CML Education Session – Susan Branford
advertisement
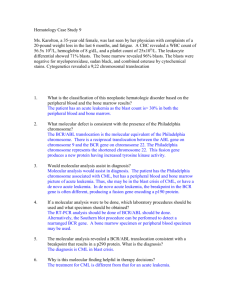
CML Education Session – Susan Branford Molecular Monitoring in Clinical Practice: In the past few years (since Iris Actually) Molecular monitoring of CML has become an integral part of CML management of patients. This is because many CML patients achieve CCR and therefore, Cytogenetic analysis provides limited information on the kinetics of residual disease. Conversely molecular monitoring can indicate pending disease relapse. By rising BCR ABL levels and the degree of reduction of BCR ABL correlates with PFS. As well, failure to achieve MMR at 18 months of IM therapy is now deemed suboptimal response, and reassessment of therapy is the order of the day. Importantly molecular analysis for the IRIS trial was not comprehensive since patients were only tested once CCR was achieved. Response considered as trial end points were hematological response as well as CCR – technology and knowledge has certainly evolved since then. The newer trials with TKI’s have included molecular monitoring and mutation analysis is also included as mutations are the major mechanisms of IM resistance. Molecular endpoints have also been used to guide treatment algorithms in clinical trials for patients with relapse following Allo SCT. However, good molecular monitoring needs to be provided outside of a clinical trial and as standard good practice in following patients in the clinical setting. So, there is a concerted effort to optimize, standardize and incorporate an international reporting scale. The majority of patients have a high level of p210 BCR ABL transcripts. If these are absent atypical transcripts must be found, otherwise the rare patients without P210 may be precluded from analysis by quantitative PCR as False negative values may be reported during monitoring. It has been shown for IM treated patients that the probability of remaining progression free for those who achieved MMR at 12 months was 100% for the 5 years. An MMR in the first year for CP CML without prior treatment with IFN was predictive of a durable CCR PFS. Molecular and Cytogenetic response is generally comparable leading one to consider whether molecular monitoring alone is sufficient to monitor patients. Only Cytogenetic analysis can monitor for the acquisition of clonal abnormalities. These may be associated with disease progression. Clonal abnormalities in Ph- cells may, although infrequently be associated with MDS and acute leukemia. In a study of 183 patients it was determined that patients who had achieved an MMR would not benefit from BM, preferring to select BM for patients who either did not achieve a MMR or who had lost MMR. Regular molecular monitoring after Allo stem cell is a good tool for detecting early response. Patients with persistently low levels of BCR ABL had the highest risk of relapse. An International Reporting Scale (IS) was proposed where BCR ABL absolute value representing MMR is standardized at 0.10% . A value of 1.0% is equivalent to CCR. The IS will eliminate terms such as “Standardized baseline” and Log reduction”. This is replaced by BCR ABL/control gene percentage value. The laboratories that performed molecular analysis in the IRIS trial fix the scale. An alternative method is to calculate the bias between patient BCR ABL values to those of a particular lab to the values generated by the IRIS lab. If comparison of the values is consistent then the mean bias between the specific laboratory and the reference laboratory defines the conversion factor. The future promises to simplify the standardization process by providing standardization kits. The ability to detect KD mutations as they emerge is key to effective patient monitoring. Particularly in the case of IM failure, suboptimal response and rising BCR ABL values. In a study of 171 patients with IM failure, mutations occurred more frequently in later disease stage, older age, prior IFN therapy development of clonal evolution, high risk Sokal at dx and failure to achieve CCR with IM. In another study of 297 patients with IM failure mutations were detected frequently with acquired resistance and in those who had commenced IM therapy in advanced phase. The most common mutations that occur in IM resistance is Y253, E255, and T315 – transplant is recommended. Mutations of M244, F317 and M351 confer low-level resistance and indicate suboptimal response. Patients identified with Y253H have shown to be moderately resistant to Nilotinib, while patients with F317L are moderately resistance to Dasatinib. Mutations are not the only indicator of IM resistance. Molecular monitoring can follow increasing BCR ABL levels. This may also show Cytogenetic abnormalities in Ph+ clones which has been detected in 58% of IM resistant patients. The addition of second Ph Chromosome indicates amplification of the BCR ABL gene with a reported overall frequency of 18%. The challenge in the future is more widespread adoption of molecular monitoring. It is essential to monitor patients in order to understand loss of response to BCR ABL inhibitors and to guide therapy. Some BCR ABL KD mutations may not respond optimally to alternate TKI therapy and some create more biologically aggressive forms of BCR ABL.