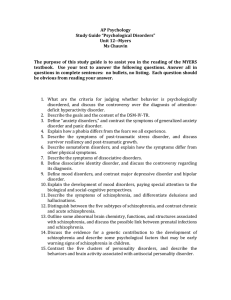
Presentation
advertisement

AP Psych—Ch. 14: Psychological Disorders (Abnormal Psychology) Also known as “psychopathology” 1 A Statistical Approach Norm = average, median In statistics, normal = things characteristic of the majority of the group The statistical approach doesn’t differentiate between “desirable” and “undesirable” behavior For example, a statistical model assessing intelligence would view both geniuses and mentally retarded people as “abnormal” because they’re not characteristic of the majority of society. In actuality, society does not refer to geniuses as “abnormal” because we see intelligence as a desirable trait. 2 Criteria of Abnormal Behavior Deviance Behavior that deviates from what society considers acceptable Culturally driven Maladaptive Behavior Interferes with social or occupational functioning Personal Distress *Don’t need all 3 to have 3 a disorder Psychological Classification A Medical Model •making the assumption that mental illness can be described in the same manner as any physical illness. •Diagnosis—distinguishing one illness from another •Etiology—cause & history of an illness •Prognosis--Forecast about the probable 4 course of an illness Diagnostic and Statistical Manual of Mental Disorders 1952: American Psychological Association agreed upon a standard system for classifying abnormal behavior It has been revised five times Most recent revision (DSM-V) in May 2013 Previous revision: 1994 5 Before the DSM The two most commonly diagnostic distinctions were “neurosis” and “psychosis” Neurotics struggled with certain mental conditions, but still remained connected with reality. Psychotics referred to those who had lost touch with reality “Neurotics build dream castles in the air, the psychotics move in, and the psychiatrists collect the rent.” These terms have been replaced but are still used by many psychologists 6 New Categories Anxiety disorders Somatoform disorders Dissociative disorders Mood disorders Schizophrenia Personality disorders 7 Categories of Mental Disorders Anxiety Disorders Generalized anxiety disorder Phobic disorder Panic disorder Obsessive-Compulsive disorder Post-traumatic stress disorder Somatoform Disorders Psychosomatice disorder Somatoform disorder Conversion disorder Hypochondriasis • Dissociative Disorders • Dissociative amnesia • Dissociative fugue • Dissociative identity disorder • Mood Disorders • Depression • Dysthymic disorder • Bipolar disorder • Cyclythymic disorder • Schizophrenic Disorders • Paranoid schizophrenia • Catatonic schizophrenia • Disorganized schizophrenia • Undifferentiated schizophrenia • Personality Disorders • Antisocial personality disorder • Other personality disorders 8 DSM-IV Descriptions 1. 2. 3. 4. Essential features of the disorder Associated features present Information on differential diagnosis Diagnostic criteria *All so that it will reduce the chances that one doctor might diagnose a patient as schizophrenic while another diagnoses the same patient as bipolar. 9 10 Axis 1: Clinical Syndromes Axis I disorders: first diagnosed in infancy, childhood, adolescence Attention deficit, brain damage, substance abuse, schizophrenia, moods, anxiety, somatoform, dissociative, sexual, eating, sleep, impulse control What brings you in to see a doctor in the first place 11 Axis II: Developmental Disorders/Personality/Mental Retardation Compulsiveness Over-dependency Aggressiveness Language disorders, reading or writing difficulties, autism, speech problems 12 Axis III: Physical Disorders General medical conditions Diabetes, arthritis, hemophilia, etc… Brain damage (e.g., a tumor or aneurysm) Chemical imbalances *Physical problems that could be causing Axis 13 I/II disorders Axis IV: Measurement of Current Stress Level life changes or events that cause particular stress in a person’s life and contribute to illness and pathology Death of a spouse Loss of a job Based on stress in the last year (Holmes & Rahe SRRS) Stress contributes to 80% of all diseases 14 Axis V: Adaptive Functioning Social relations Occupational functioning Use of leisure time “Global Assessment of Functioning” 15 16 Anxiety Disorders: Characteristics Excessive fear or dread in response to a real or imagined danger Out of proportion to the situation Worry, mood swings, headaches, weakness, sweating, fatigue, feeling that one is in danger 17% of the population 17 Types of Anxiety Generalized anxiety disorder (GAD) Phobic disorder Panic disorder Obsessive-compulsive disorder (OCD) Post-traumatic stress disorder (PTSD) 18 Generalized Anxiety Disorder Chronic, high level of anxiety that is not tied to any specific threat Panic attacks (chest pain, choking, trembling, diarrhea, reduced appetite, indigestion)—but not all the time Can’t make decisions, trouble with family Physical complaints May be genetic; arises 19 following major life changes Phobic Disorders Severe anxiety about a particular