Critical care medicine: The essentials
advertisement
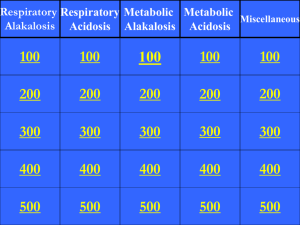
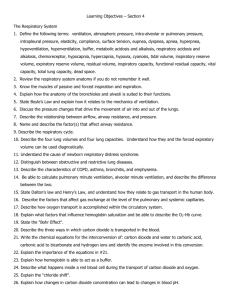
Medical Case Studies ACNP Boot Camp 2013 Case Study #1 Mr. Allen is a 62 y/o male, PMH HTN and DM2, admitted to MICU with hypoxia related to newly diagnosed community acquired pneumonia. He was given azithromycin by his PCP 2 days ago, however this morning awoke short of breath and feeling worse. He has an allergy to sulfa drugs. In the ED, SpO2 was 89% on RA. Vitals on arrival to MICU: HR 115, BP 101/58, RR 38, SpO2 92% on 50% venti-mask. His CXR is as follows: ABG on admission: 7.49 / 25 / 65 / 24 Na 138, K 4.2, Cl 102, C02 24, BUN 12 , Cr 0.8 , AG 12 What is the acid-base disturbance? A. Mixed metabolic acidosis and respiratory alkalosis B. Respiratory alkalosis with compensation C. Respiratory alkalosis without compensation D. Respiratory acidosis What antibiotic changes should be made? A. Discontinue Azithro then start Vancomycin and Zosyn B. Add Bactrim to regimen C. Start Clindamycin and discontinue Azithro D. None of the above After 24 hours of antibiotics and bipap, Mr. Allen worsens and requires intubation. Repeat CXR : ABG prior to intubation 7.2 / 50 / 53 / 20 Na 136, K 4.5, Cl 100, C02 21, BUN _ , Cr _ , AG 15 Lactate 3.9 What is the acid-base disturbance? A. Metabolic acidosis B. Respiratory acidosis C. Respiratory acidosis with metabolic acidosis D. None of the above With a pH of 7.2, what can you do to correct the acidosis? A. Increase minute ventilation (RR up to 35) B. Start a paralytic infusion C. Give crystalloid fluids D. Do nothing He now has ARDS and is now requiring 70% FiO2. For maximizing alveolar recruitment, what should his PEEP setting be? A. B. C. D. 5 mmHg 18 mmHg 22 mmHg 12 mmHg Mr. Allen is 73 inches in height and weighs 105kg. Calculate his set tidal volume (predicted body weight x 6) A. B. C. D. 480 ml 340 ml 920 ml 220 ml After 3 days of supportive care, Mr. Allen continues to decompensate and a bronchoscopy is performed. Preliminary results reveal a gram positive organism. What changes should be made to the antibiotic regimen? A. Discontinue vancomycin and start linezolid B. Discontinue vancomycin and start daptomycin C. Add coverage for atypical organisms D. Both A and C Unfortunately, the next day, Mr. Allen starts having melena stools. His PCV has been downtrending from 3833 27. After further review of his medication list, he was never started on stress ulcer prevention. Which is the best treatment option? A. B. C. D. IV H2 Blocker PO H2 Blocker High dose IV PPI PO PPI Aggressive red blood cell transfusion would be the next best course of action. A. True B. False Mr. Allen’s condition is improving. Which factor is not required to start vent weaning: A. Make unassisted breathing efforts B. No pressors required C. FiO2 <.40 and PEEP <8 D. Awake and following all commands Questions? Case Study #2 Mr. Commodore is a 43 yo M with a hx of alcoholic cirrhosis and CAD on daily ASA who presents to the MICU with c/o melena, fatigue, and weakness. Pertinent labs on admission include WBC 15, PCV 26, and platelets 100K. His initial VS are: BP 120/80, HR 110, RR 18, afebrile. Physical exam is negative except for abdominal distention with positive fluid wave. What would you do next? A.Begin Pepcid 20 mg IVP BID B.Transfuse 1 unit of PRBC C.Begin esomeprazole 40 mg IVP BID D.Prep for colonoscopy You should begin an octreotide drip at 50 mcg/hr after a 50 mcg bolus dose. A. True B. False SBP prophylaxis should be initiated. A. True B. False Which antibiotic would you start for SBP prophylaxis? A. B. C. D. Vancomycin Ceftriaxone Metronidazole Caspofungin Within 1 hour of arrival, the patient develops large volume hematemesis and becomes hemodynamically unstable. His vital signs are as follows: HR 135, BP 80/44, RR 26, O2 sat 89% on 2L NC. Which of the following is the most important next step: A. Intubate the patient and obtain 2 large bore PIVs B. Insert CVC and begin levophed drip C. Order STAT PT/INR D. Consult EGS Once the patient is intubated and the airway is stabilized, you consult the GI team STAT for endoscopy and intervention. While waiting for the team to arrive, how can you optimize the patient for endoscopy and attempt to stabilize him? A. Transfuse 1 pack of platelets B. Give 10 mg Reglan IVP now C. Transfuse 1 unit of PRBC D. All of the above The patient undergoes endoscopy and is noted to have large esophageal varices. Five bands are placed and hemostasis is achieved. Incidentally, the patient is noted to also have esophageal candidiasis. Which antibiotic should be initiated in this patient? A. Fluconazole B. Micafungin C. Amphotericin B D. None of the above; pt is asymptomatic