S. Thomas
advertisement

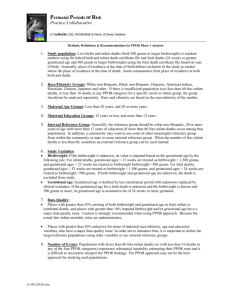
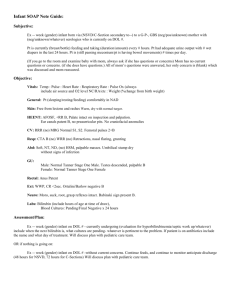
The Perinatal Periods of Risk Approach Sanil Thomas MS Biostatistics candidate April 27, 2010 Introduction • Infant mortality rate (IMR) is a critical indicator of nation’s health • IMR remains higher in United States than in other industrialized countries • But IMR does not provide sufficient information to understand the factors that contribute to infant mortality Introduction • Traditional methods don’t include the fetal death counts for the analysis of mortality rates • Fetal-infant mortality is a multi dimensional issue and a detailed analytical approach to fetal- infant mortality is needed to focus community initiatives for improving maternal and infant health. Objectives • To look at Feto-Infant mortality in a new way • Apply PPOR framework for New York State • To see the distribution of common risk factors by county level Perinatal Periods of Risk (PPOR) Approach • The Perinatal Periods of Risk Approach was developed by Dr. Brian McCarthy from the W.H.O. Perinatal Collaborative Center at CDC and other W.H.O. colleagues. • Simple method that is based on a strong conceptual prevention • The PPOR Data allow you to look at feto-infant mortality in new ways PPOR : 6 Basic Steps Step 1: Assure Analytic and Community Readiness Step 2: Conduct Analytic Phases of PPOR Step 3: Develop Strategic Actions for Targeted Prevention Step 4: Strengthen Existing and/or Launch New Prevention Initiatives Step 5: Monitor and Evaluate Approach Step 6: Sustain Stakeholder Investment and Political Will Analytic Phases of PPOR Phase 1: Identifies populations and periods of risk with the largest excess mortality. Phase 2: Explains why the excess deaths occurred. PPOR Examines Deaths in TWO dimensions simultaneously: • Age at death • Weight at birth The First Dimension Of PPOR Analysis: Age at Death Fetal 4 wks Infancy 20 wks 28 wks Spontaneous Abortion Early Late Fetal Fetal Postneonatal Infant Feto-Infant Second Dimension: Birthweight Birthweight • Very Low Birthweight (PPOR limit) = less than 1500 grams (3.3 pounds) • Low Birthweight = less than 2500 grams (5.5 pounds) • Normal Birthweight e.g., a 7.5-pound baby weighs 3,400 grams PPOR “Map” fetal & infant deaths Age at Death Birthweight 500-1499 g 1 2 3 4 5 6 1500+ g PPOR “Map” fetal & infant deaths Age at Death Birthweight Fetal Death 500-1499 g 1500+ g Neonatal Postneonatal Maternal Health/ Prematurity Maternal Newborn Care Care Infant Health PPOR is about ACTION (each period of risk is associated with a set of possible areas for action) Maternal Health/ Prematurity Preconception Health Health Behaviors Perinatal Care Maternal Care Prenatal Care High Risk Referral Obstetric Care Newborn Care Perinatal Management Neonatal Care Pediatric Surgery Infant Health Sleep Position Breast Feeding Injury Prevention PPOR: Phase 2 • Poisson log linear modeling • Covariates/Fixed effects a. Mother’s race b. Mother’s education c. Mother’s age d. Payor • Random effect - County PPOR: Phase 2 • Fetal death was not used • 2004-2007 • Predicted death counts were used to obtain smoothed death rates • Modeling done for each county Relative risk calculated from the beta estimates Data • New York State Dept. of Health. a. Electronic records of births b. Linked birth-death cohort c. selected fetal deaths Phase 1 : 2003-2007 Phase 2 : 2004-2007 Software used • SAS • Excel • ArcGIS Results Phase 1 Results Death rates per 1000 live births and Fetal