Transcript - MyVeHU Campus
advertisement

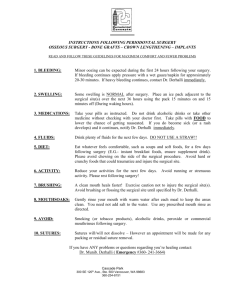
227 CPRS Orders for the Surgical Event Doug Rosendale Greg Strandberg Section 1: Overview Welcome everybody. I want to introduce you to the CPRS Order for Surgical Events talk. This is a very exciting part of my participation. I'm Doug Rosendale, a surgeon, and wannabe informatician and so I want to introduce somebody who I discovered was doing excellent work in Gainesville who now lives in Anchorage and that's Greg Strandberg. So he's actually going to take us on a flight and make this an exciting adventure about how they use CPRS in the surgical workflow. So Greg, why don't you come up and start this voyage and I'm going to interrupt him once in a while. First of all, his ability to create this project is, he lives it and breathes it and knows all the nuance and so although I was asked to participate with this, all I did is discover the excellence that he provides so I don't want to interrupt too much or it'll take away from the overall talk. So thank you for coming.This is going to be flight 227, it's a 200 level flight that we're going to be flying at, so there is more detail to be refined in the process, but we hope we'll give you a good enough overview that you can take away the gist of the flight details today. Dr. Rosendale is an outstanding surgical pilot and a great informaticist that's forward thinking in the VA and we're very lucky to have him at the level that he is trying to further and push the clinical needs that we have within the organization. What we're going to do today is ask you, like in all flights, to please reach down and fasten your seatbelts and this is to ensure you can't leave the presentation. And at any time during this presentation, if you hear an alarm sound because it becomes too boring, oxygen masks will be deployed. Please put these on your neighbor first. That way you can put you out of your misery and you may have a chance to actually expire before the presentation begins. So we're going to go ahead and get started here. We're going to go through the objectives. What we need to do is kind of go through why we have the key drivers and understand them for change. What we'd like to do is review the North Florida/South Georgia surgical implementation and we actually created an operating room as an ordering location so that we could automate the surgical process. The other thing we'd like to do is discuss the benefits and barriers, what problems that we ran into. And then review the planned policy change and Dr. Rosendale is going to talk about how the national folks are going to assist us in this endeavor." Section 2: Drivers for Change So the drivers for the change. Now this may not be too clear, but with any plane crash it always has you look to find those things that can make a real difference. 227 Patient safety, patient safety, patient safety was the primary driver for this change. The surgical event can be a turbulent time with the whirlwind of clinical activity that's all trying to coordinate about one point in time. Demands careful event planning and resources. We have electronic tools that assist the flight surgeon in evaluating the patient for surgery and doing the workup, but what about the actual flight, the trip to the OR and back. To us it's all known as the black hole where everything stops and it reverts to a manual process." So what's in our current flight instrumentation to help the pilots and crew during this flight? We have electronic ordering in the inpatient arena that does a good job of doing things like allergy checks and drug-to-drug interactions, but in the manual process, when we revert out of that into the surgical event, all of that utility gets lost." So that was our antiquated guidance system. We had a little radio out there saying well he's going to surgery, but that was about all that we're doing. The manual process of moving the patient to and from surgery is our order, it's our airplane's engine and that's what we use to document, drive and do care. And so that's what we were having failures with. Provider's hardcopy orders had to be interpreted and reviewed externally from our integrated medical record. We'd have to go search and find what happened about that surgical events. Providers didn't have the benefits of our electronic guidance systems that we normally have with order checks that can significantly improve patient safety. And it was an allergic event that spurred the evaluation of the North Florida process to develop a better way of doing things." We decided to look and see what we can do to make it better for the patient and worry about the administrative workload and the administrative actions that needed to happen. We had no order checks, we had the transcription and interpretation of data, and we had timing issues that we were facing. And the other issue that we came across was record continuity. And we all know the benefits of having the electronic medical record and having a contiguous record that's easily, readily readable. Greg, I meant to mention that your flaps weren't down at the proper time. That's why that plane crashed. The electronic paper copy of the record has a lot to be desired, we all know that, and we appreciate the benefits of the automation. 