◦ The piggyback line is coupled to the primary infusion line at the first injection port below the check valve ◦ The secondary infusion is able to function concurrently with the primary infusion only when suspended higher than the primary line Adding a Fluid/Medication (cont’d) Adding fluid/medication via piggyback (cont’d) – ◦ The primary line must have a back-check valve ◦ By opening the clamp on the secondary line, the primary infusion temporarily stops flowing ◦ When the piggyback infusion is complete and the infusate in its tubing falls below the level of the primary line drip chamber, the back-check valve opens and the primary infusion resumes Adding a Fluid/Medication (cont’d) Adding fluid/medication through an injection port in the primary administration tubing – ◦ This is termed an IV push medication ◦ Intravenous medications that would normally be delivered directly into the vein by bolus injection can be delivered through an injection port in the primary administration set if the patient already has a running IV ◦ The nurse must check for compatibility between the product already and the drug to be administered by IV push Failure to do so could cause a precipitate to form Precipitate could obstruct the infusion line, damage the vein, or embolize Nonfunctioning IV Lines *Checklist for determining the cause of a nonfunctioning peripheral IV line – Check IV site for infiltration, patency Check the infusate container ◦ Fluid level ◦ Height Check the tubing for kinking Check the air vent and filter Ensure the clamp is open Check the positioning of the patient Check the temperature of the solution Ensure the tubing is correct for the infusate Documentation *IV documentation includes labeling The main purpose for labeling is to denote IV start, stop, and discontinuation times Labels must be affixed to infusate containers, administration set tubing, and dressing sites Placement of labels ◦ IV site Place next to the dressing Include the date and time of cannulation Indicate the type of device used Length Gauge Identification (nurse’s initials) Documentation (cont’d) Placement of labels (cont’d) -◦ Allergy labels On and in the patient’s chart In the patient’s room and on the patient’s bed All communication with other personnel and departments regarding allergies and drug reactions Attach appropriate identification bracelet to the patient ◦ Administration set tubing Include date and time of initiation/change ◦ Infusate container(s) Start date and time Flow level strips Added medications Never write directly on an IV bag (use label instead) Documentation (cont’d) *Accurate charting for intravenous infusions should include these components – Date and time of insertion Which vein was cannulated ◦ Be specific (know your peripheral venous anatomy!) ◦ Document why you chose a particular vein if necessary ◦ Document the condition of the vein in terms of its softness or hardness and resiliency Device used ◦ Brand name and style ◦ Gauge and length Documentation (cont’d) What to include in your charting (cont’d) – Infusate administered ◦ Name of medication/fluid ◦ Rate of infusion Method of infusion ◦ Gravity ◦ EID Controller or pump mode Name brand and model number Type of dressing applied Remedial information ◦ Number/location of attempted cannulations ◦ Condition of the failed site(s) Documentation (cont’d) What to include in your charting (cont’d) – Patient’s response to the procedure ◦ Reaction/comments *Be sure to document in these areas - MAR Nurse’s notes Infusion and equipment flow sheets Nursing care plan Intake and output records Laboratory, radiology, and other ancillary department requisitions Local and Systemic Complications of IV Therapy Local Complications of IV Therapy Local complications = adverse reactions that occur at or close to the IV insertion site ◦ Constitutes the majority of complications in IV therapy ◦ Usually less serious than systemic problems *Types of localized infusion-related complications include infiltration, thrombosis, phlebitis, thrombophlebitis, and allergic reaction to the IV catheter *Infiltration refers to the inadvertent administration of nonvesicant solution into the surrounding tissue Local Complications (cont’d) Causes of infiltration ◦ ◦ ◦ ◦ ◦ Dislodgement of the cannula from the vein Puncture of the vein wall during venipuncture Friction of the catheter against the vein wall Use of a high pressure infusion device Irritating infusate that weakens the veins Signs and symptoms of infiltration ◦ ◦ ◦ ◦ ◦ Skin is taut and/or cool to the touch Dependent edema Absence of blood backflow Pinkish blood return Slowing of the infusion rate Local Complications (cont’d) Infiltration complications ◦ Ulceration may appear after days/weeks ◦ Compartment syndrome Fluid builds up inside an inflexible compartment Pressure on nerves, muscles, and vessels Functional muscle changes occur within 4-12 hours Ischemic nerve damage occurs within 24 hours Preventing infiltration ◦ ◦ ◦ ◦ Assess IV site (blood return is not an indicator) Pain may or may not be present Extremity comparison Infusion should stop running if pressure is applied 3 inches above the catheter site Local Complications (cont’d) Treatment of infiltration ◦ Infuse antidote through the IV if applicable, then remove the IV ◦ Apply warm compresses for antineoplastic agents, and cool compresses for most other medications ◦ Notify the physician ◦ Elevate the extremity if this promotes comfort for the patient *Extravasation is the inadvertent administration of vesicant medication or solution into the surrounding tissue Requires an incident report Local Complications (cont’d) Treatment of extravasation ◦ Dependent on a variety of factors Pharmaceutical manufacturer’s labeled uses and directions Properties and severity of extravasated agent ◦ Treatment determined before IV removed ◦ Do no apply excessive pressure to the site to avoid establishment of perfusion ◦ Ongoing observation and assessment of site (i.e. motion, sensation, circulation) ◦ Do not use extremity for subsequent IV placement ◦ Notify the physician Local Complications (cont’d) Infiltration documentation ◦ Use the INS Infiltration Scale Extravasation always graded at 4 ◦ Document written and verbal communication ◦ Chart nursing and medical interventions ◦ Document patient’s response to incident and treatment Drugs associated with extravasation necrosis include – Calcium chloride Dopamine Vincristine Calcium gluconate Vancomycin Streptozocin Infusion Nurses Society Infiltration Scale Criteria Grade 0 No symptoms 1 Skin blanched and cool to touch 1 inch edema Pain may or may not be present 2 Skin blanched and cool to touch 1 - 6 inch edema Pain may or may not be present 3 Skin blanched, translucent, and cool to touch Gross edema (>6 inches) Mild-to-moderate pain; possible numbness 4 Skin blanched, translucent, tight, discolored, and bruised Gross, deep, pitting edema *May have circulatory impairment and severe pain with infiltration of blood product, irritant, or vesicant Local Complications (cont’d) *Thrombosis occurs when blood flow through the vein is obstructed by a local thrombus ◦ If thrombosis is IV-related, it has resulted from injury to the endothelial cells of the venous wall ◦ Injury leads to platelet aggregation at the site of injury, which forms the thrombus ◦ Major complication of central venous catheters Signs and symptoms of thrombosis ◦ Earache or jaw pain ◦ Edema, redness at insertion site ◦ Tachycardia, tachypnea Local Complications (cont’d) S/S of thrombosis (cont’d) – ◦ ◦ ◦ ◦ Malaise Unilateral arm or neck pain Absence of pulse distal to the obstruction Digital coldness, cyanosis, and/or necrosis Treatment of thrombosis ◦ Never flush with force to remove an occlusion ◦ Discontinue IV and restart with a new catheter at a different site ◦ Notify the physician for assessment of circulatory status Local Complications (cont’d) *Phlebitis = inflammation of the vein ◦ Endothelial cells in the venous wall become irritated and rough, allowing platelets to adhere ◦ Capillary permeability increases, and protein leaks out into the interstitial space ◦ Area more susceptible to mechanical or chemical irritation Signs and symptoms of phlebitis ◦ ◦ ◦ ◦ ◦ Localized redness and swelling Warm and tender to the touch Palpable “cord” along the vein Sluggish infusion rate Increased temperature Local Complications (cont’d) Prevention of phlebitis ◦ Use of larger veins for hypertonic solution infusions ◦ Use of central line for long-term IV therapy ◦ Use of the smallest IV cannula appropriate for the ordered infusate ◦ Rotation of IV sites per agency protocol ◦ Change IV bag per agency protocol ◦ Appropriate stabilization of the catheter ◦ Correct venipuncture technique ◦ Good handwashing *Phlebitis is graded according to INS scale Infusion Nurses Society Phlebitis Scale Criteria Grade 0 No symptoms 1 Erythema (redness of the skin due to capillary congestion) Pain may or may not be present 2 Pain at access site Erythema and/or edema 3 Pain at access site Erythema and/or edema Streak formation Palpable venous cord 4 Pain at access site Erythema and/or edema Streak formation Palpable venous cord >1 inch in length Purulent drainage Local Complications (cont’d) *INS practice criteria for phlebitis requires established guidelines for treatment in Policy and Procedures Manual ◦ All vascular access sites should be routinely assessed for signs or symptoms of phlebitis ◦ Discontinue IV at first sign of phlebitis and remove the intravenous device ◦ Grade ≥2 report to physician and file incident report ◦ Observe peripheral catheter site for 48 hours after device has been removed ◦ Document incident, intervention, treatment, corrective action, and patient education Local Complications (cont’d) Types of phlebitis ◦ Mechanical ◦ Chemical ◦ Bacterial Causes of mechanical phlebitis ◦ Insertion of a cannula that is too small for the vein ◦ Improper taping of the cannula hub so that the catheter tip rubs the vein wall ◦ Manipulation of the catheter during infusion Causes of chemical phlebitis ◦ Excessively rapid infusion Local Complications (cont’d) Causes of chemical phlebitis (cont’d) – ◦ Infusion of irritating substances Acidic solutions (Dextrose, KCL, antibiotics) pH level falls the longer the solution is stored ◦ Improperly mixed medications ◦ Presence of particulate matter in the solution Causes of bacterial phlebitis ◦ ◦ ◦ ◦ Poor aseptic technique Incorrect cannula insertion procedure Inadequate stabilization of cannula hub Lengthy catheter dwell time Local Complications (cont’d) *Thrombophlebitis occurs when thrombosis is accompanied by inflammation ◦ May become obstructive if IV not discontinued Complications of thrombophlebitis ◦ Embolism ◦ Septicemia ◦ Acute bacterial endocarditis Causes of thrombophlebitis ◦ Use of leg veins for venipuncture ◦ Use of hypertonic or highly acidic infusates Signs and symptoms of thrombophlebitis ◦ Local tenderness and warmth Local Complications (cont’d) S/S of thrombophlebitis (cont’d) – ◦ ◦ ◦ ◦ ◦ ◦ Appearance of a red line above the IV site Hardening of the vessel Sluggish flow rate Edema in the limbs Diminished arterial pulses Mottling or cyanosis of the extremities Treatment of thrombophlebitis ◦ Notify the physician, remove IV catheter and restart in opposite extremity using new equipment ◦ Apply warm, moist compresses to the area for 20 minutes for comfort Local Complications (cont’d) Documentation of thrombophlebitis ◦ ◦ ◦ ◦ Chart all observable symptoms Document patient’s complaints/reactions Chart nurse’s actions Document information regarding new venipuncture *Allergic reaction to the IV catheter Symptoms include red streak over the vein Treatment of a localized allergic reaction ◦ Discontinue the IV ◦ Notify the physician ◦ Use different material for new IV in another site Systemic Complications of IV Therapy Septicemia Embolism ◦ Pulmonary ◦ Air ◦ Catheter Pulmonary Edema Speed Shock Allergic Reaction *Septicemia = a febrile disease caused by microorganisms in the circulatory system ◦ Major complication that occurs from cannula or infusate contamination Systemic Complications (cont’d) Signs and symptoms of septicemia ◦ ◦ ◦ ◦ Fever, flushing, profuse diaphoresis Altered mental status Nausea/vomiting, abdominal pain Tachycardia, hypotension Treatment of septicemia ◦ ◦ ◦ ◦ ◦ ◦ Monitor patient Culture IV catheter per order/agency protocol Administer antimicrobial therapy as ordered Administer oxygen if needed Administer IV fluids Observe for bleeding (all body orifices) Systemic Complications (cont’d) Prevention of septicemia ◦ ◦ ◦ ◦ Good handwashing Careful inspection of IV solutions Appropriate infusion site dressing Rotate IV sites *Pulmonary embolism is associated with IVrelated thrombus ◦ Dislodged from the wall of the vein ◦ Carried by the venous circulation through the right side of the heart to the pulmonary artery Signs and symptoms include shortness of breath, cyanosis, chest pain, tachypnea Systemic Complications (cont’d) Prevention of a pulmonary embolism ◦ ◦ ◦ ◦ Manage local complications immediately Do not apply pressure to regain IV patency Inspect medication/fluid for particulate matter Avoid venipuncture in lower extremities Treatment of a pulmonary embolism ◦ Position patient on the left side, trendelenburg ◦ Administer oxygen ◦ Transfer to ICU *Air embolism is most frequent in central lines, and results from small amounts of air in the circulatory system Systemic Complications (cont’d) Causes of an air embolism ◦ Incorrect IV insertion ◦ Excessive catheter manipulation ◦ Loose connections in the IV tubing Complications of an air embolism ◦ Accumulation of small bubbles forms larger bubbles that can block pulmonary capillaries ◦ Blockage may be fatal due to sudden vascular collapse Symptoms of an air embolism ◦ Cyanosis, hypotension, ↑ venous pressure ◦ Rapid loss of consciousness Systemic Complications (cont’d) Treatment of air embolism ◦ Immediately place the client on the left side with head down Air becomes trapped in the right atrium Prevents air from entering the pulmonary artery ◦ Administer oxygen ◦ Notify the physician ASAP ◦ May need to administer CPR *Catheter embolism can occur during catheter insertion if appropriate placement technique is not observed ◦ Catheter tip can shear off and become a freefloating embolus ◦ Can occur in both OTC and TNC Systemic Complications (cont’d) Treatment of catheter embolism ◦ Apply a tourniquet high on the extremity to impede venous flow ◦ Cardiac catheterization may be needed to remove the tip ◦ Notify the physician and radiologist ◦ Start an IV in the opposite arm to prepare for angiography for visualization Symptoms of catheter embolism ◦ ◦ ◦ ◦ Hypotension Tachycardia, chest pain Cyanosis Loss of consciousness Systemic Complications (cont’d) Prevention of a catheter embolism ◦ Never place an IV over a joint Flexing may cause the catheter to break If unavoidable, use splint to prevent bending Documentation of catheter embolism ◦ Vital signs, symptoms, level of consciousness ◦ Appearance of catheter upon removal *Pulmonary edema is caused by rapid administration of large volumes of fluid that leads to circulatory overload Prevention of pulmonary edema includes monitoring the patient frequently and using an EID for IV therapy Systemic Complications (cont’d) Symptoms of pulmonary edema ◦ ◦ ◦ ◦ Increased blood pressure Distended neck veins Shortness of breath, rales Orthopnea (sensation of breathlessness in the recumbent position) ◦ Copious frothy sputum *Speed shock = systemic reaction to rapid or excessive infusion that overloads the system; may result in cardiac arrest Symptoms of speed shock ◦ Flushing of the head and neck ◦ Severe headache, chest pain Systemic Complications (cont’d) Causes of speed shock ◦ Leaving the flow clamp open on the IV tubing ◦ IV pump