ACA: Overview of Impacts on Mediacid
advertisement

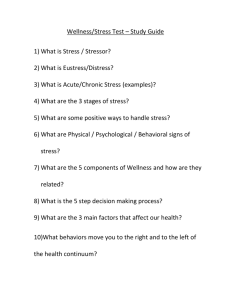
Affordable Care Act: Overview of Impacts on Medicaid Marni Bussell SIM Project Director, DHS Lindsay Buechel Communications Manager, IME Introduction • The Patient Protection and Affordable Care Act (ACA), also known as “Health Care Reform”, was signed into law on March 23, 2010. o The law is complex and requires a significant amount of time and effort to plan and implement during the last 2 and coming year(s). • There continues to be strong public policy debate on the law o o Supreme Court Decision Strong efforts to repeal or change the law in Congress. 2 Affordable Care Act (ACA) • Key provisions take effect January 1, 2014 o o Creation of Health Benefits Exchange/Health Insurance Marketplace Exchange is a “marketplace” to allow consumers to compare plan benefits and price, provide consumer assistance, facilitate plan enrollment. Mandate for individuals to have insurance coverage; penalties for large employers who don’t offer insurance Option for Medicaid expansion to 133% of the Federal Poverty Level (FPL) 2013 133% FPL: Household of 1: $15,282 Household of 4: $31,322 • Other provisions with various implementation dates o Mandatory Iowa Medicaid Enterprise (IME) operational changes to ensure ACA compliance o Optional opportunities to improve or re-balance health care programs 3 State Innovation Model Grant 4 The problem Chronic disease drives costs Chronic Care Within Medicaid 100% 23% 80% 60% 29% 80% 40% 20% 48% 15% 5% 0% Members Top 5% Costs Next 15% Bottom 80% 5 Top 5% High Cost/High Risk Members* Accounted for: • 90% of hospital readmissions within 30 days • 75% of total inpatient cost • Have an average of 4.2 conditions, 5 physicians, and 5.6 prescribers • 50% of prescription drug cost • 42% of the members in the top 5% in 2010, were also in the top 5% in 2009 *Excludes Long Term Care, IowaCare, Dual Eligibles, and maternity 6 Why change? • Health care delivery system is fragmented • Reimbursement methods reward volume not value • Cost of health care is unaffordable and unsustainable for citizens and taxpayers • We need to increase quality/outcomes & lower cost 7 What is Medicaid’s role in Delivery Reform? • Medicaid relies on the same health care system as all others to deliver care to our covered members • Medicaid uses very similar payment and contracting methods • Whatever is driving the rest of the health care system is also driving Medicaid • Medicaid is a significant payor - 2nd largest payor, covers 23% of Iowans 8 Iowa Health and Wellness Plan Background The Iowa Health and Wellness Plan was enacted to provide comprehensive health coverage for low-income adults • Begins January 1, 2014 • Iowans age 19 - 64 • Income up to and including 133% of the Federal Poverty Level (FPL) • New, comprehensive program will replace the IowaCare program, ending December 31, 2013 9 Iowa Health and Wellness Plan • The Iowa Health and Wellness Plan must receive approval from the federal government • DHS is working to obtain approval • Some program details may still change as we work with federal officials 10 One Plan, Two Options Iowa Wellness Plan • For adults age 19 - 64 • Income up to and including 100% of the Federal Poverty Level Marketplace Choice Plan • For adults age 19 - 64 • Income 101% to no more than 133% of the Federal Poverty Level 11 Iowa Wellness Plan: 0-100% FPL Family of one $11,490 Individuals up to 100% FPL Family of two $15,510 12 Patient Manager (PM) Benefits Payment Performance Fee for Service or Encounter Based Fee Claim submission Administrative Fee $4.00 Per Member-Per Month Wellness Exam Incentive $10.00 Per Member Annually if Threshold Achieved Up to $4.00 Wellness Plan Medical Home Value Index Score (VIS) Bonus Per Member Quarterly if Quality Target Achieved Iowa Wellness Plan: 0-100% FPL Program innovations include: • Ensure coordination of care for members through ‘medical homes’ • Ensure health care providers are accountable for achieving high quality and cost effective care that is focused on the patient Program innovations will continue to be developed through a statewide planning process related to the State Innovation Model* grant *Go to http://www.ime.state.ia.us/state-innovation-models.html for more information 14 ACO Option • Medicaid may contract with Accountable Care Organizations • ACO can earn the wellness exam and medical home bonus for attributed population • By Year 3: the Wellness ACO option will likely be replaced with the SIM initiative to develop a state-wide, full Medicaid ACO program. State Innovation Model (SIM) • Grants available to Governors from the Centers for Medicare and Medicaid Innovation • 2 tracks: Design (Iowa) or testing • Provides funding for developing State Health Care Innovation Plan • Iowa’s Plan will be complete by January • Will apply for Testing funds 2013 Design: State Health Care Innovation Plan 2014 Testing: Application for funds / authority to test 2016? Implementation 16 State Health Care Innovation Plan “Vision” •Patient-focused •Accountability • Aligned Quality Strategies •Economically Sustainable •Workforce Vision: Transform Iowa’s health care economy so that it is affordable and accessible for families, employers, and the state, and achieves higher quality and better outcomes for patients. 