227 We mentioned the black hole of surgery, where all record stops and the continuity is lost, and that definitely leaves us a lot to be desired." And I'm going to let Dr. Rosendale talk about some of the standards and coordinations.I was the chief of surgery in Grand Junction for five years and so I got hit pretty hard by JCAHO issues and performance measure issues. And what we're identifying is that the documentation of clinical events in the surgery package weren't necessarily there that met these needs. And interestingly, the surgery package was not really designed to become a behavioral tool. It was mainly a documentation tool. Well, with performance measures out there and JCAHO requirements which are often a reflection of the performance measures..." ...we found that we had to modify the surgery package in order to document those details about clinical care. So one of the things that this particular solution provides is the ability to document and reflect the appropriate clinical care of the patient." So some of the new performance standards. We want to make sure that we complete the medication administration loop between what is ordered and what is administered. It's a task-oriented approach where we may have antibiotics ordered or not ordered, but often times patients get to the operating room and nobody's really sure if they've been given. And this is one of the areas where nationally I work on pay for performance with the private sector, and they are really grappling with: well what if the order is given but it's not delivered; and what if it's delivered and not ordered because it's held in a back shelf with anesthesia. And so, there's a complete discontinuity there and nobody knows how to deal with this. What we can do is, we can automate that process and we can build decision support solutions along that timeline of a patient's care with the solution that Greg is presenting. And then we want to be able to measure the performance by having that documentation in the Surgery Package or wherever it ends up in CPRS." So with all of these issues, it was clear it was time for a change." We started by removing our heads from the tailpipe. And we proceeded to look at the big picture and realized that we have the tools in order to do this, but it would require some administrative changes to support our true clinical needs and what was best for the patient." Section 3: G-OR / SDSU Order Menu / SDSU Admission Set So we developed a new ride." 227 And what we did was utilize the Surgical Day Stay Unit and created a Surgical Day Stay Unit in Gainesville, and it was called an Ambulatory Day Stay Unit in Lake City Division. And with that we created two new treating specialties. One was G-OR and L-ASU, both respective of the divisions. And what we did with that is linked it to the 23-hour observation. And we created administrative procedures in order to ensure that the PTF file remained clean and also that the G & L was reflected throughout this process; so it's quite elaborate procedures that MAS filed to ensure that. We designed in a process admission that lets us integrate not only inpatients and outpatients; everybody uses the same surgical pathway in order to get admitted to the hospital. So North Florida/South Georgia is affiliated medical school. We have residents and they do over 400 cases a month, so it's been done in a complex environment where they're able to do that. And then we created discharge procedures, again to follow-up on that method to make sure that we cleaned up the records and didn't impact billing negatively." In North Florida, there's kind of five primary pathways that they go through surgery in order to make it to the OR. In one, if a patient's planning to go to surgery to home, the other feeds surgery into acute care admission, surgery to 23-hour observation, nursing home care unit to surgery that's going to return back to the nursing home care unit, and then nursing home care unit to actual acute admission. So same five different pathways to get there, they're all integrated going into the same location. Now the nursing home process is handled just a little bit differently. There's only one thing that's changed with that, really, to the admission process and we'll kind of cover that as we go. The decision to go to surgery is made and the process begins by then writing delayed orders into the Surgery Package. Now we follow the standards of orders having to be written 30 days in advance to surgery to follow along the lines with all the other JCAHO compliance. There is ways that you can write the orders in advance and not activate those delayed orders until the actual surgical event is close and some of the services have coordinated that activity. They've kind of modified their procedures in order to do that. So we're going to take a look at the process and kind of see what this looks like. It's kind of a little bit cut off the screen there, but you can see the provider sat down and he clicked on the Delayed Orders and now you see the Admit to G-OR and it's highlighted in red down there. We created in a new admission dialog that has the resident's name, additional instructions, and then the actual OR date for the