8-CML-3-2011
advertisement
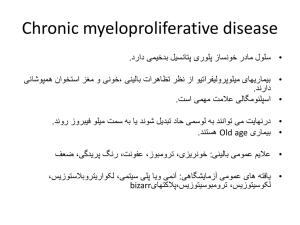
CML 9 9q+ 22 Ph 22q- Translocation ABL BCR ABL BCR Transcription and translation BCR-ABL fusion protein Inhibition by TKI Constitutive tyrosine kinase Phosphorylation of multiple substrates Mitogenic signaling and genomic instability increased Apoptosis and stromal regulation decreased CML Stem cell disorder Characterized by myeloproliferation Well-described clinical course *Clonal myeloproliferative disorder resulting from neoplastic transformation of pluripotent stem cells (affect myeloid, erythroid & megakaryocytic lineages) * proliferation, apoptosis *Cytogenetic hallmark: Ph chromosome positivity *7% to 15% of all adult leukemias (5th leukemia in USA) *Median age at diagnosis: 55 years (20% to 30% of patients ≥ 60 years) *Fatal disorder with poor prognosis *Median survival: 3-5 years (2 years without treatment) *Allogeneic SCT curative in 40% to 70% of patients (Associated with mortality and toxicity) *Interferon alfa ± cytarabine: CCyR of 20% to 30% Median survival: 6-7 years Also associated with adverse events *Other options: hydroxyurea, busulfan * The exact cause is not found * Pathogenesis is well established with consequences on treatment & prognosis *Possible association with ionizing radiation & exposure to industrial benzene Asymptomatic – accidentally discovered on routine CBC Anemia – easy fatigability, malaise, shortness of breath, chest pain, palpitation High metabolic rate - weight loss, fever Lt hypochondrial discomfort, easy satiety Bleeding- skin ecchymoses, bruises, petechiae UGI ulceration & bleeding (↑ s histamine due to basophilia) Thrombosis – thrombocytosis, leukocytosis Headache, bone pain, gouty arthritis, leukostasis, priapism Pallor, cutaneous bleeding, splenomegaly (one of the largest spleens) No lymphadenopathy Fever Weight Loss Hepatomegaly – less common than splenomegaly *85% of patients diagnosed with chronic-phase CML *50% of patients asymptomatic Symptomatic patients exhibit Constitutional symptoms Left upper quadrant discomfort Early satiety purpura ,Splenomegaly, hepatomegaly 1- Benign Phase – in which the disease behavior & response is predictable(Stable phase) 2- Accelerated phase – tumor burden increases rapidly with more systemic symptoms & increasing difficulty in control of disease 3- Acute phase – Blastic crisis may be AML,ALL, AUL Patient may present in accelerated or acute phase for the first time CBC- Hb↓, PCV↓, WBC↑ > 10000/µl Differential count – Neutrophilic leukocytosis different stages seen (blasts, promyelocytes, myelocytes, metamyelocytes, stab or band forms), eosinophilia, basophilia Thrombocytosis or thrombocytopenia LAP score ↓ or absent STC I, III ↑, SLDH↑, S histamine↑, S uric acid↑ Bone Marrow Aspirate & Biopsy- hypercellular, devoid of fat, myeloid hyperplasia, ↑retculin or collagen fibers, M:E ratio 15-20:1 Cytogenetics- Philadelphia chromosome positivity 95% (Ph –ve 5%) shortened long arm of chromosome22 Molecular biology- BCR/ABL gene positive * Balanced reciprocal translocation between chromosome 22 & chromosome 9 [t(9;22)] that brings BCR gene in juxtaposition with ABL gene forming a new hybrid gene BCR/ABL that codes for synthesis of a chimeric protein P210 that shows tyrosine kinase activity causing uncontrolled proliferation of the malignant clone 1- Leukemoid reaction rarely WBC count exceeds 30000, not clonal, BM no blasts excess, seen in overwhelming sepsis & disseminated TB. 2- MDS – CMML stage. 3- chronic corticosteroids use (demargination). 4- other MPD. Parameter Historical Perspective (Until 2000) Modern Perspective (Since 2000) Course Fatal Indolent Prognosis Poor Excellent Median survival, yrs 3-6 ≥ 25* Frontline treatment Allogeneic SCT, interferon alfa Imatinib Second-line treatment Not established Allogeneic SCT, novel TKIs Targeted Therapy1- Imatinib mesylate 400 mg/d - TKI targets the pathogenetic mechanism - revolutionized treatment causing CCyR & CMR S/E skin rash, edema, myelosuppression, hepatitis 2- Dasatinib & Nilotinib 2nd line for imatinib failure or hypersensitivity 3- high dose imatinib 600-800 mg/d * BMT when enter accelerated phase prior to acute phase * Interferon-α + cytosine arabinoside * Hydroxyurea orally * Busulfan (myleran) orally – no more used now because of severe & protracted myelosuppression 12345- Allopurinol H-2 blockers PPI Blood transfusion platelet transfusion It was an inevitably fatal disease With recent treatment became a curable disease compatible with long survival Newer agents are evolving Improving BMT &SCT results Once the patient enters the acute phase the only hope remains in transplantation & TKI are used as bridging to that Poor Prognostic Factors in CML • Older age • Splenomegaly • Anemia • Thrombocytosis, thrombocytopenia • Blasts, promyelocytes, basophils • Marrow fibrosis • Cytogenetic clonal evolution (Euro), MDACC Prognostic Models: Sokal, Hasford