stomach - eSSUIR
advertisement

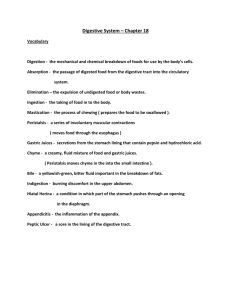
DIGESTION OF ORAL CAVITY AND STOMACH 1 ORAL CAVITY PHYSIOLOGICAL EVENTS 1. Ingestion 2. Mechanical digestion 3. Chemical digestion 4. Propulsion voluntary stage of swallowing 2 ORAL CAVITY 1. Ingestion of food is simply voluntarily taking food into the digestive tract through the oral cavity. 3 ORAL CAVITY 2. MECHANICAL PROCESSES Mastication As food enters the oral cavity the cheeks and the closed lips hold food between the teeth, the tongue mixes the food with saliva to soften it, and the teeth cut and grind it into a bolus. Suitable for swallowing Mastication is both voluntary and partly reflexive. 4 ORAL CAVITY 3. Chemical processes Chemical digestion of starch is begun by salivary amylase present in saliva. Saliva (1-1,5 liters per day) is a slightly acid solution of salts and organic substances secreted mainly by 3 pairs of salivary glands (parotid, buccal, submandibular glands). Basic saliva components: • Water 99.5% • Ions: Na+, K+, Ca2+, Cl–, HCO3– • Proline-rich proteins for protection of teeth enamel: - Enzymes: ptyalin (from salivary glands), **lingual lipase (secreted from glands on the tongue). - Immunoglobolins: IgA - Mucin: glycoproteins for lubrication of food and protection of oral mucosa - Lysozyme, lactoferrin, thiocyanate ions pH of saliva is about 7 Salivary flow ranges between 0.5 ml/min during basal flow and 5ml/min during maximum flow 5 ORAL CAVITY Other important (non-digestive) functions of saliva: Cleansing – Mouth and teeth kept free of debris, ect. Protection – Leucocytes, the enzyme lysozyme and antibodies act against some bacteria. Moistening and Lubricating – soft parts of mouth kept pliable for speech. Cells of oral mucosa protected from drying. Excretory – many organic substance (e.g. urea, sugar) and inorganic substance (e.g. mercury, lead) can be excreted in saliva. 6 ORAL CAVITY 4. PROPULSION The voluntary phase of deglutition is initiated by the tongue. The tip of the tongue is place on the hard palate, and then contracts which forces the bolus into the oropharynx. 7 Cerebral cortex Salivary center in medulla Other inputs Conditioned reflex Autonomic nerves Pressure receptors and chemoreceptors in mouth Simple reflex Autonomic nerves Salivary glands Salivary secretions 8 PHARYNX PHYSIOLOGICAL EVENTS 1. Chemical digestion Carbohydrate digestion continues. This is due to fact that the pH of the pharynx is slightly acid to neutral as is the oral cavity. No other marcomolecule begins chemical digestion. 9 PHARYNX 2. PROPULSION The pharyngeal phase of deglutition is initiated by food in the oropharynx. The presence of food causes the tongue to blocks off the oral cavity, the soft palate to rise and close off the nasopharynx. In addition, the larynx to rise so that the epiglottis covers the opening into the respiratory system, and the upper esophageal sphincter to relax and open. 10 Esophagus Bolus (moistened ball of chewed up food) is forced into the pharynx. The epiglottis prevents food from entering the trachea during swallowing, and passes bolus into the esophagus The esophagus is a muscular tube that connect pharynx to the stomach. The series of rhythmic contractions & relaxations is called peristalsis. Peristalsis pushes the bolus through the esophagus into the stomach. 11 The Swallowing Process Is also called deglutition Can be initiated voluntarily, Proceeds automatically Is divided in 3 phases: buccal phase – Compression of bolus against hard palate, Retraction of tongue forces bolus into oropharynx: pharyngeal phase – Bolus contacts: arches and posterior pharyngeal wall esophageal phase - Contraction of pharyngeal muscles forces bolus through entrance to esophagus Primary Peristaltic Waves 12 STOMACH 3 muscle layers: oblique, circular, longitudinal Regions: Cardiac sphincter Fundus Antrum (pylorus) Pyloric sphincter Vascular Inner surface thrown into folds – Rugae Contains enzymes that work best at pH 1-2 13 Functions of stomach Mix food Reservoir Start digestion of - Protein - Nucleic acids - Fats Activates some enzymes Destroy some bacteria Makes intrinsic factor – B12 absorption Absorbs - Alcohol - Water - Lipophilic acid - B12 14 Exocrine gastric glands Golbet cells mucus; Pariental cells hydrochloric acid (HCl); Chief (or zymogenic) cells pepsinogen, an inactive form of the protein-digestive enzime pepsin; Enterochromaffin-like (ECL) cells histamine and serotonin as paracrine regulalators of the GI tract; G cells gastrin into the blood; D cells hormone somatostatin. 