programming error ◦ Incorrect drip rate calculation Prevention of speed shock ◦ Always dilute IV push medications to the appropriate concentration ◦ Always administer IV push medications over the amount of time recommended per agency protocol *Allergic reaction at the systemic level is considered a hypersensitivity reaction that can be mild or severe Systemic Complications (cont’d) Symptoms of an allergic reaction ◦ ◦ ◦ ◦ ◦ ◦ Localized pain, edema, and/or redness Wheezing, bronchospasm Headache Palpitations, agitation, confusion Intestinal cramping, nausea/vomiting Development may vary from rapid to delayed Treatment of an allergic reaction ◦ ◦ ◦ ◦ Stop the infusion Keep the vein open with NS Administer oxygen if needed Ensure emergency equipment is available Systemic Complications (cont’d) Complications of an allergic reaction ◦ Severe hypersensitivity to IV therapy Profound physiological response to an antigen Abnormal immune response to an allergen ◦ May include anaphylaxis *Anaphylaxis = severe allergic reaction ◦ Immune response to allergen ◦ Large quantities of histamine released ◦ Massive peripheral dilation occurs Decreased blood flow to vital organs ◦ May lead to shock and death within minutes if untreated Medication/Fluid Interactions *Incompatibility = unintended effects from mixing fluids and/or medications ◦ Action may be neutralized, intensified, or weakened ◦ Precipitation may occur Crystallization of particles Occlusion of the IV line Vessel injury *Significant drug-drug interactions involve medications that are incompatible with other products ◦ Sodium bicarbonate ◦ Phenytoin (Dilantin) Medication/Fluid Interactions (cont’d) *Drug-drug interactions (cont’d) – ◦ Aminoglycosides (gentamicin, neomycin) ◦ Digitalis glycoside ◦ Barbiturates Secobarbital (Seconal) Pentobarbital (Nembutal) Phenobarbital (Luminal) ◦ Chlordiazepoxide (Librium) ◦ Diazepam (Valium) ◦ Theophylline Infection Control ◦ 500,000 patients develop IV-related infections every year; of these, 30,000 individuals die as a result ◦ It is critically important to understand the ways in which IV-related infection can occur, and take action to prevent it ◦ The three interacting factors in infection control are 1) prevention, 2) control, and 3) eradication of the microbe ◦ The goal of infection control is to break the chain of infection ◦ If infection does occur, practitioner must identify the microbe, determine causative circumstances, use efficient means to eradicate it, and identify factors to prevent recurrence Agencies and organizations that set guidelines for infection control: Center for Disease Control and Prevention (CDC) in Atlanta, Georgia ◦ Investigates, develops, recommends, and sets standards for infection control practices ◦ Division of the Department of Health and Human Services (DHHS) Occupational Safety and Health Administration (OSHA) ◦ Enforcing agency that provides mandates to protect employees in all fields ◦ Policies regarding health care personnel are closely aligned with CDC guidelines Infection Control – Agencies and Organizations (cont’d) Infusion Nurses Society (INS) National Association of Vascular Access Network (NAVAN) The Association of Practitioners in Infection Control and Epidemiology, Inc. (APIC) The CDC Hospital Infection Control Practices Advisory Committee (HICPAC) ◦ New committee that meets annually ◦ Updates information for health care personnel in IV therapy and hand hygiene procedures Terms Related to Infection Process Infection = process in which a host is invaded by microbes that grow, reproduce, and cause injury Pathology = a substance capable of producing disease Disease = usually a result of infection Colonize = if disease doesn’t occur, the invading microbes could colonize (or reside in) the host, and the host becomes a carrier of the organism without clinical signs or symptoms Terms (cont’d) Virulence = the microorganism’s strength and ability to produce disease; the occurrence of infection depends the virulence of the microorganism and the ability of the host to defend itself against the invader; factors that affect the virulence of the microbe include: ◦ The ability to adhere to and/or penetrate skin and mucus membranes ◦ The ability to adhere to and/or proliferate on inanimate objects ◦ Ability to exude toxic substances ◦ Ability to resist phagocytosis ◦ Ability to mutate and multiply within the host ◦ Ability to grow and multiply in the presence of antibiotics and other medications Epidemiologic Triangle Host Living organism that allows the microorganism to live Interacting conditions, surroundings, and/or influences in which the host and agent co-exist Agent Environment The microorganism that is capable of disease The Chain of Infection For an infection to occur, the 3 components of the epidemiologic triangle must be present An interacting chain of events must occur before infection will be transmitted There are 6 links of the infection chain: 1. 2. 3. 4. 5. 