coordination of surgery. So anyone would be able to look into the actual CPRS delayed orders and figure out really readily what the planned scheduled date of surgery is." 227 And that's just a screen shot showing the OR prompt that's going to assist the folks in coordination." We're just going to run through some of the order menus that we had set up. These are not by any means the most comprehensive and best menus around, but it has served our needs -- and it's what our physicians ask us to do -- so it seems to be working out fairly well. We have an integrated menu that covers both the Recovery Room orders, discharge order sets and everything. They wanted it all integrated in one menu, one place to go to find it so it made it easier for us so we facilitated that, but we could have actually designed independent menus for that. This is just a Surgical Order. You see that we do have a Standing Admission Order sets and Recovery Room Order sets and we'll cover those a little bit, and then the individual break-out of the orders." So we're going to go through the Surgical Day Stay Admission Order set. We covered the allergy. That was the whole thing that tripped us up. When the manual process that is eliminated with the electronic process here -- the ability to enter the orders." We have allergies, then we have activity orders, vital signs, your standard medications, inpatient labs, radiology, consults, procedures, study, and then there's some blood counseling that they want to do at our site that they actually do with the patient that they anticipate needing blood. Section 4: Admission Notifications / Common Medications So this is an Admission Notification that we created and in the Admission Notification, it's a text order that fires off an Orderable Item that goes to the fifth floor Surgery so they coordinate knowing whether they're going to need a bed on the anticipated date of surgery with that so it helps coordination. It also can be used through the billing for advance notification to let them know that there is going to be a surgery scheduled for the folks." This is just some activity orders that we created for the surgical event." 227 Vital Signs, pretty straight forward. We have a more complex vital menu, but this is pretty much what they use around the perioperative and post-operative periods." Radiology orders. A lot of these are old hat but it's all integrated into the process." We have some common medications for the Surgical Day Stay Unit. We looked in Pharmacy and had Pharmacy pull us the list of the most common ones that they ordered for Surgery and those were the Surgical Day Stay Unit meds that we had listed here." Notice in highlight, it's Inpatient Medication package that's used. So it mirrors the dosing with it. And so that allows us to integrate BCMA. And so this year we actually are using Bar Code Medication Administration along with the surgical process to document the medication. Now we'll tell you that they were still having the Anesthesia do some of the final pre-op administration to help with the timing to meet the measure. It was thought at first if we could switch it over to BMCA it may help with that integration, but so far we still haven't got the timing down right. Anesthesia is the better choice for now. And actually, that model is being used nationally. They found that Anesthesia is actually taking on this responsibility of pre-op antibiotic delivery, if that's the one you're talking about. Yes.And they own it and they can get that antibiotic delivered within 60 minutes of the case. And so we let them have it. We just need a better way to document it. So BCMA may be a better way to do that. And you had talked about the national approach to integrate all of the packages. I think there's a work request for that, right? Anesthesia, Surgery and the Medication delivery is something you have in the works. Well, that particular proposal ended up evolving into your proposal as it turns out. When you document an antibiotic on a patient delivered in pre-op or in the OR -- whether it's documented by Anesthesia or Surgery or a nurse -- that it's all documented in the same location. Right now, is very disparate and that's part of the impetus for this proposal. But, effectively, the solution that you guys came up with in Gainesville is the one that we think we should model. And then adding BCMA as a solution within the OR without constraints is a solution to be sure that documentation occurs. The challenge will be to get Anesthesia to participate in a BCMA workflow. And they piloted that in Gainesville. They tried it in Louisiana, I believe. What has been the success with that so far in Gainesville -- BCMA use? In the BCMA for the nursing in the pre-op and recovery room environment, that's going fine. But the anesthesia is still under process with that. This is that example of an order check. I'm just hitting this again because patient safety was the driver for this change." 