deaths Obs County Total number of deaths Sum of Live births and Fetal deaths (PPOR categories) Total Death Maternal health/prematuri ty Maternal care Newborn care Infant health 1 ST LAWRENCE 61 6215 9.81 2.74 2.25 2.74 2.09 2 BROOME 101 10438 9.68 3.35 2.59 1.92 1.82 3 OSWEGO 62 6884 9.01 2.91 3.63 1.45 1.02 4 BRONX 1015 112785 9.00 4.34 2.66 0.79 1.21 5 JEFFERSON 76 8523 8.92 3.40 3.17 1.29 1.06 6 SCHENECTADY 76 9142 8.31 3.17 2.30 1.31 1.53 7 KINGS 1607 201738 7.97 3.66 2.35 0.86 1.10 8 ONEIDA 101 12905 7.83 2.40 1.55 1.63 2.25 9 ULSTER 72 9212 7.82 2.93 1.85 1.41 1.63 10 ALBANY 120 15904 7.55 3.58 1.76 0.75 1.45 11 RENSSELAER 66 8822 7.48 2.83 1.70 1.13 1.81 12 ERIE 373 50694 7.36 2.88 2.05 1.12 1.30 13 ONONDAGA 197 27648 7.13 2.89 1.77 1.23 1.23 14 QUEENS 990 153600 6.45 2.85 1.93 0.69 0.97 15 MONROE 273 43613 6.26 2.64 1.44 0.87 1.31 16 NEW YORK 629 102684 6.13 2.69 2.01 0.56 0.87 17 NIAGARA 70 11444 6.12 2.97 0.96 0.87 1.31 18 ORANGE 159 26316 6.04 2.24 1.25 1.18 1.37 19 RICHMOND 171 29176 5.86 3.29 1.34 0.55 0.69 20 ROCKLAND 134 23110 5.80 2.08 1.51 1.51 0.69 21 WESTCHESTER 342 61189 5.59 2.27 1.31 1.14 0.87 22 SUFFOLK 531 96216 5.52 2.53 1.29 0.91 0.79 23 NASSAU 411 77325 5.32 2.16 1.33 0.69 1.14 24 SARATOGA 60 11946 5.02 2.18 1.26 0.75 0.84 25 DUTCHESS 71 15763 4.50 2.03 0.38 1.33 0.76 Phase 1 Results New York State Death Rates per 1000 live births and fetal deaths 2.58 Maternal Health/ Prematurity 1.63 Maternal Care 1.12 Newborn Care 1.21 Infant Health Phase 2 Results Poisson Log Linear model estimates Solutions for Fixed Effects mom_educn mom_age payor Estimate Standard Error DF t Value Pr > |t| -5.7132 0.06320 56 -90.40 <.0001 -0.1806 0.1431 2730 -1.26 0.2071 Effect Intercept mom_race mom_race asian mom_race black_alone 0.9248 0.05255 2730 17.60 <.0001 mom_race other_races 0.1056 0.07598 2730 1.39 0.1646 mom_race z_white_alone 0 . . . . mom_educn HighSchoolorAssoc 0.4346 0.05602 2730 7.76 <.0001 mom_educn lessthan_HighSchool 0.6420 0.07174 2730 8.95 <.0001 mom_educn z_Bachelors&above 0 . . . . mom_age 35&above 0.1367 0.05468 2730 2.50 0.0125 mom_age lessthan20 0.2512 0.06412 2730 3.92 <.0001 mom_age z_20to34 0 . . . . 0.03220 0.04705 2730 0.68 0.4937 0 . . . . payor medicaid payor other Conclusions • Infant mortality Higher risk ratio for black mothers relative to white mothers Higher risk ratio for mothers having education less than high school when compared to mothers having education more than bachelors Higher risk ratio for mothers of age less than 20 when compared to mothers of age between 20 and 34 • Smoothed rates are higher in St.Lawrence, Erie, Schenectady, Oneida, Broome, Cortland etc • Risk ratio for black mothers relative to white mothers are higher in the counties Orleans, Oswego, Chenango and Cortland Limitation • Missing data 12428 records out of 497787 records 246 deaths • Inconsistent fetal data Future study • Detailed Phase 2 analysis including fetal deaths • MHP and IH categories – Protocol for Phase 2 studies • Cluster Analysis • Spatial smoothing analysis Reference • http://www.citymatch.org/ppor_index.php • Cai, J, Hoff GL, Dew PC et al. Perinatal periods of risk: analysis of fetalinfant mortality rates in Kansas City, Missouri. Matern Child Health J.2005;9:199-205 • Cai J, Hoff GL, Archer R et al. Perinatal periods of risk analysis of infant mortality in Jackson County, Missouri. J Public Health Manage Pract. 2007;13:270-277. Acknowledgments • Dr. Glen D. Johnson, PhD, MS, MA • Dr. Marilyn A. Kacica, M.D.,M.P.H Questions???