COPD
advertisement

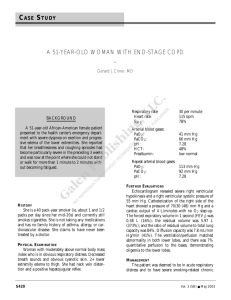
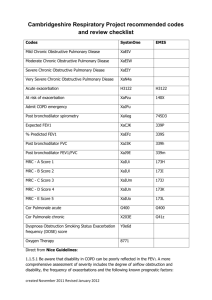
COPD Objectives • • • • How important is COPD? What is COPD? How to treat COPD? What is the prognosis? 19.3% of US Adults Smoke – 2010 CDC, NHIS 2010 2010 Current Smokers % of Smokers Demographic 19.3% US Adults % of Smokers Demographic 21.5% Males Education 17.3% Females 45.2% GED diploma Race 33.8% 9-11 yrs education 31.4% Native American/Alaska 23.8% High school diploma 27.4% Multiple race 9.9% Undergraduate degree 21.0% Caucasian 6.3% Postgraduate degree 20.6% African American 12.5% Hispanic 20.1% 18-24 9.2% Asian 22.0% 25-44 Poverty 21.1% 45-64 38.9% Below poverty level 9.5% 65 and older 18.3% At or above poverty Age CDC, NHIS 2010 Fact Sheet • 49.9 million former smokers/46.6 million current smokers in 2009 • 3rd leading cause of death in US in 2011 – 12.7 Million US adults have COPD – 24 million US adults have impaired lung function suggesting under diagnosis • Women are more likely to have COPD and die from it • 50% of COPD patients have limited ability to work CDC, NHIS 2009, 2011 Prevalence (%) of COPD by State in 2011 CDC, NHIS 2011 Etiology of COPD • 80-90% due to tobacco use • 15-20% of smokers will have clinical significant COPD • Occupational exposures • Bacterial/viral exposures • -1 protease inhibitor deficiency COPD RISK FACTORS Genes Exposure to particles Tobacco smoke Occupational dusts Indoor air pollution Outdoor air pollution Lung Growth & Development Oxidative stress Gender Age Respiratory infections Previous TB Low SES Poor Nutrition Co-morbidities Overall Mechanisms of Cigarette Smoke-Induced Lung Damage Inactivation of antiproteases Cigarette smoke- derived free radicals and oxidants Antioxidant genes Lipid peroxidation Oxidative Stress Depletion of antioxidant defenses Neutrophil sequestration Epithelial permeability I N J U R Y Inflammation ‘Susceptibility’ genes Transcription of proinflammatory cytokines MacNee W. Chest. 2000;117:303S-317S. Role of Bacterial/Viral Infections Vicious Circle Hypothesis Initiating factors (eg, smoking, childhood respiratory disease) Impaired mucociliary clearance Airway epithelial injury Progression of COPD Bacterial colonization Bacterial products Altered elastase antielastase balance Inflammatory response Increased elastolytic activity Sethi S. Chest. 2000;117:286S-291S. Viral pathogens Associated with COPD Exacerbations % Exacerbations 40 30 20 10 0 Sethi S. Infect Dis Clin Pract. 1998;7:S300-S308. Chronic Bronchitis Prevalence 2011 CDC, NHIS 2011 Emphysema Prevalence 2011 CDC, NHIS 2011 1st Hospitalization for COPD CDC, NHIS 2011 Pulmonary Function in COPD • Spirometry – Decreased FEV1 more than FVC; decreased ratio – Earliest change is a decrease in FEF25-75% • Lung Volumes – Increased Total Lung Capacity (TLC) – Increased Residual Volume (RV) – Decreased Vital Capacity (SVC) • DLCO – May be decreased Spirometry in COPD COPD Severity Classification Severity FEV1/FVC Mild ≤ 0.7 FEV1 % predicted > 80 Moderate ≤ 0.7 50-79 Severe ≤ 0.7 30-49 Very Severe ≤ 0.7 <30 ** ** < 50%predicted plus respiratory failure or clinical signs of right heart failure Smoking and COPD Males Females Former smokers 30 ml/year 22 ml/year Current smokers 66 ml/year 54 ml/year Anthonisen NR, et.al. Am J Respir Crit Care Med 166:675-9, 2002. Disease Progression Decramer Thorax 2010;65:837-841 Dynamic Hyperinflation Obstructive Diseases • Asthma – Reversible airflow obstruction – Inflammation prominent • Emphysema – Permanent – Destruction of the respiratory bronchioles • Chronic Bronchitis – Sputum production 3 months/year for 2 years Patients Have All Combinations Chronic Bronchitis Normal Lung Acinus Centrilobular Emphysema Panlobular Emphysema Centrilobular emphysema in COPD with no bronchial abnormalities Centrilobular emphysema in COPD with widespread bronchial wall thickening Centrilobular Emphysema • Emphysema of smokers and coal workers • Worst in upper lung fields of each lobe of the lung • Inflammatory changes in small airways are common Paraseptal emphysema • Selective expansion of alveoli adjacent to connective tissue septa and bronchovascular bundles • Most notable sub pleural • More Common in Young (<40) smokers