Student Outline
advertisement

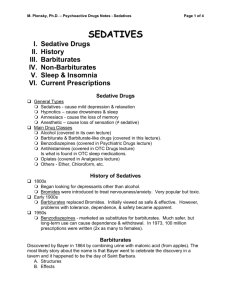
Chapter 5 • Barbiturates, General Anesthetics, and Antiepileptic Drugs Historical Background • Alcohol is oldest of sedative-hypnotic agents • Opium alkaloids (morphine) also used to induce stupor and sleep • In 1912, phenobarbital was the first of sedative drugs classified as barbiturates • Between 1912 and 1950, fifty barbiturates marketed commercially • Barbiturates are used to relieve stress, anxiety, and to induce sleep Sites and Mechanisms of Action • Barbiturates reduce electrical and metabolic activity of the brain • Accompanied by decreases in whole brain glucose metabolism • Reductions follow reduction in excitatory activity (glutamate) or augmentation in inhibitory activity (GABA) Sites of Action • Amnesic properties of sedative drugs result from glutamate antagonism • Sedative-hypnotic effect results from augmentation of GABA neurotransmission • Barbiturates bind to specific sites on GABAa receptor • Plays a major role in anesthetic properties of these agents Sites of action • Barbiturates bind to GABAa receptors and facilitate GABA binding • Barbiturates also capable of opening chloride channel in the absence of GABA • This accounts for increased toxicity of barbiturates when compared with lack of overdose toxicity of benzodiazepines • benzodiazepines do not open chloride ion channels independent of GABA availability Uses of Barbiturates • Barbiturate use has declined rapidly in recent years for several reasons: • They are lethal in overdose • They have a narrow therapeutic to toxic range • High potential for inducing tolerance, dependence, and abuse • Interact dangerously with other drugs (especially alcohol) Uses of Barbiturates • Despite the disadvantages, barbiturates are still useful • Used as anticonvulsants (for epilepsy) • Used as intravenous anesthetics • Used as death inducing agents ( main ingredient in suicide cocktails) Sedative Induced Brain Dysfunction • A mental status examination can be performed to diagnose drug induced dementia. It evaluates 12 areas of mental functioning • When sedatives are used, 5 of the 12 areas of the mental status examination are particularly altered. They are sensorium, affect, mental content, intellectual function, and insight and function (see table5.1) Pharmacokinetics • Barbiturates are classified by their pharmacokinetics • Short half-lives (thiopental has 3 minute redistribution half-life) • Longer half-lives (48 hour elimination halflife for pentobarbital) • Very long half lives (24-120 hour elimination half-life for phenobarbital) Pharmacokinetics • When taken orally, barbiturates rapidly and completely absorbed • Well distributed to most body tissues • Ultra short-acting barbiturates are very lipid soluble, cross blood brain barrier quickly, induce sleep in seconds • Longer acting barbiturates more water soluble. Sleep delayed for 20-30 minutes Screening for Barbiturates • Urinalysis is used to screen for the presence of barbiturates • Test will be positive for as short as 30 hours or as long as several weeks Pharmacological Effects • Barbiturates have low degree of selectivity and therapeutic index • Barbiturates are not analgesic; they cannot be relied upon to produce sedation or sleep in the presence of even moderate pain • Barbiturates suppresses REM sleep, and therefore dreaming Pharmacological Effects • Barbiturates are cognitive inhibitors • They depress memory function, cognitive function, motor skills, and judgment • Behavior may persist for hours or days until barbiturate is completely metabolized and eliminated • Overdoses or in combination with alcohol can result in death Pharmacological Effects • Barbiturate-alcohol combinations have been responsible for accidental and intentional suicides • Barbiturates in the liver stimulate synthesis of enzymes that metabolize barbiturates • This produces significant tolerance Adverse Reactions • Drowsiness is the primary effect produced by barbiturates • Impaired driving skills, judgment , and memory during period of intoxication • No specific antidotes • Treatment of overdose is aimed at supporting respiratory and cardiovascular system until drug is eliminated Tolerance and Dependence • Barbiturates induce tolerance by either of these mechanisms: • 1. Induction of drug metabolizing enzymes in the liver • 2. Adaptation of neurons in the brain to the presence of the drug • Withdraw from barbiturates results in hallucinations, restlessness, and disorientation Miscellaneous • Freely distributed to the fetus in a pregnant mother • Barbiturate exposure during pregnancy can have long term deleterious effects on the offspring • Some non-barbiturate sedatives such as methaqualone (quaalude) and meprobamate were used recreationally in the 1970’s-1990’s Miscellaneous • Chloral hydrate (Noctec) is a non-selective CNS depressant • Withdrawl from drug causes disrupted sleep and intense nightmares • Combination of chloral hydrate and alcohol can produce increased intoxication, stupor, and amnesia • This was called a Mickey Finn and is an example of an early form of date rape drug General Anesthetics • General anesthetics are potent CNS depressants that produce a loss of sensation accompanied by unconsciousness • One of two types: 1) those that are administered through inhalation through the lungs 2) those that are injected directly into the vein to produce unconsciousness Inhalation Anesthetics • Current ones are nitrous oxide gas • There are five volatile liquids: • Isoflurane, halothane, desflurane, enflurane, and sevoflurane • Vapors are administered by anesthesia machine • These produce a dose related depression of all CNS functions. Result in amnesia and unconsciousness Inhalation Anesthetics • Anesthetic action involves alteration of the physiochemical processes of nerve membranes • There is a linear relationship between potency and solubility in lipid • There is a potential for abuse for nitrous oxide (whippets) Injectable Anesthetics • Pentothal, Brevital, Diprovan, and Amidate are injectable anesthetics that are available • Mechanism of action of all these probably involves intense CNS depression produced secondary to facilitation of GABAa receptor activity and to depression of excitatory glutamate synaptic transmission Gamma hydroxybutyric acid • • • • • GHB is a potent CNS depressant Structure similar to GABA Freely crosses the blood-brain barrier GHB increases dopamine levels in the brain Widely implicated as a date rape drug Antiepileptic Drugs • Seizures are manifestations of electrical disturbances in the brain • Drugs suppress epileptic seizures in one of two mechanisms: • 1) limit the repetitive firing of neurons by blocking sodium ion channels, thereby blocking the depolarizing action of the ions • 2)Enhancing GABA mediated synaptic inhibition by reducing the metabolism of GABA, enhancing the influx of chloride ions, or facilitating GABA release from presynaptic nerve terminals Antiepileptic Drugs • Antiepileptic drugs are used in the treatment of bipolar disorder and a variety of explosive psychological disorders • These disorders can be treated with CNS depressants that stabilize neuronal membranes either by facilitating inhibition or by limiting excitation Structure and Activity • More recently introduced antiepileptic drugs were developed because they either resembled GABA structurally, or acted on GABA receptors to potentiate GABA neurotransmission • These drugs include valproic acid, gabapentin, lamotrigine, and felbamate • Barbiturates are used occasionally to reduce seizures. An example would be phenobarbital, the first effective antiepileptic drug New Antiepileptic Drugs • Several new drugs being evaluated are steroid derivatives referred to as epalons. • Epalons facilitate GABA activity. They are devoid of hormonal action • They exert anxiolytic, sedative, and anticonvulsant effects Antiepileptic Drugs in Pregnancy • Children of epileptic mothers who received antiseizure medication have an increased incidence of a variety of birth defects • Likelihood of birth defects increases from 2-3% for the general population to 7% when the mother takes antiepileptic drugs during pregnancy