Soft tissue disorders and fibromyalgia
advertisement

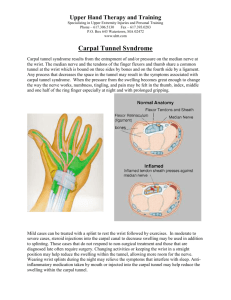
Soft Tissue Disorders and Fibromyalgia Jaya Ravindran Consultant Rheumatologist Introduction Definitions Approach to soft tissue disorders Overview of some soft tissue conditions: Flexor tenosynovitis De Quervain’s Carpal tunnel Golfer’s/Tennis elbow Rotator Cuff Trochanteric bursitis Achilles tendonitis Fibromyalgia • WHAT ARE TENDONS, LIGAMENTS, ENTHESIS AND BURSA? Definitions Ligament A band of tough connective tissue that connects bone to bone Tendon a tough band of fibrous connective tissue that connects muscle to bone Enthesis the point at which a tendon inserts into bone, where the collagen fibres are mineralised and integrated into bone tissue Bursa a fluid filled sac located between a bone and tendon which normally serves to reduce friction between the two moving surfaces • THOUGHT PROCESS/ISSUES IN SOFT TISSUE DISORDERS? Approach to soft tissue disorders History and examination paramount Differentiate from inflammatory/mechanical arthropathy Think about anatomy of area and mechanism of injury/overuse to understand pathology Work history Precipitating activity Approach to soft tissue disorders Could it be referred pain eg C5/6 Neck pain radiating to shoulder – ask about neurological symptoms May be associated with inflammatory arthritis eg RA or psoriatic arthritis or systemic illness Bloods not helpful in making diagnosis Imaging - X-ray and ultrasound may play a role in certain soft-tissue disorders • JOINT vs PERIARTICULAR? Is it an articular or extra-articular problem? • ARTICULAR PERI-ARTICULAR • • • • • pain in plane of tendon active > passive linear swelling localised tenderness localised erythema/heat pain all planes active = passive capsular swelling/effusion joint line tenderness diffuse erythema/heat Management Rest Simple analgesia NSAIDs Local steroid injection Physiotherapy/Occupational therapy Surgery in certain cases e.g. carpal tunnel • Features of flexor tenosynovitis ? Flexor tenosynovitis Inflammation of flexor tendon sheaths Pain and stiffness in flexor finger/thumb, may extend to wrist Reduced active flexion, crepitus, thickened tender tendon sheaths May be associated with nodule – “trigger finger” Can be associated with RA, Diabetes Treatment – injection hydrocortisone, surgery • Features of De Quervains? De Quervain’s (tenosynovitis) Inflammation of tendon sheath containing extensor pollicis brevis and abductor pollicis longus tendons De Quervain’s (tenosynovitis) Pain, swelling radial wrist Localised tenderness, crepitus, pain worse over radial styloid Finkelstein’s test De Quervain’s (tenosynovitis) Finkelstein With the thumb flexed across the palm of the hand, ask the patient to move the wrist into flexion and ulnar deviation. Positive if reproduces pain De Quervain’s (tenosynovitis) Management Rest from precipitating activity Splintage Steroid injection surgery • Features and causes of carpal tunnel syndrome? Carpal tunnel syndrome Compression of median nerve as it passes through carpal tunnel Carpal tunnel syndrome Common, F>M, elderly/middle aged Mostly idiopathic Associated with (particularly if bilateral): Diabetes Hypothyroidism RA Pregnancy Acromegaly Vasculitis Trauma Others (e.g. amyloid, sarcoid) Carpal tunnel syndrome anatomy Median nerve supplies: Motor (beyond carpal tunnel in hand) L lateral two lumbricals O opponens pollicis A abductor pollicis brevis F flexor pollicis brevis Sensory Palmar surface thumb, lateral 2 ½ digits Carpal tunnel syndrome Clinical features Numbness/parasthesia in median nerve distribution Pain, can radiate up arm Worse at night ‘Hang hand over end of bed’ Weakness of thumb (abduction) Thenar wasting Positive Tinel’s/Phalen’s Carpal tunnel syndrome Tinel’s Phalen’s Carpal tunnel syndrome Investigation Nerve conduction studies show reduce nerve conduction velocities across wrist Management Avoidance of precipitating activity Night time splints Local steroid injection Surgery – division of flexor retinaculum and decompression of carpal tunnel (80% success) • Features of epicondylitis ? Tennis & Golfer’s Elbow Both enthesopathies Tennis elbow = lateral epicondylitis = inflammation common extensor origin Golfer’s elbow = medial epicondylitis = inflammation common flexor origin Tennis elbow more common than Golfer’s Tennis & Golfer’s Elbow Pain localised to specific area Elbow