6. A causative agent Its reservoir Its portal of exit A method of transmission A portal of entry A susceptible host The Chain of Infection (cont’d) The causative agent is the microorganism present in the environment The reservoir is the source of infection ◦ Human individuals or groups ◦ Environmental fomites or contaminants (i.e. food, water, soil, air) ◦ Animals (i.e. ticks, fleas, mosquitos, bats) The portal of exit is the site where a pathogen leaves the reservoir ◦ ◦ ◦ ◦ Gastrointestinal Respiratory Blood Urinary The Chain of Infection (cont’d) The mode of transmission is the mechanism of transfer for the agent ◦ Contact transmission (direct, indirect contact) ◦ Airborne or droplet ◦ Vector (flies, mosquitos) The portal of entry is the location by which the agent enters; the agent gains entry by permeating the first level of defense (i.e. skin, mucus membranes) The susceptible host has little resistance to the invader and is capable of supporting growth Normal Flora Normal flora is the mixture of organisms found at any anatomical site at any given time Complex mixture (>200 species of bacteria) The make-up of normal flora depends on genetics, age, sex, stress, nutrition, diet, etc The nature of associations between humans and their normal flora is thought to be mutualistic (beneficial to each other) ◦ Humans benefit normal flora by supplying nutrients, a stable environment, constant temperature, protection, and transport ◦ Normal flora benefits humans by stimulating the immune system and keeping potential pathogens away through colonization, competing for nutrients, and contributing to a low (acidic) pH Normal Flora (cont’d) Normal flora has tissue tropism, or tissue preference ◦ Certain bacteria may be found at one location on/in the body, but not another ◦ This may be due to the presence of an essential growth factor needed by the bacteria Density and composition of normal flora depend on location ◦ High moisture content of the axilla, groin, and areas between the toes have higher counts of normal flora than other skin sites; bacteria on the skin surface near any body orifice may be similar to the bacterial count within that orifice Normal Flora (cont’d) The majority of skin organisms are found in the superficial layer of epidermis and upper parts of hair follicles ◦ Staphylococcus epidermidis Remains benign until conditions arise that allow it to cause disease Especially life-threatening in hospital patients with any type of catheter This bacteria can form antibiotic-resistant biofilms along the catheter and enter the bloodstream causing systemic infection Can be fatal Catheters that prevent biofilm are in production ◦ Corynebacteria Normal Flora (cont’d) Throat organisms ◦ Corynebacterium diphtheriae Urogenital epithelium ◦ Neisseria gonorrhoeae Surfaces of the tongue and teeth ◦ Streptococcus mutans ◦ Streptococcus salivarius Epithelium of the small intestine ◦ Vibrio cholerae ◦ Escherichia coli (E. coli) Nasal membranes ◦ Staphylococcus aureus Normal Flora (cont’d) Respiratory tract ◦ ◦ ◦ ◦ Nares are always heavily colonized Staphylococcus epidermidis Corynebacteria Staphylococcus aureus The nares are the main carrier site for this pathogen Can be found on the face and hands of individuals that are nasal carriers Pathogenic A major cause of surgical wound and systemic infection Often resistant to antibiotics; this type of S. aureus can be fatal for the aged individual, burn and trauma patients, and the immunocompromised Normal Flora (cont’d) Methicillin-resistant staphylococcus aureus ◦ Has become resistant to most antibiotics, including methicillin and vancomycin ◦ Often carried in the nares of health care workers, and transmitted from patient to patient ◦ Has been found to survive on nurses’ hands for up to 3 hours ◦ Can result in skin and wound infection, septicemia, endocarditis, and pneumonia ◦ Why some people are carriers while others are not remains unknown ◦ Prevent spread through effective handwashing Nosocomial Infections Develop in individuals during hospitalization Preventable Three main influences include: ◦ Overuse of antibiotics ◦ Failure to follow basic infection control practices ◦ Increase in immunocompromised patients 200,000 nosocomial infections occur each year Most are related to the use of IV therapy Rates are highest in the ICU Hand hygiene is most important in preventing the spread of dangerous microbes; gloves do not replace adequate hand hygiene; long natural and artificial nails harbor significant bacteria Factors that could weaken the host and allow the infection process: Age Integrity of the mucus membrane Body weight Body system function State of nutrition and hydration Mental outlook Coexisting disease process Social and psychological health Ability to adapt to the external environment Stress Immune incompetence Length and amount of exposure to microbes Medications (antibiotics, chemotherapy) Skin integrity Equipment (indwelling catheter, IV line) Who is at risk for infection? Diabetes ◦ Foot and lower leg ulcers ◦ Candida infections (vulvovaginal or thrush) ◦ UTI (more common and more severe) Alcoholism ◦ Decreased effectiveness of neutrophils, impaired neuro function, and organ damage ◦ Pneumonia more likely than in general population ◦ Bacterial peritonitis (co-occurs with ascites) Injected drug use ◦ ◦ ◦ ◦ ◦ Unsterile techniques Bacterial endocarditis on tricuspid valve Superficial skin infections Tetanus Transmission via needle-sharing (hepatitis, HIV) Infection risk (cont’d) Internal prosthesis ◦ Potential for infection at site of insertion ◦ Immune response to