mucous + enzymes
advertisement

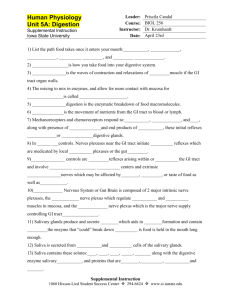
Mastication (Chewing) To grind & break food into small parts. Function Facilitate swallowing Mix food with saliva Stimulate tastebuds that affect secretion of saliva, stomach & pancreas Mechanism: Can be done voluntary. Most chewing is reflex in response to the present of food in mouth. Salivary Secretion 3 pairs of glands 2 parotids 20% Serous sec. Rich in enzymes 2 submandibular 70% Mixed secretion (mucous + enzymes) 2 sublingual 5% Mucous Buccal glands 5% Mucous Nerve supply: Symp. 1st & 2nd thoracic seg. relay in cervical ganglia Parasymp. 7th & 9th cranial cranial nerve facial glosso-phary. Composition of Saliva: Volume pH Tonicity 1-1.5 lit/day 6-7 i.e. acidic Hypotonic than plasma 99.5% 0.5% Water Solids Organic Mucous to lubricate food Enzymes Ptylin (S.amylase) Lingual lipase Lysozymes (antibacterial) Inorganic Na & cl less than plasm. K+ & HCO3- more than plasm. Functions of Saliva: 1. Swallowing moisten food particles lubrication by mucous. 2. Speech help movement of tongue & lips. 3. Solvent for substance to stimulate taste bicarbonate. 4. Antibacterial due to presence of lysozymes. 5. Buffer action due to presence of bicarbonate to prevent dental caries. 6. Excretion of drugs as Hg & I2. 7. Regulation of osmolality by sensation of thirst. 8. Digestion Saliva is not essential for digestion Starch amylase maltose Xerostomia: or arrested salivary secretion Dry mouth. Bad odor. Dysphagia (difficult swallowing). Dental caries. Difficulty in speech. Mechanism of Salivary Secretion: [1] Primary sec. = (Acini stage) contains enzymes mucous electrolytes very near to ECF [2] Secondary sec. = (Duct stage) Na+ K+ actively actively reabsorbed secreted Na+ in Saliva K+ in Saliva Na reab. > K+ secretion -ve 70 mv. inside duct. HCO3- are secreted by duct into lumen. HCO3- is exchanged with cl-. Duct is impermeable to H2O hypotonic. Characters of Saliva under Resting condition: Hypotonic Rich in K+ & HCO3- Poor in Na+ & cl- Characters of Saliva under Activity: Salivary flow is rapid time for electrolyte exchange Saliva Hypotonic (closer to isotonic) Less K+ & HCO3that of plasma Aldosterone hormone: Na+ & cl- K+ secretion reab. N.B.: If rate of salivary flow is rapid K+ loss. K+ in plasma. Hypokalemia. Muscle weakness & paralysis. High Na+ & cl- but still less than plasma Control of Salivary Secretion: Under nervous control Only why there is No hormonal control The hormonal control needs Time, while food in mouth Stay for very short time Basal Secretion of Saliva: Continuous & spontaneous. Occurs even in absence of stimuli. Is due to parasymp. Tone Control of secretion Unconditioned reflex (simple) Conditioned reflex (acquired) Unconditioned reflex: Food in mouth stimulate Chemoreceptors Pressure receptors Afferent 7, 9, 10 cranial nerves. Centre M.O. Efferent 7 & 9 cranial nerves. Response salivary secretion. N.B.: During dental procedures, salivary secretion is due to stimulation of pressure receptors. Conditioned Reflex (Acquired): Before food enters mouth. Sight, smell, odor, hearing thinking. Centre: Cerebral cortex +++ superior & inferior Salivary nuclei Afferent: 7th & 9th cranial nerves Response: Salivary secretion This reflex needs previous experience. Removal of cortex Loss of Cond. Re. Role of Autonomic Nerves: Parasymp. Symp. Dominant role Visicid True secretion Concentrated High volume ( water) Small volume Rich in enzymes Rich in mucous Cause dry mouth during