object, animal, activity, or situation Types: specific Social (agoraphobia) See pg. 578 http://www.phobialist.com/ 20 Panic Disorders A feeling of sudden, helpless terror A sense of impending doom or death Smothering, choking, faintness, difficulty breathing, nausea, chest pain 21 Obsessive-Compulsive Disorder Obsession: thinking the same thoughts over and over again Compulsion: performing irrational acts May have a genetic basis Video Clip—20 year old girl w/OCD 22 Post-Traumatic Stress Disorder (PTSD) NPR audio article: Ending Nightmares Caused by PTSD After a traumatic event, severe, long-lasting effects Flashbacks, night-mares or night terrors, anxiety, insomnia Combat vets, victims of rape or assault, survivors of disasters Combat veterans, rape/assault victims, disaster survivors 23 Etiology (cause) of Anxiety Disorders Biological Factors concordance rate (% of twin pairs with the same disorder)— slight genetic similarity; anxiety sensitivity—some people are more sensitive to the internal physiological symptoms of anxiety & then overreact with fear Conditioning and Learning Classical—traumatic experience made a neutral stimulus a conditioned stimulus Operant—avoiding what you’re scared of-negative reinforcement Evolutionary—historical threats (bugs/snakes) vs. modern threats (irons/outlets) Observational—watching how parents respond to threats… Etiology (cause) of Anxiety Disorders (cont’d) Cognitive Factors Focusing too much attention on perceived threats Misinterpreting harmless situations as threatening Selectively recall information that seems threatening (The doctor examined little Emma’s growth) Personality Neuroticism (people who are self-conscious, nervous, jittery, insecure, guilt-probe, & gloomy) Stress Positive correlation between high stress & anxiety 25 Psychosomatic and Somatoform Disorders Psychosomatic disorders: involve real, identifiable physical illnesses; caused by stress or anxiety Somatoform disorders: symptoms appear that are not characteristic of any readily identifiable disease; no organic cause Two types of somatoform disorders: conversion disorder, hypochondriasis Conversion Disorder occurs when a person “converts” psychological and/or emotional distress into physical symptoms, usually to avoid dealing with a painful or stressful situation in their lives Conversion of emotional difficulties into the loss of a specific body function rare and involve severe physical problems such as paralysis, numbness, seizures, blindness, and deafness No physical damage Because conversion disorders offer a way to avoid stress and pain, sufferers often accept their physical problems with relative calm, remaining unconcerned or even cheerful about their condition. 27 Conversion Disorder (examples) Glove anesthesia Sufferers experience a complete lack of feeling from the wrist down, retaining sensation in the rest of the arm anatomically impossible: the nerves of the hand and arm blend together, so if a person really had nerve damage affecting their hand, it would affect their arm as well. Another type of conversion disorder involves paralysis of the legs; however, the sufferer is sometimes seen sleepwalking at night. 28 Hypochondriasis People with hypochondriasis interpret any small physical ailment they have (such as minor aches, bumps, or bruises) as a sign of a serious illness. Looks for signs of serious illness Found most often in young adults Occurs equally in men and women 29 Etiology of Somatoform Disorders Highly active autonomic system? Personality Factors (especially histrionic personalities—self-centered, suggestible, excitable, highly emotional, overly dramatic) Cognitive Factors (good health=complete absence of symptoms and discomfortunrealistic) The Sick Role Indirect benefits like avoiding everyday challenges, having an excuse for failure, people demand less from you, attention from 30 others Dissociative Disorders A person experiences alterations in memory, identity, or consciousness Includes amnesia and multiple personalities 31 Dissociative Amnesia Memory loss with no biological explanation (form of selective forgetting) Blotting out painful experiences & repressing it to into their unconscious Total amnesia is very rare 32 Dissociative Fugue Amnesia coupled with active flight May establish a new identity Repression of past knowledge May last from days to decades “Traveling amnesia” 33 Dissociative Identity Disorder Multiple personalities (two or more distinct identities, each with their own way of thinking and behaving) usually relates to severe physical or sexual abuse suffered as a child Different personalities in control at different times Case studies 34 Etiology of Dissociative Disorders Excessive stress Severe emotional trauma? Certain personality traits Fantasy-proneness Some think it is intentional roleplaying to avoid personal failings Mostly unknown because of its rarity Only about 25% of American psychiatrists believe in DID (1999) 