foreign material ◦ Inoculation at time of insertion (sepsis may occur years after insertion) Indwelling catheter ◦ Provides communication between external environment and sterile internal environment ◦ The two major factors that determine the likelihood of catheter-related infections are duration of catheterization and degree of cleanliness maintained during catheterization Neurologic deficits ◦ Predisposes individual to infection ◦ Loss of gag reflex can lead to aspiration of gastric or oral secretion (pneumonia) ◦ Diabetic neuropathy ◦ Long-term catheterization with neurogenic bladder Infection risk (cont’d) Granulocytopenia ◦ Absence of adequate number of circulating neutrophils ◦ Hematologic malignancy ◦ One becomes infected with one’s own normal flora ◦ Causes fever Immunosuppressive agents ◦ Used to prevent rejection of transplanted organ or tissue ◦ Used to control autoimmune disorders ◦ Steroids ◦ Injectable tumor necrosis factor (TNF) ◦ Inhibiting drugs (rheumatoid arthritis, inflammatory bowel disease) Occupational exposure ◦ Legionnaire’s Disease (form of pneumonia from the spread of water droplets through an air-conditioning system) Infection risk (cont’d) Age ◦ Diminished immune response in the elderly ◦ Nosocomial infection from residence in hospital/nursing home ◦ Various tube insertions ◦ Failure to follow infection control procedures ◦ Environmental factors IV therapy ◦ Most common invasive procedure ◦ At least 90% of hospitalized patients require IV ◦ CDC reports lower infection rate in peripheral than central venous lines ◦ Tunneled central catheters have lower infection rate than non-tunneled catheters Lines of defense for the prevention of infection: First line of defense – Skin and mucus membranes ◦ Act as protective coating ◦ Secrete substances to inhibit the growth of microbes ◦ Sweat glands secrete lysozyme, which is an antimicrobial enzyme ◦ Sebaceous glands secrete sebum, which has antimicrobial and antifungal properties ◦ Acidic secretions of the skin inhibit the growth of microbes Lines of defense (cont’d) Skin and mucus membranes ◦ Colonized with normal flora, which prevents the entrance of pathogens Second line of defense – Phagocytosis ◦ Leukocytes have the ability to ingest bacteria; measurement indicates severity of infection ◦ Neutrophils fight bacteria; first responders; release lysozyme that destroys bacteria; phagocytosis Complement system ◦ 17 different proteins that attach to the infectious agent and promote ingestion by the phagocyte Stages of the Infection Process Incubation Stage ◦ Presence and reproduction of pathogen ◦ Host remains asymptomatic ◦ This stage could last hours to years Prodromal Stage ◦ Initial symptoms appear, which are usually mild ◦ Symptoms may be nonspecific Acute Stage ◦ Presence of pronounced symptoms ◦ Results from toxic by-products of the metabolic processes of microbes and from tissue damage caused by the inflammatory process Stages of Infection (cont’d) Convalescent Stage ◦ Diminished symptoms ◦ Infection is contained Resolution Stage ◦ Elimination of the pathogen Classification of Infection Local infection ◦ Microbes penetrate tissues at a specific area of the body ◦ Microbes grow, multiply, exert effects within that specific area ◦ Microbes do not migrate to other areas of the body ◦ A localized infection can become systemic if conditions are right in the host Classification of Infection (cont’d) Systemic infection ◦ Microbes travel freely and exert effects on several, or all, body systems Sepsis ◦ Describes a pathologic condition that results from the spread of microbes or their toxins through the circulatory and/or lymphatic system ◦ This is the leading cause of death in the ICU ◦ 65 – 70% of sepsis is caused by gram negative E. Coli (diarrhea, UTI, pneumonia), pseudomonas (pneumonia, bacteremia), klebsiella (pneumonia, UTI, bronchitis) ◦ Sepsis is on the rise since more pathogens are becoming antibiotic resistant Updated CDC Guidelines for Preventing Infusion Device-Related Infections -- Major Recommendations - Prepping the skin ◦ Use 2% chlorhexidine, which is more effective in lowering catheter-related bloodstream infection rates than 10% povidone-iodine and 70% isopropyl alcohol ◦ Chlorhexidine persists on the skin longer, which is important because it kills organisms that could repopulate the insertion site from deeper skin layers Major Recommendations (cont’d) Prepping the skin ◦ The CDC recommends “back and forth” scrub rather than outwardly radiating concentric circles ◦ Allow solution to dry ◦ It has not been determined if chlorhexidine should be used on infants less than 2 months of age Routine central venous catheter replacement has now been changed to dwell time as long as needed, (remove immediately when no longer needed) Major Recommendations (cont’d) Peripheral IV site recommended for only 72 to 96 hours to prevent phlebitis Maintain peripheral IV in place in pediatric patients as long as needed ◦ Ensure site is free from complications ◦ If catheter was placed in an emergency situation, replace within 48 hours Follow hand antisepsis protocols (i.e. handwashing and alcohol-based hand rubs) Use aseptic technique Wear clean gloves Major Recommendations (cont’d) For central line insertions, use maximum sterile barrier