Powerpoint
advertisement

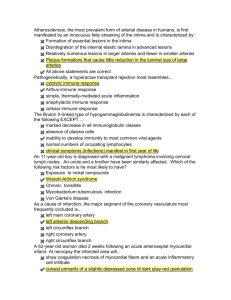
Immunopathogenesis of AIDS, an historical perspective: Or 30 years in 15 minutes Michael M. Lederman, MD Dec 10, 1981 Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency MS Gottlieb, R Schroff, HM Schanker, JD Weisman, PT Fan, RA Wolf, and A Saxon An outbreak of community-acquired Pneumocystis carinii pneumonia: initial manifestation of cellular immune dysfunction H Masur, MA Michelis, JB Greene, I Onorato, RA Stouwe, RS Holzman, G Wormser, L Brettman, M Lange, HW Murray, and S Cunningham-Rundles Barre-Sinoussi et al, Science 1983 Popovic et al Science,1984 Levy et al Science, 1984 The lymph node in HIV infection is inflammatory and enriched with effector T cells Tenner Racz ‘93 Cheynier ’94 Pantaleo ‘94 Altfeld ‘02 Brenchley ‘04 Biancotto ‘07 Lymph Node Naïve T cells Central memory cells antigen antigen Effector cells See Wednesday LB: JC Mudd Homeostatic proliferation Peripheral tissues Increased fibrosis in the HIV+lymph node Predicts failure of CD4 T cell restoration on HAART Schacker AIDS ‘05 Impairs intercellular communication Zeng et al, JCI ‘11 Estes, Schacker and Haase CD4 T cell homeostasis is broadly impaired in HIV infection Lymph Node Naïve T cells Central memory cell antigen antigen Thymus Effector cell Bone Marrow Homeostatic proliferation (IL-7 dependent) Periphery Dec 10, 1981 Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency MS Gottlieb, R Schroff, HM Schanker, JD Weisman, PT Fan, RA Wolf, and A Saxon An outbreak of community-acquired Pneumocystis carinii pneumonia: initial manifestation of cellular immune dysfunction H Masur, MA Michelis, JB Greene, I Onorato, RA Stouwe, RS Holzman, G Wormser, L Brettman, M Lange, HW Murray, and S Cunningham-Rundles T10 = CD38 Immune activation predicts HIV disease progression Janice Giorgi • Immune activation predicts HIV disease progression – CD38 – a better predictor of disease progression than VL. (Liu JAIDS ’98, Giorgi JID ’99, Deeks ’04, Wilson ‘04) High turnover of both CD4 and CD8 T cells in HIV infection is attenuated by antiviral therapy Kovacs et al J Exp Med ‘01 So if immune activation drives HIV pathogenesis (CD4 depletion),what drives immune activation? • A homeostatic response to cytopenia? (Srinivasula et al ‘11) • HIV itself? – Via antigen specific T cell activation and expansion? – Via products such as envelope that bind and activate cellular coreceptors? (Herbeuval et al ‘05) – Via viral elements that activate innate immune receptors? (Heil et al ‘04, Fontaneau et al ’04, Meier et al ‘07) • An immune deficient environment that permits replication of other microbes (eg CMV, other herpesviruses, HCV) (Lisco et al ‘09, Hunt et al ’11) HIV infection rapidly depletes gut effector memory CD4 T cells HIV- Veazey ’98; Guadalupe ’03; Mehandru ‘04 Matapallil ‘05 HIV+ Brenchley et al JEM 2004 Plasma LPS levels are increased in chronic HIV infection Brenchley et al, Nat Med 06 CD4 T cell increase at 48 weeks Levels of microbial products correlate inversely with magnitude of CD4 T cell restoration on HAART 800 R² = 0.2516 700 600 500 400 300 200 100 0 0 50 100 150 Plasma 16s DNA levels copies/ul Jiang et al J Inf Dis ‘09 200 Brenchley et al Nat Med ‘06 HIV disease is characterized by heightened inflammation and coagulation • The environment in both blood and lymph nodes is inflammatory (Pantaleo ‘94, Andersson ‘00, Biancotto ‘07, Kalayjian ‘10) • Indices of inflammation (IL-6, CRP) and coagulation (ddimers) predict all cause mortality (Kuller ‘08) • Activated CD4 T cells show signatures