35 Schizophrenia and Mood Disorders “Schizophrenia” = “split mind” Schizophrenia--severe disorder that involves disordered thoughts, extreme emotions that have nothing to do with any particular situation, and very strange behavior Mood disorders--person experiences unusual, prolonged changes in their mood or emotions. The most common mood disorders are depression and mania. Depression--overwhelming feelings of despair, sadness, and hopelessness, a severe drop in self-esteem, leading to feelings of worthlessness and self-hatred Mania--opposite of depression: afflicted people feel incredibly happy (bordering on euphoric), energetic, and gregarious 36 What Is Schizophrenia? Distortion/disturbance of cognition, emotions, perception, and motor functions Can lead to brain damage Confused, disordered thoughts Affects 1 in 100 Odds increase 1 to 10 if it runs in the family 37 Schizophrenia (cont.) Loss of contact with reality Lives life in an unreal dream world Delusions, disembodied voices, & vivid hallucinations No single cause or cure Psychotropic drugs can help block out the schizophrenic voices Collection of symptoms “Rule of Thirds”—1/3 gets better, 1/3 stays the same, 1/3 gets worse 38 Symptoms of Schizophrenia Delusions/paranoia Hallucinations (visual or auditory) Incoherent or marked decline in thought Language changes Speech sounds like gibberish & unrelated words thrown together Inappropriate Affect (emotion Sluggish emotions Movement changes Diverted attention (cognitive “flooding” that erodes their ability to focus) 39 Types of Schizophrenia Paranoid Catatonic Disorganized Undifferentiated 40 Paranoid Schizophrenia Complex delusions Perceived persecution Hallucinations of smell, taste, other bodily sensations Usually NOT visual hallucinations Unseen voices that give them commands Belief that they have a special mission Jani 41 Catatonic Schizophrenia moves back and forth between a waking state in which they often become quite active and even agitated, and a catatonic state Catatonic state: mute, immobile, mostly unresponsive “Waxy flexibility” Unusual postures held for long periods of time 42 Disorganized Schizophrenia Disturbed and Incoherent language Inappropriate emotions Disorganized motor behavior Hallucinations (visions) and delusions 43 Undifferentiated Schizophrenia Deterioration of daily functioning Hallucinations and delusions Inappropriate emotions Thought disorder Doesn’t fit the other 3 types, but has symptoms from them 44 Remission No cure exists for schizophrenia, but some sufferers do have periods where their symptoms become greatly reduced or disappear completely. Psychologists refer to this as “remission” because symptoms almost always return eventually. Symptoms are completely gone or still exist but are not severe enough to have earned a diagnosis of schizophrenia in the first place 45 Etiology of Schizophrenia Genetic Biochemistry/brain structure Environment 46 Genetics and Schizophrenia 1% chance in general population 10% chance if it runs in the family Adoption model studies One study looked at schizophrenic mothers who gave birth to twins, one was given up for adoption. Even though the twins grew up in different environments, about 16% of them went on to develop schizophrenia. Not conclusive 47 Biochemistry/Brain Structure Psychosis results from chemical imbalances in the brain Brain abnormalities Creates chemical imbalances Stress may knock the brain’s mechanisms for processing information out of kilter and interfere with normal synaptic transmission. Creates biochemical changes May not cause schiz but can contribute to its development The dopamine hypothesis schizophrenia results from an excess of the neurotransmitter dopamine at certain synapses 48 CAT Scans and MRIs Brains of identical schizophrenic twin has enlarged ventricles. When these ventricles fill with fluid, they enlarge and reduce the space available for brain tissue. 49 Neurodevelopmental Hypothesis Schiz may be caused by insults or disruptions in the normal maturational processes of the brain before birth, causing subtle neurological damage that elevates vulnerability to schiz later on Insults=viral infections or malnutrition during prenatal development or obstetrical complications during birth 50 Family Experiences/Interactions Bad experiences during childhood are not enough to lead to schizophrenia Pathogenic (unhealthy family may contribute to problems)—High expressed emotion (EE) Diathesis-stress hypothesis although an individual may have inherited a predisposition toward schizophrenia, the person must be exposed to certain environmental stressors for it to develop. 