technique (i.e. cap, mask, sterile gown, sterile gloves, large sterile drapes) ◦ This also applies to peripherally inserted central lines ◦ Facilities must comply with these recommendations by having the necessary equipment available Change short-term central catheter dressings every 48 hours or every 7 days depending on the dressing Major Recommendations (cont’d) The CDC does not recommend transparent dressing over tape-and-gauze dressing, but gauze does not allow access to viewing insertion site ◦ Gauze is adequate for a site that is bleeding (i.e. the first day or so after insertion) ◦ If using a transparent dressing, visually inspect IV site ◦ If using a gauze dressing, palpate to assess for pain or tenderness to site ◦ Remove dressing if any symptoms of infection occur in order to inspect directly ◦ Educate patient to inform the nurse of any discomfort or changes at the IV site Major Recommendations (cont’d) Replace a gauze dressing every 48 hours and a transparent dressing every 7 days (except in pediatric patients in which the risk of dislodging the catheter outweighs the benefits of changing the dressing) Change either dressing if it becomes contaminated, damp, or nonadherent It is not recommended to routinely use antimicrobial ointment to the insertion site, as this promotes fungal infections and antimicrobial resistance Major Recommendations (cont’d) The Infusion Nurses Society recommends use of sterile wound closure strips under a dressing if needed to secure the catheter; the sterile strips are to be changed along with dressing changes The IV tubing is to be routinely changed no more than every 72 hours, including the piggyback, or secondary, tubing that remains attached to the primary tubing continuously ◦ Exceptions include 24-hour use of tubing for blood, blood products, lipids, and TPN Major Recommendations (cont’d) Add-on adaptors used with needleless systems should be changed as frequently the tubing Stopcocks have a high contamination rate (50%), so closed, modified stopcocks and piggyback connections should be used instead Use of central catheters coated or impregnated with antimicrobial/aseptic agents is not recommended due to increased cost and risk for antimicrobial resistance Major Recommendations (cont’d) Coated central catheters can be used if chlorhexidine site preparation results in infection and catheter will remain in place longer than 5 days Only remove central catheters when they are no longer needed; don’t replace them for the sole purpose of reducing the incidence of infection Intravascular catheter infections may be localized or systemic Major Recommendations (cont’d) The CDC defines localized infection as the significant growth of a microorganism from the catheter tip, subcutaneous segment of the catheter or catheter hub The CDC defines systemic infection as per the above definition, in addition to growth from a peripheral blood culture (in other words, a mild local infection to the IV site could progress to full-blown systemic bacteremia) The CDC does not recommend taking routine cultures of catheter tips Major Recommendations (cont’d) Watch for localized and systemic signs and symptoms associated with catheter-related infection ◦ ◦ ◦ ◦ Redness, swelling, and tenderness at insert site Cellulitis and purulent drainage Altered mental status Diaphoresis, fatigue, muscle aches, weakness, fever, and chills ◦ Glucose intolerance ◦ Abdominal pain, nausea and vomiting, and diarrhea ◦ Hypotension, tachycardia, and hyperventilation Major Recommendations (cont’d) Resistant pathogens that can cause catheter-related bloodstream infections include ◦ Coagulase-negative staphylococcus ◦ Enterococcus ◦ Staphylococcus aureau These are commonly resistant to multiple antibiotics, which makes treatment difficult Catheter-related infections occur by contamination of device by skin flora on insertion (i.e. migration down the cannula tract from the skin) or contamination of the hub during manipulation Major Recommendations (cont’d) Use clean gloves to insert a peripheral catheter; do not touch access site after skin prep has been applied Wash hands with antiseptic soap and water, or an alcohol-based gel or foam Observe hand hygiene before and after palpating catheter insertion sites; before and after inserting an IV; and before and after replacing, accessing, repairing, or dressing an IV site When inserting a peripheral catheter, use a “no touch” procedure, wear gloves that fit, do not repalpate after prepping, and do not touch the prepped area with nonsterile gloves to stabilize the vein Occupational HIV Exposure Preventing exposures to blood and body fluids is the primary means of preventing occupationally acquired human immunodeficiency virus (HIV) infection ◦ Universal precautions ◦ Handwashing ◦ Proper use of safety equipment Follow institutional policy/procedures Recommendations for post-exposure prophylaxis (PEP) include urgent medical treatment to ensure timely initiation ◦ Prompt reporting of exposure ◦ 4-week regimen of two antiretroviral medications to prevent seroconversion of HIV infection in health care workers ◦ Counseling IV Calculation Introduction to IV Calculation IV’s are fluids, sometimes infused with medications, blood, nutrients, electrolytes, etc. The fluids are