File
advertisement

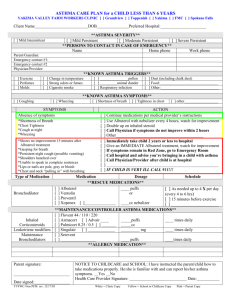
Heather Carballo, Dana Horton, Claudette Johnson, Kimberly Kusch Goals Quick relief of symptoms Controlling inflammation Types Controller (LABA) • Corticosteroids • Long Acting Beta Agonists (LABA’s) • Leukotriene modifiers (LTRA) • Cromolyn & Nedocromil • Methylxanthines: (Sustainedrelease theophylline Relievers (SABA) Easing flare-ups • Short acting bronchodilators • Corticosteroids • Anticholinergics (Lehne, 2013) Short Acting Bronchodilators Long Acting Bronchodilators (LABA) Keeps swelling and mucus from developing in the airways Must be taken EVERY day even when not having symptoms Inhaled corticosteroids (ICS’s) are the most common and effective way to control asthma Help prevent asthma exacerbations from developing! (Lehne, 2013) SABA Mild Intermittent • Reliever only prn Both control and rescue medications come in MDI (metered dose inhalers) and nebulized forms Mild Persistent • Controller/Reliever Moderate Persistent • Controller plus long-acting bronchodilator and reliever Control medications are also available in dry powder discs, breath actuated inhalers and pill form Severe Persistent • Controller plus long-acting bronchodilator and reliever (Asthma Organization, 2012) (Lehne, 2013; Schiffman & Szeftel, 2012) Short-acting Inhaled Bronchodilators Proventil, Ventolin (Albuterol) Xopenex (Levalbuterol) Maxair Autohaler (Pirbuterol) Alupent (Metaproterenol) For relief of acute symptoms or as preventive treatment prior to exercise Potential adverse effects Tremors, tachycardia, headache Therapeutic issues Drugs of choice for acute bronchospasm Systemic Corticosteroids Pediapred Prelone Prednisone Orapred Prevents progression of moderate to severe exacerbations, reduces inflammation Potential adverse effects Short-term- increased appetite, fluid retention, mood changes, facial flushing, stomachache Long term- growth suppression, hypertension, glucose intolerance, muscle weakness, cataracts (Lehne, 2013; Mayo Clinic, 2012; McCance & Huether, 2010) Herbal Therapy Ephedra (Ma Huang) Dangerous and should be avoided Potent CNS and CV stimulant Can be a precursor for methamphetamine FDA recently banned its use Many other herbal folk remedies used by different cultures (Lehne, 2013; McCance & Huether, 2010) (Schiffman & Szeftel, 2012) Corticosteroids: Pulmicort, QVAR, Alvesco, AeroSpan, Flovent Pharmacokinetics: Peak concentration in thirty minutes for inhaled therapy, 34% distributed in the lungs and systemic availability is 39%. Rapidly metabolized and excreted in urine and feces (Pulmicort Pharmacology, 2006). Pharmacodynamics: Rapid onset of action, asthma improvement demonstrated within 24 hours after starting treatment although full benefits may take one to two weeks to be seen. When orally inhaled there is a direct effect on the respiratory system(Pulmicort Pharmacology, 2006). Drug Interactions: certain antibiotics, antidepressants, and ketoconazole (Pulmicort Pharmacology, 2006). Side effects: Runny nose, sore throat, white patches in mouth, nose bleed, headache(Pulmicort Pharmacology, 2006). Adverse effects: Worsening respiratory symptoms, wheezing, vision changes and weakness(Pulmicort Pharmacology, 2006). Long Acting Beta Agonist: Brovana, Perforomist, Arcapta, Serevent Diskus Pharmacokinetics: These medications typically work locally within the lungs. Taking plasma levels will not indicate therapeutic effects. These medications are 96% protein binding and are excreted in the feces and urine. The usual half life of these medications are usually fairly long, on average about 5-7 days (Kim, 2009). Pharmacodynamics: Effects of these medications usually last about 12 hours. Causes bronchodilation by relaxing smooth muscles in the airway (Kim, 2009) Drug Interactions: Erithromycin, beta blockers, MAOI’s, antidepressants, non-potassium sparing diuretics (Kim, 2009.) Side effects: Headache, nasal congestion, nausea/vomiting, skeletal muscle pain. Adverse effects: Bronchospasms which could cause worsening respiratory effects, irritation or swelling of the airway, hypertension, increased heart rate, hypokalemia (Kim, 2009). Assess respiratory status. Overall physical exam with vital signs should be conducted. Assess patient’s knowledge of medication administration and lab values as needed. Assess for side effects and knowledge of side effects as well as compliance with medication regimen. (Stanley et al., 2008) Risk for ineffective breathing pattern related to noncompliance with medication regimen Risk of ineffective airway clearance related to improper use of asthma medications Anxiety related to inability to manage disease process as evidenced by patient stating they are overwhelmed Deficient knowledge related to medication administration as evidenced by improper use of metered dose inhaler. (Stanley et al., 2008) Patient will identify 5 signs of worsening respiratory status. Patient will identify 5 potential side effects of each medication they are taking. Patient will verbalize their asthma treatment plan and discuss why it is important along with any concerns. Patient will demonstrate proper administration of a metered dose inhaler. (Stanley et al., 2008) Nurse will provide written and verbal education on respiratory status. Nurse will provide written and verbal education on the patient’s medications and side effects. Nurse will discuss treatment plan with patient and discussion of any anxiety as well as provide written information. Nurse will provide videos to patient on use of meter dose inhaler and will assist with return demonstration by patient. (Stanley et al., 2008) Patient’s condition improved. Patient’s condition stabilized. Patient’s condition deteriorated. (Stanley et al., 2008) Health Care Provider Community Resources Public Health Department Patient Education Tools* Your Voice-Advocacy School Nurse Take Control of your Asthma American Lung Association. (2012). Learning more about Asthma. Retrieved from http://www.lung.org/lung-disease/asthma/ Gulanick, M., & Myers, J. (2011). Nursing Care Plans (7th ed.). St. Louis: Mosby Elsevier. Kaufman, G. (2012). Asthma: assessment, diagnosis, and treatment adherence. Nurse Prescribing, 10(7), 331-338. Kim, D. (2009). Evaluation of Long Acting Beta Agonists. Allergy and Immunology , 8, 933-940. Lehne, R.A. (2013). Pharmacology for nursing care. (8th ed.) St. Louis: Saunders Elsevier. 967-981. Mayo Clinic. (2011). Asthma inhalers: Which one's right for you? Retriever from http://www.mayoclinic.com/health/asthma-inhalers/HQ01081 McCance, K.L. & Huether, S.E.(2010). Pathophysiology: The biologic basis for disease in adults and children. (6th ed.). St. Louis: Mosby Elsevier.1285-1286. Pulmicort Pharmacology. (2006). Retrieved November 9, 2012, from Drug List 1: www.1stdruglist.com/pumicort.html Schiffman, G. & Szeftel, A. (2012). What asthma medications to use. MedicineNet. Retrieved from http://www.medicinenet.com/asthma/page9.htm#what_medications_are_used_in_the_treatment_of_asthma