227 And this is what would have assisted with that patient that we had. And this is just an example of cefazolin we were trying to enter and caught in real time." Section 5: Order Comments / Procedures / Education We also, with the orders, have ability to echo comments, as you all know, into BCMA. So we can put the administrative comment field and the nurses see that, so we have here: Only to be given in Surgical Day Stay Unit.And also, because of the distinction that happens with this process, now we segregate the orders. We used to have pre-op orders. Used to go under active orders for the patient that's actually on the ward. And then, does the ward give it? Or does the on-call when he's down in Florida, do they give it or-- And so there was a lot of that back-and-forth figuring out what to do. Well when you actually write the Delayed Orders and it becomes a movement, then it takes the issue out of who's supposed to administer it. So we kind of switched that down to that.And I think that's really the driving-home point. The hook or the justification for this process is the fact that surgical patients, since CPRS is implemented, were not having the value of Order Checks, Allergy Drug, Drug-Drug Interaction Checks. They were just going off into the black hole, like you said, and they weren't having the value of those solutions. And so that's a real reason to actually implement this solution. And we'll talk about why this is not implemented more uniformly in just a few minutes -- and it has nothing to do with clinical care." So this is a Procedure menu, again following along the order set just to kind of let you see what were doing." The studies -- We just have a real brief menu that has some kind of standards that they wanted to do if the patient was 60 years old, or the creatinine or glucose elevated, that they get these specific labs." And this is just an example of any kind of education text order that could be followed up and now documented via nurse verification in the record." So the orders actually get entered and placed. And we're going to go ahead and sign these orders off..." ...and when we do, they become activated. And now in the top left-hand corner screen up there, you'll see that it says Delayed G-OR, so they're awaiting activation to the inpatient location." 227 So now we're back into the pre-operative process and we decide it comes the day of surgery. The ward administration staff is going to do the admission where they're going to put the patient in that treating specialty and into that ward location. All the orders will then print out in the pre-operative area." Section 6: Administrative Admission Process / Time Out of OR Talk a little bit about what the administrative process is. The PSAs or, the patient service assistants, receive the OR schedule of patients to be admitted. And they assist the surgical day stay staff in actually getting those patients admitted and they take care of the first several cases. What that does is it activates the orders in the computer system and allows pharmacy and surgical day staff to then see the orders and act on it. But the nice thing about the delayed order process is also that anybody can see the orders in advance of the surgical event, so it kind of lets them know what's coming up and who they have planned as well. So the orders get activated through the MAS actions. BCMA is there for doing the administration." We see here, G-DSU, so now there in inpatient location and they're admitted." The orders have been activated." And with this, now we see once Pharmacy finishes if it shows up in the BCMA and we can echo the comments that we're doing there for the one-time administration. Now we have it documented in CPRS, readily retrievable." So the patient moves to OR and actually goes to the interoperative period." And the Interoperative Orders are still paper-based. That's our next step is to try to integrate the Interoperative Orders. And we're still dealing with the logistics of how to do that in the electronic environment. But now we have the tools, since this is all automated, in order to do that." The Case Conclusion, or the "Time Out of OR," has a trigger under the Event Delayed package that was released. Actually it's called surgery in that event trigger and it triggers off the time this field was done." 227 This is just a little example for any CACs in the audience. One of the things that you'll notice is that both of them are set to "No." For over a year and a half we had it set to "Yes" where we used the time out of OR as the actual trigger, but we ran into some issues with that." And the issues that evolved with that is that the end of a surgical case is a very busy time for the patients. And nurses, physicians and anesthesiologists are running around trying to make sure the patient goes to the next care area as safely as possible, and so they're not focused on a "Time Out of OR" field at that particular time. Well we also have pathways where patients never go to the Recovery Room or OR, they get immediately transported to the Surgical ICUs. And so any delay in setting that "Time Out of OR" field could cause active good valid orders that have been released, like the Surgical Intensive Care Orders, to be discontinued or triggered. We actually had a couple events where they had full activated orders, because of delays, nursing come back after the patients had been settled and entered in, causing valid orders to be discontinued -- and that required re-writes. And you know, if things are bar coded in the ICU, then