Paraseptal Emphysema Don’t mistake this for honeycombing Panacinar = Panlobar Emphysema • Alpha1 antitrypsin deficiency and familial cases • Generally emphysema of non-smokers • Can co-exist with centrilobular • Most widespread and most severe • More severe at lung bases but distributed throughout lung Alpha 1 Antitrypsin Alpha 1 Antitrypsin • Lung and liver disease • Lower lung panacinar emphysema with bronchial wall thickening • Frank bronchietasis with PiZZ phenotype • Bullous formation relative uncommon • Serum protein that inhibits lysosomal proteases during inflammation preventing the damaging effects of elastases released by macrophages and neutrophils PiMM Normal 1-levels PiMZ Decreased 1-levels to 60% PiZZ Decreased 1-levels to 1020% GOLD • Collaborative project of NHLBI and WHO – Increase awareness of COPD – Decrease morbidity and mortality Stage Criteria Stage 0 (at risk) Chronic cough and sputum; Normal PFT Stage I (mild) FEV1/FVC<70%; FEV1 > 80%; ± Sx Stage IIA (moderate) FEV1/FVC<70%; FEV1 50-79%; ± Sx Stage IIB (moderate) FEV1/FVC<70%; FEV1 > 30-49%; ± Sx Stage III (severe) FEV1/FVC<70%; FEV1 < 30% or presence of respiratory failure or right heart failure Modified Stepwise Approach to Treatment MILD MODERATE SEVERE VERY SEVERE FEV1>80% FEv1 50-79% FEV1 30-49% FEV1<30% or failure Smoking cessation; Reduce risk factors; Vaccination Pulmonary Rehab based on functional status O2 Surgery Short acting bronchodilators PRN if respiratory symptoms Long acting bronchodilators ICS, if freq. exac (≥ 2/yr.) GoldCOPD.org Available Drugs SABA Albuterol Pirbuterol Levalbuterol Beta-2 agonists LABA Salmeterol Formoterol Arformoterol Olodaterol Budesonide Fluticasone Mometasone ICS ??? SAMA Ipratropium Antimuscarinics LAMA Tiotropium Aclidinium Roflumilast Theophylline ??? PDEI Short Acting b-agonists • All equal efficacy • Studies show HFA and CFC have equal efficacy • Tachycardia decreased with spacer use and rinsing mouth after use Importance of Spacer Barnes et.al 1998 Asthma Basic Mechanisms and Clinical Management Short Acting Anti-muscarinics • Decreases secretions • Longer acting than albuterol • Blocks bronchoconstriction from inhaled irritants • Spiriva – 4x/day = once a day Spiriva – Competitive inhibitor Cardiac Risk, Ipratroprium, Tiotropium • Better tolerated than beta-agonists • Meta-analysis - increased CV deaths in patients on anti-muscarinics • UPLIFT - 4 yr trial - decreased fatal cardiovascular event risk with Tiotropium • Clinical trial safety database Tiotropium – no increased risk Celli. Am J Respir Crit Care Med. 2009;180(10):948 Celli. Chest. 2010;137(1)20 Tiotropium Delays Next Exacerbation/ Hospitalization Niewoehner, D. E. et. al. Ann Intern Med 2005;143:317-326 GOLD ICS Therapy • Candidates – Symptomatic patients with spirometric response – Patient with daily sputum production – Patients with variability in symptoms – FEV1 < 50% with frequent exacerbations needing steroids or Abx • Trial 6 weeks – 3 months Oral Steroid Therapy • 10-20% will have significant response to oral steroids – 2 week trial of steroids improves PFTs then continue ICS • Effective for acute exacerbation • Antibiotics decrease relapse rate Oral Steroid Therapy • Conflicting results in stable COPD patients – Significant side effects • Exacerbations (10-14 day courses) – Decreased treatment failure – Rapid improvement in PFTs and symptom scores – Decreased in hospital stay – Maximum benefit in the first 2 weeks Thompson WH et al. Am J Respir Crit Care Med. 1996;154:407-412. Davies L et al. Lancet. 1999;354:456-460. Niewoehner D et al. N Engl J Med. 1999;340:1941-1947. Antibiotic Use • Chronic Macrolides – Decreases exacerbations – Increased resistance • Macrolides/Doxycycline at home for early exacerbation treatment Theophilline • Positive effects for COPD – Stimulate respiratory center – Improves muscle function – Anti-inflammatory • Negative effects for COPD – Increases GERD – Narrow therapeutic window – Significant drug-drug interactions – Significant food interaction (fatty foods) Roflumilast • Unknown exact mechanism – Selectively inhibits phosphodiesterase Type 4 leading to increased intracellular cAMP • Decreases exacerbations • Use with caution in liver