15 STOMACH Mechanical digestion The walls of the stomach have several muscle layers. These muscles work together to churn the food, breaking up food particles and mixing them with gastric fluid. This results in a mixture called chyme. Chyme moves from the stomach to the small intestine. Gastric glands release gastric juice, a mixture of mucus, digestive enzymes, and hydrochloric acid. 16 STOMACH Gastric fluid carries out chemical digestion in the stomach Hydrochloric acid ensures a low pH in the stomach, dissolves minerals and kills bacteria An enzyme called pepsin begins the break down of proteins into peptide chains (chains of amino acids). Pepsin functions in a pH of about 2. Mucus coats the stomach and protects it from HCl & digestive enzymes • When the mucus coating breaks down allowing digestive enzymes to eat through part of the stomach lining, the result is called an ulcer. 17 STOMACH PROPULSION After a meal, peristalsis begins near the cardiac region and moves toward the pyloric sphincter. The intensity of the movements are due to the increase in the number of muscle layers of the stomach. 18 STOMACH The pyloric region of the stomach holds about 30 ml of chyme. It allows only liquids and small particles of chyme, about 3 ml, to pass through the valve for each peristaltic wave. The contractions of the pylorus decrease the opening of the valve. This results in the remaining chyme being remixed again and again. 19 STOMACH The rate of peristaltic waves is constant 3/min., however, the intensity can be modified. This contractile rhythm is set by the spontaneous activity of pacemaker cells located in the longitudinal smooth muscle layer. This cells establishes the basic electrical rhythm of the stomach. 20 STOMACH The stomach usually empties completely within 4 hours after a meal. The rate of gastric emplying depends on the contents of the duodenum as on what is happening in the stomach. 21 Mechanism for secretion of hydrochloric acid Extracellular fluid Pariental cell Lumen of canaliculus 22 Stomach neurological control 23 Stomach neurological control 1. CEPHALIC PHASE Slight, thought, taste, or smell of food causes stimulation of the vagus. The vagus stimulates the production of gastric juice. 24 Stomach neurological control 2. GASTRIC PHASE Vagovagal VAGOVAGAL REFLEX reflex Stomach distention will act locally or evoke the vagovagal reflex. 25 Stomach neurological control 3. INTESTINAL PHASE 26 27 Stomach hormonal control MECHANICAL DIGESTION 1. Gastrin--stimulate gastric emptying 2. 3. 4. 5. Serotonin--contraction ofsmooth muscle Somatostatin--inhibits motility and emptying Secretin--inhibits gastric motility Gastric Inhibitory Peptide--inhibits gastric motility 28 Stomach hormonal control CHEMICAL DIGESTION 1. 2. 3. 4. 5. Gastrin--stimulates gastric secretions Histamine--stimulates HCl formation Somatostatin—inhibits gastric secretions Secretin--inhibits gastric secretions Gastric inhibiory peptide--inhibits gastric secretions 6. Vasoactive intestinal peptide-inhibits HCl production 29 Stomach hormonal control PROPULSION 1. Gastrin--stimulates emptying 2. Somatostatin--inhibits gastric motility and emptying 3. Secretin--inhibits gastric motility and emptying 4. Gastric Inhibitory Peptide—inhibits gastric motility and emptying 30 Mouth break up food digest starch kill germs moisten food Stomach break up food digest protein kill germs store food 31