51 Mood Disorders 52 Seasonal Affective Disorder (SAD) A type of depression Affects people in most northern areas of the world Less light available in winter = more melatonin secreted by the pineal gland Melatonin regulates sleep cycle and has been linked to mood and depression Less daylight also seems to affect neurotransmitters that regulate the body’s internal clock, including norepinephrine, serotonin, and dopamine. Treatments: temporary sleep deprivation (to reset biological clock), exposure to artificial light Usually as winter begins to end and the days start to get longer, the depression seems to lift and eventually disappear. 53 Suicide Every year, more than 32,000 Americans end their own lives. One suicide occurs every 16 minutes. Escape from physical or emotional pain, terminal illness or loneliness, old age Women attempt suicide more often than men, but men are more likely to succeed. occurs more commonly among the elderly and college students (2nd leading cause of death among college students) Desire to end “unacceptable” feelings (especially sexual feelings) Attempt to “punish” loved ones who they feel should have perceived and attended to their needs 70% of those who threaten suicide kill themselves within 3months of making the threat. 54 Kurt Cobain Even people who seemingly “have it all” commit suicide sometimes. Musician Kurt Cobain’s band Nirvana was at the top of the charts when he killed himself with a shotgun. He left behind a note: one sentence in it stated, “I’m too much of an erratic, moody baby! I don’t have the passion any more and so remember, it’s better to burn out than to fade away.” 55 Major Depressive Disorders Severe forms of depression that interfere with functioning and concentration Symptoms: lack of appetite, insomnia, and noticeable weight changes (either an increase or decrease). Effects: hopelessness, suicidal impulses, feeling of worthlessness 56 Bipolar Disorder (formerly “manic depression”) Sufferers alternate between despair and mania Manic phase: elation, confusion. (Sometimes this phase gets mistaken for a spurt of creativity. ) Depressive phase: same as for people with major depression Length of phases varies from person to person 57 Etiology of Mood Disorders Genetic vulnerability Neurochemical factors Cognitive factors (learned helplessness) Stress 58 Genetic Vulnerability (Mood disorders) Genetics plays a strong role High concordance rate Heredity creates a predisposition to mood disorders, but environmental conditions convert it to a disorder Genetics may play a higher role in men than women Genetics may be a bigger factor in bipolar disorder than unipolar disorders 59 Neurochemical factors Correlation between mood disorders and the activity of norepinephrine and serotonin Decreased NE=depression Increased NE=mania Unbalanced levels of serotonin No simple neurochemical explanation…complex alterations in neurotransmitter activity 60 Cognitive Factors Martin Seligman”Learned Helplessness Model” Learned helplessness=passive “giving up” behavior produced by exposure to unavoidable aversive events (like uncontrollable shocks in a lab) Roots of depression lie in how people explain the setbacks & other negative events they experience People with a “pessimistic explanatory style” are more vulnerable to depression (glass is half empty) (blame personal flaws instead of 61 situational factors) Hopelessness Theory Pessimistic explanatory style + high stress + low self esteem = hopelessness which = depression Susan Nolen-Hoeksema—people who ruminate about their depression stay depressed longer than people who try to distract themselves Negative thinking is what leads to depression 62 Interpersonal Roots Correlation between poor social skills and depression Depressed people are ….depressing, so people tend to want to be around them less and they end up with fewer sources of social support 63 Stress and Mood Disorders Moderately high link between stress and the onset of mood disorders Stress affects how people respond to treatment and likelihood of a relapse 64 Personality Disorders • People with personality disorders do not suffer from anxiety, nor do they usually behave in bizarre ways. • Instead, they are unable to establish meaningful relationships. • wide range of self-defeating patterns and behaviors, from being painfully shy to acting vain and pushy. • displays an inflexible, long-standing, and maladaptive way of dealing with other people. Ted Bundy--murdered at least 37 young women all across the nation. He was well-educated, articulate, and charming. Even while sitting on death row, he never showed any remorse for his crimes. Some psychologists believed that Bundy had a personality disorder that prevented him from establishing a normal, intimate relationship with a woman. When combined with his intelligence, his amoral nature, and his lack of a conscious, it 65 produced a deadly, pathological mix. Types of Personality Disorders Anxious/fearful Cluster—Maladaptive efforts to control anxiety and fear about social rejection (maladaptive=adapting poorly) Avoidant Personality Disorder Dependent Personality Disorder Sensitivity to potential rejection, humiliation or shame Socially withdrawn in spite of desire for acceptance from others Excessive