if those labels didn't match and it was a real nightmare. Doug has been instrumental in bringing aboard a change and I'll let him talk about that.Doug Rosendale: The point is that, what I'm trying to identify is a workflow issue, not necessarily a policy or a political issue. And that is that in the workflow in the operating room, the interoperative nurse actually fills in a field in the OR Package, the Surgery Package that triggers all these other events. And it's a trigger point called the time the patient is out of the OR. Sometimes they don't even fill that field out until the next day or sometimes days later. Now that doesn't happen much any more I can assure you, but there's now a lot of attention to make sure that's done at the time the patient actually does leave the OR. Well that didn't work for the Gainesville solution. The time out of the OR was too hustle bustle and complex. And so the notion was to create a "Time in OR" as the trigger point for the change to occur. And so what we've done is to put forward a new service request. And that actually is going to be started on by the program officer, surgery package office, shortly. In fact, they may have already started. So that change will occur and that will help us. It was an archaic point when the development of the Surgery Package occurred because they just said, well at the end of the case that's when you finish and that would be your trigger point; not realizing that the episode of care between pre-op holding then the OR and then post-op required some lag time between, like, the time of the case where the interoperative nurse could do diligence. So the "Time in OR" has now become the change or trigger point. Does that make sense to everybody? So I think that's a real valuable change that will help the solution. " And with this process and the changes that occurred, it actually compartmentalized each one of the events. So now we have an admission or transfer orders that we get to see. We have the surgery parameter, currently Time Out of OR, changed to "Time in OR." That groups the pre-op and interoperative orders. And then we have those orders being discontinued by an auto event. Then we have the Recovery Room orders that we're able to see as an event trigger. And then we either have a 227 transfer to the ward or discharge. So it's very easy then to go back and to look at those individual orders that were activated and done at that particular event, kind of track the patient through surgery electronically ...and so that's where we're at right now. We're actually at the Recovery Room or PACU for the patients that are going that pathway. And the patients that are actually going to be admitted, the recovery Anesthesiologist usually writes the Recovery Room orders at our facility and the physicians write the delayed orders to the ward concurrently. And there was that battle between physicians and Anesthesia, who was going to grab it first for writing the orders.They're just transferred. It's still all in that same location. And what we're using to segregate those events is that event trigger -- that Time Out of OR, Time in OR -- so it wipes the slate clean for the Recovery Room PACU orders at that time after they're moved out, so they have a blank ordering screen in order to make sure they're just dealing with those orders and nothing pre-operatively." Section 7: PACU Orders / Nursing Home / Auto/DC Release Events / Barriers & Cons PACU Recovery Orders -- and we're just going to go through like we did in the others through the actual order sets." We see that we have the standing orders, that they ask for the Anesthesiologist and some common medications, again we went to Pharmacy, what was the most frequently being ordered, and this is what we got for the list, any labs and common radiology they'd like to follow-up with." This is just an example of a PACU Standing Order Set that we had developed with the orders." We do the IV fluids, of course, and start PCAs in the PACU too." Then the decision is made whether the patient is going to be home or discharged; if he's going to be transferred to the ward." The delayed orders are entered in and it's like any other transfer to any location that happens. If he's going to be discharged..." 227 …now MEA goes through the procedures to discharge the patient to home and then actually deletes the admission to do a clean up." One of the things we talked about before was the nursing home patients that go through this process. The procedures vary a little bit for the nursing home because if the patients were leaving out of the nursing home from an acute care setting, it was actually re-triggering events that the physicians would have to do, like, the admission H&P again, back to the nursing home. And you know, we two-hour little trip through the OR and back again shouldn't require all that. What we did was create a GNHOR location for the nursing home. The orders still print and go to the same printer in the Surgical Day Stay Unit there, but it keeps the nursing home patients in that ward location so that they don't have to go through those administrative requirements unnecessarily, so, because the patient is still returning to the nursing home. We use the same treating specialty. In North