of high level type 1 interferon exposure (Sedhagat ‘08) And Immune Cells show signs of exhaustion and senescence • Increased expression of CD57, PD-1, shortened telomeres (Vanham ‘90; Effros ’96; Trautmann ‘06, Day ‘06; Petrovas ‘06) A model of immune activation and pathogenesis in the HIV+ lymph node E CM CM CM E E M APC Naive Naive E APC E E E Naive CM Naive APC E CM CM E CM Even after > 5 yrs of HAART and current VL BLD, ~20% of adult pts have CD4 T cell counts below 2, 740 350 the defined normal range Normal (95%) range 15% Valid N Median Percentile 25 Percentile 75 Percentile 2.5 Percentile 97.5 Minimum Maximum Perc ent 10% >5 years 340 609 412 802 122.525 1417.88 48 1822 5% 0% 100 200 300 400 500 600 700 800 900 1000 1100 1200 1300 1400 1500 1600 1700 1800 CD4 Rodriguez, Myerson Despite “complete” virologic control on ARVs, immune failure patients have increased T cell activation – – – – – – – – – – Teixiera AIDS ’01: age and low thymic output Anthony JAIDS ’03: immune activation and turnover Benveniste JID ‘05: Low thymic output Fernandez Clin Imm ‘06: immune activation and senescence Gandhi JAIDS ‘06: women restore better Hunt JID ‘08 Immune activation and microbial translocation Marchetti AIDS ‘08: immune activation and microbial translocation Rajasuriar JID ‘10: Linkage to IL-7Ra haplotype Sandler et al JID (in press) immune activation and microbia Gazzola CID ‘09: Excellent review of immune failure Fernandez ’06; Hunt ‘08; Marchetti ‘08; Sandler ’11; Lederman ‘11 Though both CD4 and CD8 T cells are activated in Immune Failure, cell cycling is increased only among CD4 T cells _____P<0.001_____________ __P<0.001___ Increased inflammation, coagulation and evidence of monocyte activation in immune failure despite virologic control ____p < 0.09_____ What we know • HIV is the cause of AIDS • HIV linked to immune activation; plausible drivers of activation identified • Immune activation is linked to disease course • Inflammatory cytokine levels are increased What we don’t know • Exactly how HIV causes AIDS • Which “drivers” are most important in which setting • Causality likely; proof lacking • Which cytokines mediate pathogenesis; which are just markers of infection? • Will blocking these pathways block activation? • Will blocking these pathways alter disease course? • To what degree and at what point are these pathways reversible? Immune Failure despite virologic control What we know What we don’t know • Increased T cell activation; increased CD4 T cell cycling • How much T cell activation is “push” and how much is “pull”? – And among plausible “pushers” which pathways are most important? • Increased coagulation and inflammation • What is the link between T cell activation and inflammation/coagulation • The degree to which “drivers” and mediators of morbidity in immune failure are linked to the drivers of pathogenesis in untreated HIV infection? A Way Forward • Interventional Trials targeting key pathways of “activation” can concurrently test hypotheses of pathogenesis and also explore promising treatment strategies for persons at risk for morbidity Thanks to: CWRU: Scott Sieg Benigno Rodriguez JC Mudd Nick Funderburg Brian Clagett Len Calabrese Carey Shive Wei Jiang VGTI: Rafick Sekaly Elias Haddad Nicolas Chomont Lydie Trautmann Rush: Alan Landay NIH Jason Brenchley Danny Douek Netanya Sandler Mary Carrington Leonid Margolis Irini Sereti Jake Estes Emory Guido Silvestri Mirko Paiardini Drexel Jeffrey Jacobson U. Minnesota Tim Schacker UCSF: Steven Deeks Peter Hunt Hiroyu Hatano U. Penn Mike Betts U. Paris Yves Levy