stress N.B.: VIP is cotransmitter with ac. ch. VIP V.D not blocked by atropine The smooth muscles of G.I.T. are arranged in bundles. They are electrically connected with one another through gap junctions that allow low-resistance movement of ions from one cell to the next. So, each muscle layer functions as functional a syncytium. The pace maker cells of G.I.T smooth muscle are present in the circular muscle layer. These cells are called: Interstitial cells of Cajal These Cajal cells are self excitable like SA-node Electrical activity of G.I.T is divided into Basic electric rhythm = Slow wave potential = Resting membrane potential It is the passage of food from mouth to stomach. Started: Voluntary (Buccal phase) Completed: Involuntary (Pharyngeal & oesoph.) Controlled by: Deglutition Centre in M.O. Involves 3 phases Buccal (oral) 1 sec. Pharyngeal phase 2 sec. Oesophageal phase 8-10 sec. 1.Buccal phase (Oral phase): Voluntary lasts for 1 sec. Passage of food from mouth to phary. by contraction Hard palate of myelohyoid muscle. The bolus is on the dorsum of tongue The tip of tongue is in contact to hard palate. Bolus Tongue Tongue moves upward & backwards To push bolus into pharynx. We can stop deglutition in this buccal phase (bec. it voluntary). 2. Pharyngeal phase: Involuntary lasts 2 sec. Passage of food from pharynx to oesoph. When bolus is at oropharyngeal junction It stimulates: Pressure receptors Afferent : 5 & 9 cranial nerves. Centre : Deglutition centre in M.O. Efferent : 5, 9, 10 & 12 cranial n. Events: Palatopharyngeal folds: Approximate to prevent passage of large bolus into pharynx. Soft palate (uvula): Moves upwards to close posterior nasal cavity to prevent food entrance into nasal cavity. Respiration: Is inhibited i.e. reflex apnea for 2 sec. Vocal cords: Approximated. Larynx: Moves upwards & anterior to be covered by epiglottis. Anterior movement will open upper oesoph. sphincter. Pharyngeal muscles: Fast pharyngeal peristalsis to intrapharyngeal pressure to move bolus into oesophagus. It is Primary Peristalsis. Upper oesophageal sphincter: Is relaxed by the anterior movement of larynx. 3.Oesophageal phase: Involuntary. Passage of food from oesophagus into stomach. 2 types of peristalsis. Primary Peristalsis Secondary Peristalsis Continuation of peristaltic wave initiated in pharynx. Takes 8-10 sec. Occurs with each swallowing Controlled by swallowing centre in M.O. If food is remained in oesoph. wall. Food attached to oesph. wall will stimulate. Pressure receptors Local reflex from oesophageal myenteric plexus Very strong Powerful peristalsis to push food till reached to stomach. Sec. peristalsis occurs when primary fails to move food into stomach. Lower esophageal sphincter LES: Formed of circular muscle. It is Tonically contracted to prevent reflux of Hcl from stomach into oesoph. When peristalsis reaches lower end of esophagus, LES is relaxed to allow bolus to pass into stomach. Esophageal secretion: Only To lubricate food mucous No enzymes. To protect wall of esoph. from Hcl of stomach Motor disorders of esophagus: (1) Achalasia Failure of relaxation of LES. Due to: Damage of myenteric plexus. Accumulation of food in esophagus. Distension of esoph. Treatment: Antispasmotics to relax sphincter Surgical myotomy to dilate sphincter. (2) LES incompetence If LES is incompetent Hcl reflux from stomach to esoph. Heart burn. (3) Dysphagia: i.e. difficulty in swallowing Ex. Myasthenia gravis Paralysis of 5, 9, 10 cranial nerves.