generally normal saline (NS), or salt water, and dextrose water (DW), or sugar water The IV flow rate is the speed at which the IV fluid infuses into the body ◦ Often measured in drops per minute (abbreviated “gtt/min”) Factors affecting the flow rate include: ◦ The amount of fluid to be infused ◦ The time over which it is to be infused ◦ The size of the tubing IV Calculation (cont’d) The number of drops required to deliver 1 ml of fluid varies with the type of IV administration set (tubing) used; the size of the tubing is called the drop factor There are 2 types of IV administration sets: ◦ Macrodrip = 10, 15, or 20 gtt/ml ◦ Microdrip = 60 gtt/ml In calculating the flow rate, ratio/proportion cannot be used because there are more than two components to calculate The dosage calculation formula cannot be used because a dosage is not being calculated When calculating the flow rate, all rates should be rounded to the nearest whole number IV Flow Rate Formula volume of infusion (in mL) x drop factor time of infusion (in minutes) = Flow rate (in gtt/min) • Note that time must be converted to minutes, and that the drop factor is in gtt/mL IV Calculation Examples Administer D5 ½ NS at 30 mL/h. The drop factor is a microdrip. 30mL x 60gtt/mL = 30gtt/min 60min An IV medication in 60 mL of 0.9% NS is to be administered in 45 minutes. The drop factor is a microdrip. 60mL x 60gtt/mL = 80gtt/min 45min Examples (cont’d) Administer 3,000 mL D5 ½ NS in 24 hours. The drop factor is 10 gtt/mL. 3000mL x 10gtt/mL = 21gtt/min 1440min Administer Lactated Ringer’s at 125 ml/h. The drop factor is 15 gtt/mL. 125mL x 15gtt/mL = 31gtt/min 60min Examples (cont’d) 1,000 mL of Lactated Ringer’s solution is to infuse in 16 hours. The drop factor is 15 gtt/mL. 1000mL x 15gtt/mL = 16gtt/min 960min Infuse 2,000 mL D5W in 12 hours. The drop factor is 15 gtt/mL. 2000mL x 15gtt/mL = 42gtt/min 720min Electronic Flow Rate When using an electronic infusion device (IV pump), the flow rate is calculated in milliliters per hour (mL/h) To find mL/h, you must divide the total milliliters by the total hours You would then round your final answer to the nearest whole Examples - ◦ 1000 mL in 8 hours = 1000/8 = 125mL/h ◦ 500 mL in 24 hours = 500/24 = 21mL/h If an order is given without total milliliters, this becomes a dose calculation; you would use ratio-proportion, dimensional analysis, or the Formula Recalculating the Flow Rate Sometimes the IV infusion rate changes due to a change in the patient’s position If you notice that the flow rate needs to be adjusted, assess the client and determine the percentage of change needed to correct the infusion Please note that you can adjust the infusion flow rate by no more than 25% without consulting the physician or practitioner In order to determine the percentage of increase or decrease of the flow rate: ◦ Determine the actual change in the flow rate ◦ Divide by the original flow rate ◦ Multiply by 100 Examples of IV Recalculation Original infusion order : 1000mL D5W IV to infuse over the next 10 hours. Infusion start time: 1300 hours. Drop factor = 10. Hourly rate = 100mL/h. Flow rate = 17gtt/min. At 1430 hours, the infusate level is at 900mL. 150mL should have already infused, leaving 850mL remaining to infuse over the next 8 ½ hours. The IV would be recalculated as follows: 900mL = 106mL/h – 100mL/h = 6mL/h 8.5h 6mL/h = 0.06 x 100 = 6% increase 100mL/h Recalculation Examples (cont’d) Original infusion order : 1000mL D5W IV to infuse over the next 8 hours. Infusion start time: 0900 hours. Drop factor = 15. Hourly rate = 125mL/h. Flow rate = 31gtt/min. At 1200 hours, the infusate level is at 850mL. 375mL should have already infused, leaving 625mL remaining to infuse over the next 5 hours. The IV would be recalculated as follows: 850mL = 170mL/h – 125mL/h = 45mL/h 5h 45mL/h = 0.36 x 100 = 36% increase 125mL/h Titrating Medications Titrating means to adjust the medication until it brings about the desired effect Always start with the low end of “safe” and increase dosage from there Follow institutional protocol for titrating medications Titrated medications are calculated in the same way as non-titrated drugs An example of a titration order would be: ◦ A client weighing 50 kg is to receive a Dobutrex solution of 250 mg in 500 mL D5W ordered to titrate between 2.5–5 mcg/kg/min Titration Calculation Examples In the previous order, the initial dose would be set at the low end of safe. Therefore, the client will receive 2.5mcg/kg/min of the ordered medication, and will receive no more than 5mcg/kg/min. The client’s weight is 50kg. 50 x 2.5 = 125mcg/min safe range of drug 50 x 5 = 250mcg/min Per IV pump, the client would receive the minimum dosage of 7500mcg/h, or 7.5mg/h: 250mg = 500mL = 250 X mg/mL = 7.5mg(500mL) 7.5mg X mL X = 3750mg/mL = 15mL (initial dose is 15mL/h) 250mg Heparin Heparin is an anticoagulant for the prevention of clot formation; ensure correct calculation to avoid complications Heparin is measured in USP units IV Heparin is often ordered in units per hour (units/h), and should be administered per IV infusion device Heparin infusions would be calculated like other medications via IV pump, in milliliters per hour (mL/h) The normal adult dosage of Heparin is 20,000 – 40,000 U every 24 hours