flexion/extension does not cause pain Pain upon: resisted wrist extension (Tennis) resisted wrist flexion (Golfer’s) Tennis & Golfer’s Elbow Management Rest from precipitating activity Elbow clasps Local corticosteroid injection Physiotherapy – ultrasound and acupuncture Surgery (often ineffective) • Rotator cuff disease features? Rotator Cuff Pathology A range of various conditions, including: Supraspinatous tendinitis/rupture Rotator cuff tear Adhesive capsultitis (frozen shoulder) Acute calcific supraspinatous tendonitis Subacromial bursitis Acromioclavicular joint OA Overlap in clinical features but distinct entities Rotator Cuff – anatomy A sheath of conjoint tendons to support glenohumeral joint, made up of: S I T S supraspinatous - abduction infraspinatous – external rotation teres minor – external rotation subscapularis – internal rotation Rotator Cuff Syndrome Spectrum from mild supraspinatus tendinitis to complete tendon rupture Chronic impingement of cuff under acromial arch Pain often over acromial area extending into deltoid Rotator Cuff Syndrome Painful mid arc Impingement test – abducted, flexed and internally rotated Supraspinatus stress Rotator cuff investigation - ultrasound • Full thickness tear Rotator Cuff Syndrome Management Rest, NSAIDs Local steroid injection around tendon – subacromial space and PT If chronic/rupture refer to Orthopaedics for surgical opinion Acute calcific supraspinatus tendinitis Calcium hydroxyapatite deposition near supraspinatus enthesis Young adults, F>M, acute pain over several hours Normally resolves over few days Treatment Minor – NSAID Moderate – consider steroid injection Severe – consider aspirating calcified material Adhesive capsulitis (Frozen shoulder) Progressive pain and stiffness Global reduction in movement, but particularly external rotation Three phases Pain (3-5 months) Adhesive phase (4-12 months) Recovery phase (12-42 months) Adhesive capsulitis (Frozen shoulder) Associated with diabetes Most patients recover by 30 months, but still have reduced movements Management Analgesia, NSAIDs, Physiotherapy, steroid injection Surgical opinion in difficult cases (manipulation under anaesthesia) • ACJ disease features ? Acromioclavicular OA • High arc pain • Local tenderness • Adduction painful • Impingement • Trochanteric bursitis features? Trochanteric bursitis Inflammation of the superficial and deep bursa that separates the gluteus muscles from the posterior and lateral side of the greater trochanter of the femur Trochanteric bursitis Boring pain over lateral aspect of hip May radiate down lateral thigh Worse on walking or lying in bed at night Localised tenderness upon pressure over greater trochanter Trochanteric bursitis Management Rest Analgesia Steroid injection Physio Achilles tendonitis Inflammation of the achilles tendon Sometimes at enthesis Sometimes in middle avascular portion of tendon Can be seen with seronegatives Achilles tendonitis Chronic tendonitis can lead to Achilles tendon rupture Aetiology of tendonitis though to be avascular degeneration of tendon Tenosynovitis does not lead to rupture Also can get acute traumatic rupture All have localised pain and swelling of Achilles tendon, with difficulty walking Achilles tendonitis Investigation - ultrasound Management Rest, NSAIDs, physiotherapy Local steroid injection under U/S guidance into paratenon can help tenosynovitis – if no evidence of tear Achilles rupture Acute rupture – sudden calf pain as if being hit on back of leg Palpable gap in tendon Some but little plantarflexion Squeeze calf whilst prone - no plantarflexion in affected leg (Simmond’s) Management Surgery to repair tendon Conservative – below knee cast in ankle equinus 6 weeks • Fibromyalgia features ? Fibromyalgia • • • • • • • • “All over pain” Fatigue Sleep disturbance Depression Anxiety Irritable bowel Tender spots Diagnosis of exclusion Prevalence/Risk Factors Common Approx 2-5% depending upon definition Female (F:M ratio between 3:1 and 7:1) Middle age (typically 30-60) Differential diagnosis Other conditions can mimic fibromyalgia: Systemic lupus erythematosus (SLE) Hypothyroidism Polymyalgia rheumatica Malignancy Myopathy Metabolic bone disease Management Patient education About condition Reassure that no serious pathology No harm in exercising Cognitive behavioural therapy (CBT) Low dose amitriptyline Graded aerobic exercise regime THANK-YOU