Florida/South Georgia all of our event triggers are all based on treating specialty. We don't have anything based on ward location. So if your general surgeon puts you on the third floor or general surgeon puts you on the fifth floor or even if you're in the nursing home, it's still the same treating specialty that does the trigger. So we don't loose any orders that way by the location movement." We talked a little bit about the Medical Administration Service. And the MAS ADPAC was instrumental in developing a set of guidelines. And we have the documents. We can put this up on a resource. A kind of a step-by-step that tells them where they're going, what event, and exactly how they need to do it in the package in order to ensure that they're going to have an accurate G&L and that we don't negatively impact billing resources in there. So it ensures that we have an accurate patient treatment file, we're not creating something in there that shouldn't be, and also that the G&L is maintained accurately." Through that process we have the midnight, the full moon where evil happens in the MAS Process.(Werewolf howl) So what we have to do with this process is ensure that the patients are out of that location. Most the patients are through surgery at that time and -- and removed from that location before midnight. And we'll talk a little bit about what happens if somebody needs to stay over. But for the most part what happens is, we have set up a routine that automatically e-mails the MAA on duty at 8 p.m. and 10 p.m. and lets them know if there's any active patients in that ward location. So they look to just make sure that it's not just an administrative oversight that somebody forgot to take a patient and actually discharge. Sometimes it happens -- it's a late case and the actual clerk that's in that area has left. So the MAAs are the back-up for that to pick up to make sure that's done. If a patient had to stay over, it's a real late case that goes through, there's always a way to administratively clean that up through the MAA. And they do that on the midnight shift. When they're ensuring that the G&L is correct, they go through the procedures to find out if it was a surgery patient. Oh he shouldn't have been there; he was just through the part of the OR; and they do the administrative clean-up. So there's 227 a couple checks and balances along the way to make sure that it's accurate. If the patient needs to remain at midnight, there's MAA, telling them they have to be discharged or calling them. With this process, we're obviously about patient safety. And this is the whole point with this. It's just one of those things that we had to overcome as part of this process. " With the events we had talked about doing in CPRS, you may or may not be aware, there's an Auto DC/Release Event view and that shows you things that happened on those release events." And this is kind of a little blow up of that menu And you see here for this surgical patient that we did, we have the admit to G-OR and the "Discharge-G" is for discharge, the Gainesville division. And in that, you see that the patient event shows up in the little red diagram box that's up there, and you see that these were the orders that were acted on for that particular admission." A little bit about the pharmacy process -- There was a Pharmacist that's assigned to the pre-operative area so they look at those orders, the Surgical Day Stay Unit orders, and act on those to try to get all the timing, the antibiotics, make sure everything is done. Now it's electronic so they're not going down trying to gather paper, written orders for that process. They poll the Surgical Day Stay Unit and Lake City Surgical Day Stay Unit locations. And with the prep part that the MAA works with the Surgical Day Stay Unit in order to admit the patients a little bit early and in advance of the event, it actually buys pharmacy a little more time to prep the orders and get them done.We're also, part of this process, trying to develop a routine and assist Pharmacy better in the preparation of medications. And what we're proposing that that does is it looks to the OR schedule for the day and actually looks in the delayed orders and pulls out the medications that the patient would be activated in the delayed status. So that way if they're making up antibiotics, although they couldn't finish the order, they can do some of the prep work in advance to get those set up. And then when the patient is actually admitted they have the IVs already finished or the antibiotics already finished for that part." The revenue impacts inpatient processing with this are handled in pretty much the same way. So it doesn't really impact anything, any of the procedures for inpatient. It's just the timing issues that they adjust within the admission. And from what Medical Administration Service says, there were no changes there. 