lack of self-reliance & self-esteem Needs others to make decisions Constantly putting others’ needs above their own Obsessive-Compulsive Personality Disorder Preoccupied with organization, rules, schedules, lists Extremely conventional, serious & formal 66 Odd/Eccentric Cluster Distrustful, socially aloof and unable to connect with others emotionally Schizoid Personality Disorder Schizotypal Personality Disorder Cannot form social relationships Absence of warm & tender feelings for others Social deficits Oddities of thinking, perception & communication Mild form of schizophrenia Paranoid Personality Disorder Pervasive & unwarranted suspicious & mistrust of people Overly sensitive Prone to jealousy 67 Dramatic/Impulsive Cluster Overdramatizing personalities Histrionic Personality Disorder Narcissistic Personality Disorder Grandiosely self-important Preoccupied with success fantasies Expect special treatment No interpersonal empathy Borderline Personality Disorder Overly dramatic Exaggerated expressions of emotion Egocentric, seeking attention, provocative dressing Unstable in self-image, mood, and interpersonal relationships Impulsive & unpredictable Antisocial Personality Disorder 68 Antisocial Personality serial killer Jeffrey Dahmer Exhibits a persistent disregard for and violation of others rights Shallow emotions; don’t think about consequences of their actions Lacks a conscience, lives for the moment Serial killers Many have antisocial personalities Many abuse alcohol or drugs Most were abused—emotionally, physically, and often sexually—as children. (Abuse only served as a contributing factor.) Some serial killers believe that they are doing something good for the society by killing certain types of people. According to psychologist Joel Norris, almost a third of 69 serial killers cannibalize their victims. Reasons for Antisocial Behavior Imitation of one’s own antisocial parents Lack of discipline or inconsistent discipline Faulty nervous system; genetic 70 Psychological Disorders and the Law M’naghten Rule Daniel McNaghten Woodworker in 19th century Scotland Had delusions and paranoid schizophrenia Thought he was the target of a conspiracy involving the Pope and British Prime Minister Robert Peel 1843-tried to assassinate Peel but killed his secretary instead “delusional” so acquitted by rule of insanity Public outrage, but it became a law the next year The Insanity Defense 71 Involuntary Commitment Danger to self Danger to others In need of treatment 72 Therapy and Change 73 74 The Nature of Psychotherapy “Healing of the soul” The term “mental illness” has outlived its usefulness; mental stigma associated with that phrase Thomas Szaz--alternate view of abnormal behavior, portraying it not as an illness but merely as a deviation from society’s normative structure characterized mental illness as a form of cultural myth and that people labeled as mentally ill simply have problems coping in society 75 “problems in living” Functions of Psychotherapy Learning to be responsible for one’s behavior Take control of one’s life Understanding how one’s current way of living can cause problems; believe change is possible Therapist acts as a guide 76 Main Kinds of Therapy Psychoanalysis Humanistic approach Cognitive approach Behavioral approach Biological approach Eclectic approach 77 Types of Therapists Clinical psychologists (Ph.D) Counseling psychologists (MA) Clinical neuropsychologists (Ph.D) Psychiatrists (medical doctor) Psychoanalysts (Freudian) Social workers, nurses 78 Common Methods Used…. Discussion Advice Emotional Support Persuasion Advice Relaxation training Role Playing Drug therapy Biofeedback Group therapy 79 What Are the Qualities of a Good Therapist? Empathy & understanding Psychologically healthy Must be able to create a comfortable, safe atmosphere 80 Group Therapy Patients work together with the aid of a leader/therapist to resolve interpersonal problems Advantages Cheaper than one-onone therapy Helps with high patientto-staff ratios in mental hospitals 81 Family Therapy Observes interactions Establishes an objective point of view Identifies patterns that lead to problems Helps untangle the web of communication 82 Self-Help Groups People who share a particular problem (like alcoholism, cancer survivors, abuse survivors, parents of terminally ill, or drug addictions) Conducted without a professional AA, ALANON, ALATEEN (12 step model) 83 Does Psychotherapy Work? Hans Eysenck (1952): psychotherapy is no more effective than no therapy at all (2/3 of people get better within two years w/o therapy) Allen Bergin (1971): challenged Eysenck’s methodology (most people make at least moderate improvements) Smith & Glass (1977): meta-analysis (combining results of a number of studies and analyzing them) also disagreed with Eysenck; some therapy is better than none; most forms of therapy have similar rates of effectiveness 84 Insight Therapies (“talk therapy”) Originally