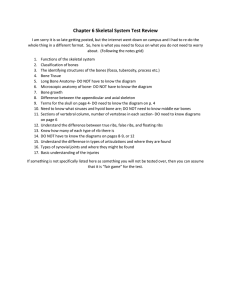
Chapter 5 Study Guide Bones I. Functions 1) Supports body 2
advertisement

Chapter 5 Study Guide Bones I. Functions 1) Supports body 2) Protects soft body parts Rib cage, skull 3) Produces blood cells- Certain bones 4) Stores calcium and phosphate ions in calcium phosphate Ca3(PO4)2. 98% body’s Ca+2 in bone 5) Permits flexible body movement- Provides leverage for muscles. 6) Energy metabolism * new! - osteoblasts produce osteocalcin (hormone) which regulates insulin secretion. Also, stimulates adipocytes to store less fat! II. Characteristics & classification of Bone A. Axial Skeleton: skull ,vertebral column, sternum, ribs Appendicular skeleton: all other bones B. Blood supply: well vascularized. Nutrient arteries hole in the diaphysis (nutrient foramen) to marrow, spongy & compact bone. C. Composition/Structure 1. 65% inorganic a) Calcium phosphate interacts with calcium hydroxide to form crystals of hydroxyapatite. b) also contains sodium, magnesium, fluoride c) Very strong but crystals shatter when exposed to bending or twisting motion. 2. 35% organic a) collagen fibers b) tough and flexible. Gives bones flexibility to stretch & bend. D. Microscopic anatomy/Histology 1. bone organization (review osteon) a) bone composition: collagen & hypoxyapatites (calcium & phosphate) b) concentric lamellae interstitial lamellae circumferential lamellae c) blood supply: central canals, Volkman’s (perforating) canals, canaliculi d) trabeculae: (spicules) if thick, osteons will be present E. Cells 1. osteoprogenitor cells: unspecialized stem cells osteoblasts. Found in inner perositeum & endosteum. Important in repair & growth. 2. osteocytes: star shaped, from osteoblasts, maintain bone matrix. Occupy lacunae. 3. osteoblasts “bud/sprout”: a) lay down osteoid: unmineralized, organic portion of the bone matrix b) Respond to stress on bones & hormones. c) Osteoblast is surrounded by matrix osteocyte 4. osteoclasts: a) giant, multinucleated, mobile. Derived from immune cells b) secretes HCl: breaks down Ca+2 and PO4 -3 lysosomal enzymes breaks down collagen, a process called osteolysis c) furrowed edge to increase surface area for osteolysis F. Membranes: 1. Periosteum: covers entire outer surface of bone except at ends where articular cartilage is. a) Held to bone by Sharpey’s fibers (collagen fibers) b) Double membrane: rich in blood & nerve! - inner layer osteoprogenitor cells, osteoblasts & osteoclasts- remodeling - outer layer : fibrous, tough. Attach bone to CT network 2. Endosteum: internal membrane, incomplete layer, only 1 cell layer thick. Contains osteoprogenitor cells Covers: 1. trabeculae 2. lines central canals 3. medullary cavity G. Shapes/types 1. Sutural bones 2. Pneumatized bones 3. Short bones are cube shaped In wrist & ankle. 4. Flat bones are plate-like &broad surface. 5. Irregular bones have varied shape 6. Sesamoid bone: imbedded in tendon 7. Long bones longer than they are wide. 2 distinct ends. a) Epiphysis b) diaphysis c) metaphysis d) medullary cavity with yellow marrow e) articular cartilage f) epiphyseal plates (or epiphyseal lines) g) periosteum & Sharpey’s fibers h) compact bone & spongy bone (with red marrow, site of hematopoiesis) III. Growth/remodeling: A. Bone remodeling: bone is deposited & removed continuously. Spongy bone is replaced every 3-4 years! Compact bone every 10 yrs! B. Ossification & Osteogenesis: formation of bone 1. Intramembranous ossification: bone forms from mesenchyme (embryonic tissue type). Skull bones (except a few at the base) & clavicle are formed this way 2. Endochondral ossification (endochondral bones) Begins at 2nd month of development & doesn’t stop until early adulthood. This type of growth helps a bone grow both in length & width. a) Primary ossification center: medullary cavity b) Secondary ossification center: epiphyses. c) Epiphyseal plate i) Band of hyaline cartilage within the epiphyses of bone. Bone can still grow in length as long as there is a plate. Cartilage is organized for quick, efficient growth- chondroblasts are at the top of stacks & divide quickly. Pushes the epiphysis away from the diaphysis. Older chondrocytes signal surrounding matrix to calcify & then die. Leaves trabeculae of calcified cartilage- eventually forming spongy bone. ii) Bones lengthen entirely by growth of epiphyseal plates & the plate maintains a constant thickness. iii) End of adolescence: -chondroblasts divide less, ephiphyseal plates thin. - cartilage stops growing, replaced by bone. - Epipyseal plate become an epiphyseal line. 3. Appositional Growth: 1. Growth in diameter is through appositional growth : adding layers, become thicker & stronger. 2. Layers laid down around the diaphysis occurs by deposition of bone beneath the periosteum. 3. Regulation of Bone growth a. hormones: Growth hormone (primarily), Thyroid hormone, Sex hormones promote spike in growth at beginning of puberty & then induces the epiphyseal plate to close, ending growth. (approx. age 18 females, 21 for males) b. stress on bone (weights) IV. Types of Bone A. Compact Bone B. Spongy Bone 4. Disorders 1. osteoporosis Condition where bones are weakened due to loss of bone mass. Most common in post-menopausal women, men develop it to a lesser degree. About 30% of women have it between ages of 60-70. 70% have it by age 80. Estrogen deficiency strongly implicated b/c secretion of estrogen helps maintain bone density. Diet & exercise critical to maintaining healthy bone. Vitamin D is necessary to absorb calcium from the gut. (estrogen replacement therapy has been linked to higher risk of heart attack, stroke & breast cancer.) Whole skeleton affected but vertebral column & neck of femur are most vulnerable to breakage. V. Gross Anatomy Bone markings- see table 5.1 Bone surfaces reflect the stress placed on it. Bone markings are on the surface & unique to each bone. They are: 1) projections that are attachments sites for muscles & ligaments 2) surfaces that form joints 3) depressions & openings