227 As we delete the PTF file, it doesn't impact any of the outpatient procedures. Outpatients are still handled. There's a clinic that they're scheduled to. The coders review and process, they look for additional fees, they create the appointments, and they review the surgical diagnosis and the operative reports as part of that process. So we've made sure that this didn't negatively impact that as well CPRS configuration, there's just a couple of points. Orders are controlled by treating specialty changes which we've already mentioned. Release events excludes microbiology and pathology orders. As we were doing this for the OR movement throughout there, we found that they ordered a pathology report or micro report and the order would get cancelled. When we would go from one location like Surgery, it would, "Time Out of OR" would trigger and kill it. So we've just excluded those orders so they just always remain active in the status and we don't have to worry about that. We created the admission order with the OR date and also that notification, generic text order, and we developed some specific surgery and anesthesia menus." Barriers. It requires strict adherence to procedures. We really want to make sure that the administrative process done correctly and wasn't impacting billing. So MAAs and the PSA clerks really have to have the training and follow those guidelines. And they've developed, pretty straight forward, this is what you do so once they learn those it's a pretty easy process.Surgical cancellations are our biggest still bone of contention. Since we're doing delayed orders, and they're admitting the patients, if the patient actually has the surgery cancelled, those delayed orders that have been activated have to be rewritten if it's going to be postponed to another day. And there is no automated way to say whoops, he didn't have surgery today, restore those orders. So, that's an impact that we have.Surgical processes have to be modified. You know a lot of times paper-based process allow a little bit of latitude and change. And with this, there has to be a process for making sure the orders are signed-off within 30 days in advance. It's a process for the surgeons to learn this, but most of the time it's like they order any other way in the hospital other than surgery. And they were pretty happy to have a way that they do everything the same instead of having the paper-based process to try to deal with afterwards. So the surgeons at North Florida/South Georgia was pretty pretty receptive. Anesthesiology is having to enter orders. They're now having to enter Recovery Room PACU orders, and so that was a little bit of a change and process change for something new for them to learn. " Section 8: Thanks to NFSG Team Greg Strandberg: Last slide here is, we'd like to definitely thank -- it was a great team at North Florida, I just have the opportunity today to represent the hard work of a lot of different people involved in it. And especially Dr. Good was our chief of staff at the time and had the foresight to really say: Hey, this is in the best interest of patients so we're going to push that envelope to do what we can do to do it. And my former boss, Ruth Gorman, was instrumental in making this happen.Doug Rosendale: Yeah, I want to thank Greg. That was just phenomenal. And I want to make a couple points, going back a little 227 bit, about to that MAA issue. Effectively, there was a rate limiting step, in this case it was an adoption limiting step because, essentially, we were being held hostage by a coding/billing requirement so that we did not impact the G&L. And there was a memorandum that came out, some of you may have received it, that said we were not allowed to admit patients to this status and then discharge them from this status because that was a so-called pseudo-admission. Well we did a lot of diligence to try to organize that so that we could be allowed to accomplish this solution in the name of patient safety. Order Checks, Drug Allergy, Drug-Drug Checks, and workflow documentation. And it's been very successful. So this Chief of Staff I hold my hat off to because he really made a decision to allow for this sort of a process. Now, there is not a formal memorandum that has rescinded the prior memorandum but they are allowing us to do this as long as we do diligence to make sure that those admissions are terminated at midnight. I've discussed this with the HIMS folks and I really think the next step is to start to really reflect what status a patient's in and have the coding/billing actually identify and understand what that is. So that policy issue needs to be changed and that functionality for coding/billing needs to be changed. And then the other point I wanted to make, we have an internist in the crowd, and surgeons and internists are always fighting. Well not any more. We are a team effort and whether a patient goes to a medical floor or a surgical floor is not relevant. They go to a hospital team point where they get the maximum care for all providers. And that's what it takes for all this. For pharmacy, for the CACs, for the clerks, for the surgeons, everybody to collaborate and work together. And I think that this solution is going to be the way that we actually maximize on the use of CPRS. I wanted to invite Ben Davoren and get another view. There are other people, other facilities around the country that are starting to adapt this solution. And I thought I would ask him for a couple of minutes at least, before we take other questions, to see if he could give us his perspective. Ben Davoren: Thanks Doug. I'm Ben