17 Iowa State Innovation Model Plans • Strategy 1: Implement a multi-payer ACO* methodology across Iowa’s primary health care payers Improve value and align payment models • Strategy 2: Expand on the multi-payer ACO methodology to address integration of long term care services and supports and behavioral health services Valued based payment reform Organized, coordinated delivery systems Build on developing health homes / medical homes Align payors to provide ‘critical mass’ to support needed investments in change • Strategy 3: Population health, health promotion, member incentives * ‘Accountable Care Organizations’ are a reimbursement method that incents accountability for outcomes and lowers costs 18 Goals of Iowa Wellness Plan • Begins to implement SIM Strategy 1 and 3 in the Wellness Plan – Implements medical homes and ACOs – Health Incentives for members to engage in Healthy Behaviors • • • 2/13/2012 Based on local access to care Focus on health and improved outcomes Emphasis on care coordination 19 Iowa Wellness Plan Reforms • Iowa will pay incentives to physicians and ACOs for achieving quality metrics consistent with Wellmark metrics • No claims history so starting with incentives and will move to shared savings for ACOs • Provides starting point to begin and learn, and will eventually be merged under larger Medicaid SIM designs 2/13/2012 20 Iowa Wellness Plan: 0-100% FPL Out of Pocket Costs: • No copayments except for using the emergency room when it is not an emergency • No monthly contributions during the first year (2014)* • No contributions for those with income below 50% FPL* • Costs cannot exceed 5% of income *Monthly contributions subject to CMS approval 21 Iowa Wellness Plan: 0-100% FPL Monthly contributions* waived beginning in 2015 if the member completes wellness activities First year (2014) members need to complete health risk assessment and wellness exam (annual physical) • 2015 and beyond will also other wellness activities *Monthly contributions subject to CMS approval 22 Marketplace Choice Plan: 101-133% FPL Family of one $11,491$15,282 Family of two $15,511$20,628 Individuals 101% FPL up to 133% FPL 23 Marketplace Choice Plan: 101-133% FPL Members select a certain commercial health plan available on the Health Insurance Marketplace Medicaid pays the premiums to the commercial health plan on behalf of the member – often referred to as “premium assistance” 24 Marketplace Choice Plan: 101-133% FPL Innovation: Purchasing private coverage Allows individuals to stay enrolled in their current plan if their income changes 25 Application Process Federal Health Insurance Marketplace www.HealthCare.gov DHS website www.dhs.state.ia.us DHS Contact Center 1-855-889-7985 APPLICATION PROCESS 26 Iowa Health & Wellness Builds PCP Capacity & Entry Point for New Population SIM Development Phase I: H&W Population Stronger Primary Care (PCP/MH) Incentivizes Medical Home Concepts, Prepares for ACO models Phase II: Full Medicaid , Statewide ACO Regions Stronger Care Management (Health Home (Chronic Condition & SPMI & BIPP) Stronger Home and Community Based Services (through BIPP) Sustainability through SIM Development, and Multiplayer Alignment Phase III: Fully Defined LTC and Behavioral health Accountability Future State: Current State: Mostly FFS Unmanaged Care Silos of Care Delivery Limited Access Volume Based Purchasing Value Based Purchasing Clear Accountability Integrated Care Delivery Alignment in Measures and Analytics Data are timely and Secure Stronger Mental Health System (Through Redesign Efforts) 27 Stakeholder Process • Workgroups met June – September, 2013 • • • • Metrics and Contracting Member Engagement Long Term Care Integration Behavioral Health Integration • Two Consumer Focused Workgroups (October) • Recommendations to Steering Committee, October 30, 2013 • Review and seek guidance from Legislative Subcommittee in November 2013 28 SIM Organizing Principles for Transformation • Dedicated and consistent leadership • Collaboration and open communication • Clarity in accountability • Transparency in Data • Alignment in measure and analytics Areas of Recommendation Across all Workgroups: • • • • • • • • Care Coordination/Community focus Communication/Technology Regulatory Financing Measures/data Transparency Provider Supports Patient Supports Access/Benefits 29 IowaCare Transition IowaCare Transition • IowaCare will end on December 31, 2013 • Current members will continue to have same access to services until the program ends o Continue to seek care at medical home IowaCare Transition • Current members will not be cancelled unless: o Premiums are not paid o Get other health insurance o Turn 65 o Move out of the state IowaCare Transition • DHS re-evaluated the decision that all IowaCare members will have to go through the full application process and will: o Centrally verify the income of all IowaCare members o `Administratively transfer` qualifying members into the Iowa Health and Wellness Plan IowaCare Transition • DHS must verify income in order to `administratively transfer` • Members who cannot be verified or whose income exceeds the Iowa Health and Wellness Plan limits will be instructed to proceed to the full application process IowaCare Transition • • • The verification/transfer process will take place by the end of October Members whose verified income indicates eligibility for Iowa Health and Wellness will receive confirmation of eligibility and will proceed to enrollment for physician selection, or qualified health plan selection Members whose income cannot be verified or cannot be transferred, or have income too high for the program will receive an additional letter instructing them to proceed to HealthCare.gov IowaCare Transition • Iowa Medicaid will: o Send letters to each IowaCare member before October 1 notifying them of this change in the verification/transfer process o Coordinate with medical homes on outreach o Reach out to members multiple times to make sure they are aware of transition Questions? Marni Bussell SIM Project Director Iowa Medicaid Enterprise mbussel@dhs.state.ia.us 515-256-4659 Lindsay Buechel Communications Manager Iowa Medicaid Enterprise lbueche@dhs.state.ia.us 515-974-3009 37