based on the tradition of Freud’s psychoanalysis Complex verbal interactions intended to enhance clients’ selfknowledge and promote healthful changes in personality and behavior Individual or groups (includes family & marital therapy) 85 What Is Psychoanalysis? Insight therapy Developed by Freud based on the theory that psychological problems result from anxiety about feelings and thoughts a person has repressed into their unconscious Therapy aimed at making patients aware of their unconscious motives so they can gain control of their lives 86 Free Association A method used to examine the unconscious Patients say whatever comes into their mind Patients are strongly encouraged not to “edit” themselves so that they can achieve a true “stream of consciousness.” psychiatrist often says nothing for long periods of time Resistance (reluctant to reveal painful or embarrassing things) Slow process (years) 87 Transference Sooner or later, the patient reaches a level of comfort with their analyst. A process in which patients take feelings toward some other person and transfer these feelings to the analyst (feelings for parents toward analyst) Transference can be either positive or negative: patients can feel good about their analysts or they can take out their negative feelings on them the therapist does not take anything the patient says personally, remaining neutral 88 Humanistic/Client-Centered Therapy Insight therapy Focuses on a person’s value, dignity, worth Reflects the belief that the client and therapist are partners Supportive emotional climate The client plays a major role in determining the pace & direction of therapy 89 Client-Centered Therapy (CCT) Carl Rogers believed the term “patient” suggests inferiority, while the term “client” implies an equal relationship Therapist shows real caring and empathy; assumes people are basically good Need to become self-actualized Unconditional positive regard/empathy (respect and empathy no matter what they might say) techniques often involved repeating much of what he would hear from his clients in order to help them clarify their feelings. 90 Cognitive Therapy Goal is to change the way people think It assumes that negative and/or incorrect beliefs, expectations, and ways of thinking can distort behavior. helps people modify their behavior by changing misconceptions they have about themselves and society in general. Behavior modification: a systematic method for changing the way a 91 person acts and feels Cognitive Therapies: Similarities All types of cognitive therapy operate under the same basic principles. Disconfirmation-- confronting patients with specific evidence that directly contradicts their existing beliefs Reconceptualization-- process in which the therapist helps patients develop an alternative belief system to explain their experiences and observations. Insight-- clients work toward an understanding 92 of how they arrived at these new beliefs. Rational-Emotive Therapy (RET) Albert Ellis aimed at changing unrealistic assumptions (“everything I do must be approved by others” or “I need to be loved by everybody.” ) People behave in rational ways Role playing Wanted to correct these false & self-defeating beliefs For example, if a client believed he would never have any success with women, Ellis would have him practice his skills at asking for a date. He would then direct the patient to ask out women whom the patient believed would be likely to reject him. This experience would help the client learn that he can cope with things not going his way. May be called REBT (Rational-Emotive Behavioral Therapy) 93 Ellis’s A B C Ellis claimed that experiences by themselves don’t cause psychological problems; rather, it is the way a person thinks about the experience that leads to troubles. In other words A does not cause C, rather B causes C. 94 Aaron Beck’s Cognitive Therapy Maladaptive thought patterns cause a distorted view of oneself and lead to problems Therapists use persuasion and logic to try to help patients change existing beliefs. For example, if a client believes that he or she never has a good time, the therapist might point out that this is a hypothesis, not a fact. The therapist might then ask the client to test the hypothesis by looking at the evidence differently, and note the times in their lives when they did in fact have a good time. Works well with depressed people Beck theorized that depressed people blame themselves for their problems rather than their circumstances. He also believed that depressed people focus on only negative events and ignore positive events, which leads them to make pessimistic projections about the future and undermine their self-esteem and sense of worth. 