disease, depression (suicide) Is There a Drug To Cure COPD? • No existing medications will change the inherent decline in lung function related to age/smoking • Goal of Tx: – Decreased symptoms – Decreased complications Other Modalities • • • • • Nutrition Post-nasal drip treatment Flu vaccine reduces serious illness Pneumovax: >65 or <65 with FEV1 <40% Statins?!? – Slower decline in PFTs, decrease exacerbation rate, decreased death rate Frost. Chest 2007;131:1006-12 Keddissi. Chest 2007; 132:1764-71 Aspiration and GERD - Risks • Medical risk factors – CVA, Parkinsons, Dementia, medications • Medication risk factors – Calcium channel blockers, bisphosphonates, iron supplements, NSAIDS, potassium, anticholinergics, narcotics, nitrates, progesterone, benzodiazepines Aspiration and GERD • PPI – before meals • Lifestyle changes – Elevation of head of bed 4-6 inches – Minimizing caffeine/mint – Avoiding eating/drinking 2-3 hours before bed Oxygen therapy 100 • PaO2 < 55 or • PaO2 = 56-59 with evidence of pulmonary hypertension, polycythemia or cor pulmonale 90 80 COT 70 Cumulative Survival (%) 60 50 MRC O2 NOT 40 MRC controls 30 20 10 0 0 10 20 30 40 50 60 70 Months Flenley DC. Chest. 1985;87:99-103 Pulmonary Rehabilitation • Benefit from exercise training programs • Improved health status – – – – ↑ exercise tolerance & QOL Return to function ↓ dyspnea & fatigue ↓ hospitalization & LOS • ↓ exacerbations • Improves survival Lung Surgery • Bullectomy • Lung Reduction Study - NETT trial – Increased mortality in patients with DLCO<25% predicted – Benefit in patients with asymmetric lung disease by HRCT – 7.9% 90 day mortality vs 1.9% control – 28% had improved exercise capacity at 6 months/15% at 2 years NETT. NEJM 2003: 348:2059-73. Lung Transplant • • • • • <=65 Maximal medical therapy Body weight 80-120% of ideal Favorable social factors $ Lung Transplant Contraindications • • • • • • Untreatable pulmonary infection Malignancy within last 2 years Significant dysfunction of other organs (heart) Significant chest wall/spine deformity Active smoking/drug and alcohol dependency Unresolved psychosocial problems (noncompliance) • HIV, Hep B, Hep C • Absence of social support Acute Exacerbation Classification • Level 1: Treatment at home • Level 2: Hospitalization Clinical Factors Favoring Hospitalization HR, RR, change in BP Hypoxia/ hypercapnea Significant comorbidities Elderly Poor home support Inadequate outpatient response ER Visit in last 2 weeks • Level 3: ICU/Specialized Care COPD Exacerbation Survival • 6 month mortality = 24% • 12 month mortality = 33% • Survival associated with albumin, BMI, PaO2, disease duration Gunen H, Eur Resp J. 2005; 26:234-241. Acute Exacerbation Treatment • Oxygen for low saturations • Bronchodilators – MDI vs nebulizer • Steroids 14 day max – IV vs Oral – Improves spirometry, decreases relapse rate – No study on taper • Education • Antibiotics Antibiotics and Survival • Retrospective cohort of 50K COPD pts in Netherlands • Median time to next exacerbation delayed • More benefit in worse exacerbations • Fewer treatment failures with newer Abx Roede et al. Thorax 2008: 63:968 NIPPV in Acute Exacerbations • If pH<7.35, if tolerated • Decreases symptoms/ morbidity/ mortality • Avoid in: – – – – CV instability, Uncooperative patient, ΔMS, Copious secretions, high aspiration risk, – Facial abnormalities Relapse Rate 20-40% • If ER visit : 33% recur within 14 days, 17% eventually need hospitalization • Risk of Relapse – Low FEV1 – Increasing medication use (BDs or steroids) – Prior exacerbations (3 within last 2 years) – Comorbid conditions Miravitlles M. Respiration 67:495, 2000. Heart Rate and COPD Prognosis Jensen. Eur Respir J, 2013; 42: 341-349. From Rabe, KF. NEJM 356:851-854. Prognosis • Patients hospitalized 6 mth mortality 24%; 33% 1 year; 39% 2 year; 49% 3 year FEV1 (L) Prognosis (years) 1.4 10 1.0 4 0.5 2 Gunen H, Eur Resp J. 2005; 26:234-241. Summary • Prevention is key – Smoking cessation – Prevent exacerbations and infections • Symptom management – Inhaled drugs may help symptoms • Combination therapy is better than monotherapy • Pneumonia risk increased with ICS • Oxygen improves longevity The REAL reason dinosaurs became extinct...