Davoren. I'm an oncologist so I'm an internist as well, and working at the San Francisco VA as the director of clinical informatics. And you know we struggle, I'm sure all of you do too, with the same issues you have here. Some of the solutions you have are human solutions, which I think we've all discovered the issues of the timely admission or transfer action in VistA to try and parallel the physical movement of the patient. When those things don't match, those have been our biggest problem. We have had a long history of having patients who are going to be admitted after their surgical procedure being admitted in VistA at 5 a.m. Now there's not a human there doing that. The events that have happened physically in time have been done later in the day when the clerks have been able to actually perform the VistA action. And what that does of course is discontinue any admission orders that were written at 9 a.m. in perfect advance of the patient really being admitted physically. And then they went back in time and suddenly those don't exist anymore because they should have been transfer orders. But of course you couldn't have written them at that time. So the clerical steps here are really critical. And so I think you've done a great job in separating the issue -- the treating specialty is the only way we can make this work for us as well -- but in separating the responsibilities for pharmacy, nursing, and clerks in the movement to the OR. I am curious, actually as to, one problem that we've identified as we're doing something that's very similar is still making sure that patients who are on the ward or who are in the hospital the night before get their pre-op medications before they go to surgery in terms of divvying up the workflow -- for beta blockers in particular. If somebody comes the night before and they don't bring their medications with them, they miss their 5 p.m. dose of beta-blocker because the orders are written after the time when they would normally take their dose or it's due in BCMA. But the 227 following morning when it would be due in BCMA, for us an administration time of 9 a.m. but the patient is whisked off to the OR at 7. And the transfer of responsibility, just like for the pre-op antibiotics, for the pre-op medications is tough. I'm curious how that works for you. Before you answer, the issue for us is similar for the "time in" versus "time out" of OR, and so I think we made that change internally to our software about eight years ago when we realized that time out of OR was exactly as you described: it's no time to be worrying about whether or not you're running over to the terminal or the keyboard. Time in OR is much more controlled.Doug Rosendale: Thanks Ben. Greg can answer this too, but the way we have been able to look at some of these process issues and being sure, double checking that patients are getting things done -- like the antibiotic delivery or the beta blocker or the time out -- is we've modified the Surgery Package to actually capture that information. And we go through what's called a pre-op huddle. Now that's not being done at all facilities. It's actually being initiated by Patient Safety. It's being done in a few places like Boston and Houston. The idea is that if a patient has an indication for a pre-operative beta blocker, that we ask that question. Now the solutions to actually identify if that's been delivered through BMCA and the clinical decision support that would flag us about whether or not it was ordered or delivered have not been developed. But at least at a checklist point in the pre-op area, we will be able to ask the question. And then if they haven't received it, then we ought to be giving it to help with our patient care. Do you have an answer about how you actually manage medications that are ordered on the ward before the patient gets whisked off to surgery?Greg Strendberg: What they've consolidated in North Florida-- We had it where that we tried to order some pre-ops under active medications on the ward and then others that we would do under the delayed status. And over time it's kind of evolved for the pre-op, taking on all the medication administration responsibility. So if it's needed for the surgical event, they write it into the delayed status for the order. And then when the orders get activated, they actually have the order for administration. Doug Rosendale: Right, so it goes to the same responsibility shifting that anesthesiologists have so nicely taken on. Not that they want to do it electronically, they're just very good to pull the bag out of the refrigerator and give it. But as far as documentation of that, we need an easier way for them to do so. On that note -- then I'll take questions -- there is probably, hopefully, going to be lift of the moratorium to order anesthesia record keepers. And that would allow us to at least document delivery of antibiotic in a third party software solution. My goal, and one of the projects you mentioned earlier, is that though it's documented in a third class COTS application, we want that to report back to our Electronic Medical Record. Right now that's reported in a PDF, non computable form, and that's not adequate. So there's a lot of work to do but we're working on it.