95 Behavioral Therapies Changing undesirable behavior through conditioning. assumes that people become disturbed because they have learned to behave in an undesirable way and that any behavior learned can also be unlearned Don’t spend time going over the past Focus on producing a change in behavior; thoughts will follow 96 Systematic Desensitization A technique used to help a patient overcome irrational fears and anxieties Pairs relaxation techniques with anxiety-producing situations Pic of snake touching a snake Counter-conditioning 97 Counter-conditioning 1. The person builds an “anxiety hierarchy,” with the least feared situation at the bottom and the most feared at the top. 2. The person practices deep muscle relaxation techniques. 3. Eventually, the person learns to use these relaxation techniques to cope with each situation in the hierarchy. 98 Flooding • Directly exposing a patient to the object or situation they fear. •If scared of water, the therapist would have the hydrophobic patient wade out a little deeper each time (usually the therapist would accompany them). 99 Modeling Patients and therapists first analyze anxiety-arousing situations step by step. The therapist then gradually exposes the patient to real-life situations and models (demonstrates) the desired behavior. 100 Aversive Conditioning Links an unpleasant state with an unwanted behavior in an attempt to eliminate the behavior Use of drugs with alcohol that cause nausea (dysulfurum) 50% success rate; takes 6 months 101 Operant Conditioning Behavior that is reinforced tends to be repeated Contingency management: undesirable behavior is not reinforced, while desirable behavior is reinforced Used in prisons and mental hospitals 102 Token Economies Desirable behavior is reinforced with valueless objects or points which can be accumulated and exchanged for various rewards Use of “hospital or token money” 103 Cognitive Behavior Based on a combination of substituting healthy thoughts for negative thoughts focuses on setting goals and changing the client’s interpretation of their situation designed to help clients differentiate between serious, real-life problems and imagined or distorted ones 104 Biological Therapy Assumes an underlying physiological problem Medication, electric shock (ECT), psychosurgery Must be administered by a psychiatrist Used when talking and learning theories do not work 105 Drug Therapy Psychopharmacotherapy Drug therapy tries to help patients by manipulating levels of neurotransmitters in the brain tries to help patients by manipulating levels of neurotransmitters in the brain For example, one theory of schizophrenia postulates that people develop the disease when their dopamine receptors become overactive. Three major groups Antipsychotic drugs Antidepressant drugs Antianxiety drugs 106 Antipsychotic Drugs Treating schizophrenia AKA Neuroleptics Examples: Thorazine &Haldol: blocks or reduces the sensitivity of the dopamine receptors Clozapine: decreases dopamine levels while simultaneously increasing serotonin levels Decrease activity at the dopamine synapses Side effect: Tardive Dyskinesia muscle rigidity, tremors, and coordination problems. Antidepressants works on neurotransmitter levels and are used to treat anxiety, phobias, and obsessive compulsive disorder (OCD). MAO inhibitors (MAOIs), tricyclics SSRIs (Selective Serotonin Reuptake Inhibitor) Can also treat OCD & Panic disorders Increase the amount monoamines, norepinephrine, or serotonin SSRI’s—usually have less size Some affects (Prozac, Paxil, Zoloft, antidepressants also Wellbutrin) used for anxiety. 108 Lithium Carbonate Lithium is a naturally occurring salt that controls levels of norepinephrine A chemical used to treat mood swings or bipolar disorder Very dangerous side effects Acute toxicity sometimes used to treat severely depressed and suicidal people 109 Anti-Anxiety Drugs Benzodiazepines (Tranquilizers like Valium, Xanax) Relieve anxiety and panic disorders by depressing the activity of the CNS Makes you drowsy More mild than other drug therapies Lethal when mixed with alcohol 110 Electroconvulsive Therapy (ECT) • Used mostly for severe depression • The shock is intended to induce a convulsion in the brain similar to an epileptic seizure (70-150 volts for 0.1-1 seconds) • Now, there is rTMS (repetitive transcranial magnetic stimulation) 111 Psychosurgery Destroys part of the brain to make the patient calmer and freer of symptoms Pre-frontal lobotomy (a radical procedure that cuts off parts of the frontal lobes of the brain) 1950’s—used for Schizophrenia, depression, bipolar, OCD lobotomies would often sever the frontal lobes from the rest of the brain, either by boring a hole in the patient’s skull or by passing an electric needle through the edge of the eye socket and cauterizing the brain tissue. caused a great amount of damage to intellectual functioning, and the procedure is no longer used. 112 Eclecticism Using two or more systems of therapy 113 The Deinstitutionalized Person • Transferring the treatment of mental illness from inpatient institutions to community-based facilities that emphasize outpatient care • Revolving door • Homelessness 114