The patient remains in the MICU overnight for close observation. He remains hemodynamically stable and has no further bleeding. However, this morning’s labs reveal a PCV of 20 and platelet count of 92K. Which of the following is the next best course of action? A. Nothing. The patient is stable without evidence of recurrent bleeding. B. Transfuse 1 unit of PRBC C. Discharge the patient home D. Transfuse FFP Questions? Case Study #3 Mr. Smith is a 67 yo male who resides in a SNF, with a history of CVA, COPD on 2L 02 who was treated 6 weeks ago for CAP. He is admitted to the MICU with SOB, AMS, and a 5 day history of diarrhea. VS: BP 88/52, HR 116, RR 22, 02 sat 92% on 6L 02 ABG: 7.22 / 30 / 65 / 10 What acid base disturbance is present? A. Metabolic acidosis B. Acute Respiratory acidosis C. Chronic Respiratory acidosis D. Respiratory alkalosis Winter’s formula 1.5 x 10 + 8 = 23 What does this tell us? A. Respiratory compensation is incomplete B. Pt. has a secondary respiratory acidosis C. Both 1 and 2 D. Neither 1 or 2 Delta / Delta ratio is 7/14 This indicates the following: A. There is an additional non-gap metabolic acidosis B. There is an additional metabolic alkalosis C. Neither of the above D. Not sure Mr. Smith’s diarrhea becomes severe and he tests positive for clostridium difficile. What is the best antibiotic treatment for this patient? A. B. C. D. Metronidazole PO Vancomycin IV Fluconazole IV Vancomycin PO Questions? Case Study #4 55 y/o male presented to ED with 3 day hx of malaise, fever, and poor PO intake. PMH significant for HTN, DM, and ESRD s/p renal transplant March 2013. Admitted to MICU for septic shock. Admission labs showed WBC 0.4, creatinine 5.0, increased from baseline of 1.8, and lactate 6. Patient received 1500mg IV Vancomycin, Zosyn, and 2L IVF in the emergency department. When should the Vancomycin level be checked and what type of level should it be (peak, trough, random)? A. Trough level 30 min before 5th dose B. Peak level 12 hours after initial dose C. Peak level after the 5th dose D. Random level 12-24 hours after the initial dose Patient arrived in MICU hypotensive. An additional 3L IVF given with no improvement and vasopressors started. Patient rapidly became hypoxic (SpO2 in the 70’s) and required intubation. Vent settings: Volume control, 100% FiO2, 12 PEEP, rate 15. Fentanyl drip started. Patient remains hypoxic on the current vent settings. Peak pressure is 23. This patient’s peak pressure is within acceptable range. A. True B. False ABG: pH 7.22 / 30 / 65 / 10 Na 136, Cl 102, C02 10 What is the acid-base disturbance? A. Respiratory acidosis B. Non-anion gap metabolic acidosis C. Anion gap metabolic acidosis D. Compensated metabolic acidosis What are the next steps to improve oxygenation? A. B. C. D. Paralyze the patient Increase PEEP Prone positioning Inhaled Flolan Hospital day #2: Patient without improvement. Remains ventilated and on vasopressors. Creatinine up to 5.5 and WBC holding at 0.4. Current antibiotics include Vancomycin, Zosyn, and Levaquin. Blood cultures pending. Urine culture pending. What additional organisms should be considered as a source of infection? A. B. C. D. MRSA ESBLs Candida Candida and ESBLs Which is the best antibiotic to treat an ESBL in this patient? A. B. C. D. Zosyn Aztreonam Clindamycin Meropenem Which antibiotic would best treat Candida in this patient? A. Fluconazole B. Caspofungin C. Fluconazole and Caspofungin D. None of the above Patient’s shock is resolved and he is no longer requiring pressors. What should your next action be? A. Continue fluid infusions B. Daily CPAP breathing trials C. Attempt diuresis D. Both B and C Questions? References Acute Respiratory Distress Syndrome Network: Ventilation with Tidal Volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. New Engl J Med. 2000; 342: 1302-1308. ARDSNet: Higher versus lower Positive End-Expiratory Pressures in patients with the acute respiratory distress syndrome. New Engl J Med. 2004; 351: 327-336. CDC website Garcia-Pagan et al, NEJM 2010; 362:2370-9 Halperin, Mitchell L., Kamel, Kamel S. and Goldstein, Marc B. (2010) Fluid, Electrolyte and AcidBase Physiology: A Problem Based Approach, Fourth Edition. Philadelphia, PA. Saunders Elsevier. Infectious Disease Society of America website Lau JY, Sung JJ, Lee KKC, et al, NEJM 2000; 343: 310–316 Marini, J.J., Wheeler, A.W. (2010). Critical care medicine: The essentials (4th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Rivkins, K., Lyakhovetskiy, A AJHP 2005; 62: 1164-1165 Sucher, A.J., Chahine, E.B., Balcer, H.E. Echinocandins: The Newest Class of Antifungals. The Annals of Pharmacotherapy. 2009, (43), pp. 1647 - 1657. Villaneuva, C et al NEJM 2013; 368:11-21