The Cell-Derived Mediators of Chemical Mediators of Inflammation
advertisement
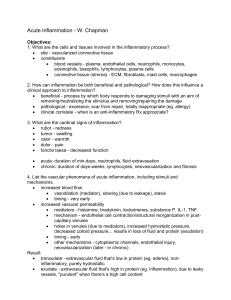
The Cell-Derived Mediators of Chemical Mediators of Inflammation Presented by Sara M. Al-Shaker Wed. 5/11/2008 King Saud University Riyadh, KSA Introduction • What are mediators? A mediator is a substance or structure that mediates a specific response in a bodily tissue General Properties of Chemical Mediators of Inflammation • Site of production Local or remote • Method of action Mostly by binding to receptors May have direct enzymatic and/or toxic effects General Properties of Chemical Mediators of Inflammation • Some mediators Stimulate release of secondary effector molecules • Actions of most mediators are tightly regulated Decay Enzymatic inactivation Elimination Inhibition Chemical Mediators of Inflammation Cell-Derived Plasma-ProteinDerived Chemical Mediators of Inflammation Cell-Derived Plasma-Protein-Derived Vasoactive Amines Eicosanoids PAF Cytokines Chemokines ROS NO Lysosomal Enzymes of Leukocytes Neuropeptides Chemical Mediators of Inflammation Cell-Derived Plasma-ProteinDerived Complement Coagulation and Kinin Systems Cell-Derived Mediators • Producing cells: Tissue macrophages Mast cells Endothelial cells Leukocytes Vasoactive Amines Histamine & Serotonin Vasoactive Amines • Among first mediators in acute inflammatory reactions • Preformed mediators in secretory granules Histamine • • Source: many cell types, esp. mast cells, circulating basophils, and platelets Actions: ARTERIOLAR DILATION INCREASED VASCULAR PERMEABILITY ENDOTHELIAL ACTIVATION • Inactivated by: Histaminase Histamine • 1. 2. 3. Stimuli of Release: Physical injury Immune reactions C3a and C5a fragments of complement (anaphylatoxins) 4. Leukocyte-derived histamine-releasing proteins 5. Neuropeptides (e.g. substance P) 6. Certain Cytokines (e.g. IL-1 and IL-8) Serotonin (5-HT) • Source: Platelets • Action: Similar to histamine’s • Stimulus: Platelet aggregation Eicosanoids Eicosanoids = Arachidonic Acid (AA) Metabolites = Prostaglandins (PG), Leukotrienes, and Lipoxins Eicosanoids • May be thought of as hormones but they differ from hormones by: 1. Produced in all tissues rather than in specialized glands 2. Act locally rather than after transport in blood to distant sites • • Decay spontaneously OR enzymatically Have short half-life Eicosanoids • Source: Leukocytes Mast cells Endothelial cells Platelets Arachidonic Acid • 20-carbon polyunsaturated fatty acid (4 double bonds) • Obtained from dietary linoleic acid • Present in the body in its esterified form as a component of cell membrane phospholipids • Released from phospholipids via phospholipases AA Metabolism • Two major enzymatic pathways: 1. Cyclooxygenase Prostaglandins & Thromboxanes 2. Lipooxygenase Leukotrienes and Lipoxins Chemical Mediators of Inflammation Cell-Derived Plasma-Protein-Derived Vasoactive Amines Eicosanoids PAF Cytokines Chemokines ROS NO Lysosomal Enzymes of Leukocytes Neuropeptides Platelet Activating Factor (PAF) • Another phospholipid derivative • Very potent bioactive molecule • Source: membranes of Neutrophils, monocytes, basophils, endothelial cells, & platelets • Derived by the action of Phospholipase A2 • Acts via G-protein-coupled receptor PAF • Actions: Platelet activation (aggregation & degranulation) Vasoconstriction Bronchoconstriction Leukocyte adhesion Leukocyte degranulation Chemotaxis Synthesis of other mediators, esp. Eicosanoids Cytokines • Polypeptides • Actions: Involved in early immune and inflammatory reactions Some stimulate bone marrow precursors to produce more leukocytes Cytokines • • • • Interleukins (IL) Tumor Necrosis Factor (TNF) Chemokines Interferon-γ (INF- γ) Acute inflammation: IL-1, TNF, & chemokines Chronic Inflammation: INF- γ & IL-12 TNF and IL-1 • Source: Activated macrophages Mast cells Endothelial cells • Stimulation: Bacterial endotoxins Immune complexes Products of T-lymphocytes (adaptive immune response) TNF and IL-1 • Actions: Endothelial Activation Both: 1. Stimulate expression of molec. on endothelial cells 2. Increased leukocyte binding and recruitment 3. Enhanced production of additional cytokines (notably chemokines) and eicosanoids TNF and IL-1 • Actions: TNF : • Thrombogenicity of endothelium • Neutrophil activation IL-1: • Tissue fibroblasts activation increased ECM N.B. TNF and IL-1 may enter the circulation and induce systemic acute-phase reaction Chemokines • • Small proteins They are chemoattractants for leukocytes • Main functions: 1. Leukocyte recruitment & activation in inflammation 2. Normal anatomic organization of cells in lymphoid and other tissues • Act via G-protein-coupled receptors (e.g. CXCR4 and CCR5 important for HIV entry into lymphocytes) Reactive Oxygen Species • Synthesized via NADPH oxidase pathway • Source: Neutrophils and Macrophages • Stimuli of release: Microbes Immune complexes Cytokines Nitric Oxide • • • • 1. Short-lived SOLUBLE Free-radical gas Isoforms of NO Synthase (NOS): Type I (nNOS) : neuronal, not significant in inflammation 2. Type II (iNOS): inducible, in macrophages and endothelial cells, NO production in inflammation 3. Type III (eNOS): constitutive, endothelium NO • Functions: 1. Vasodilation 2. Antagonism of platelet activation (adhesion, aggregation, & degranulation) 3. Reduction of leukocyte recruitment 4. Microbicidial (cytotoxic) agent (with or without ROS) in activated macrophages Lysosomal Enzymes of Leukocytes Leukocytes: Neutrophils & Monocytes Enzymes: • Acid proteases • Neutral proteases (e.g. elastase, collagenase, & cathepsin) Their action is checked by: Serum antiproteases (e.g. α1-antitrypsin) Neuropeptides • Small proteins • Secreted by nerve fibers mainly in lung & GIT • Initiate inflammatory response • Substance P : Transmits pain signals Regulates vessel tone Modulates vascular permeability Chemical Mediators of Inflammation Cell-Derived Plasma-Protein-Derived Vasoactive Amines Eicosanoids PAF Cytokines Chemokines ROS NO Lysosomal Enzymes of Leukocytes Neuropeptides THANKS! Have a nice day & a GREAT weekend!