conduction of both sensory and motor
advertisement

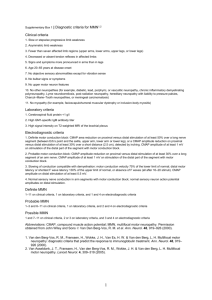
By Dr shereen algergawy associate prof rheumatology and rehabilitation Benha faculty of medicine The speed of conduction of both sensory and motor fibers is determined by the integrity of heavily myelinated fibers and the preservation of saltatory conduction between individual nodes of Ranvier. . If the myelin is disrupted between the stimulus and recording sites, the recorded potential will be delayed in onset. This measurement is called the distal latencv and in sensory conductions is the time from the stimulus onset to the peak of the sensory nerve action potential (SNAP in sensory nerves is calculated by dividing the measured distance between the stimulation and recording sites by the distal latency. With a supramaximal stimulus, all of the axons beneath the stimulator should depolarize, resulting in a waveform amplitude commensurate with the number of underlying axons depolarized. The amplitude is measured from the peak to the trough of the SNAP . Each EMG laboratory should have normal values with controls for patient age and height. Skin temperature should be controlled, which may require warming the limb. in sensory nerves is calculated by dividing the measured distance between the stimulation and recording sites by the distal latency. With a supramaximal stimulus, all of the axons beneath the stimulator should depolarize, resulting in a waveform amplitude commensurate with the . Each EMG laboratory should have normal values with controls for patient age and height. Skin temperature should be controlled, which may require warming the limb. Conduction velocity in sensory nerves is calculated by dividing the measured distance between the stimulation and recording sites by the distal latency. With a supramaximal stimulus, all of the axons beneath the stimulator should depolarize, resulting in a waveform amplitude commensurate with the number of underlying axons depolarized. The amplitude is measured from the peak to the trough of the SNAP (Fig-1B). Each EMG laboratory should have normal values with controls for patient age and height. Skin temperature should be controlled, which may require warming the limb. all of the axons beneath the stimulator should depolarize, resulting in a waveform amplitude commensurate with the number of underlying axons depolarized. The amplitude is measured from the peak to the trough of the SNAP (Fig-1B). Each EMG laboratory should have normal values with controls for patient age and height. Skin temperature should be controlled, which may require warming the limb. Technical errors such as 1- not placing the recording electrode directly over the nerve being tested or 2-not achieving supramaximal stimulation of the nerve can artificially lower the amplitude of the SNAP. Factors such as 3- inaccurate distance measurements or 4-a cold limb can markedly alter distal latency and conduction velocity determinations Motor NCSs can aid in the assessment of the etiology of weakness. A recording surface electrode is placed over the belly of the muscle being studied . Through orthodromic, supramaximal stimulation of the motor nerve at a fixed distance, a waveform called the compound motor action potential (CMAP) is obtained (Fig-2B). This waveform represents the summation of the depolarization of muscle fibers beneath the recording electrode. This distal latency is determined by recording the time from the stimulus onset to the initial motor response. The motor nerve is then stimulated from a second, more proximal site and a second CMAP is obtained. The conduction velocity of the nerve segment between stimulation sites is calculated by dividing the distance between stimulation sites by the difference between distal latencies. In motor nerves such as the ulnar or peroneal nerve that are commonly susceptible to compression about fixed structures, a third stimulation site is used to span the possible compression site. The conduction velocity can then be calculated from each of the two proximal sites and compared. Focal slowing of more than 10 m/s in a short segment is considered significant. With supramaximal stimulation of the motor nerve, all motor fibers beneath the stimulus are depolarized, resulting in a maximal contraction of the muscle being recorded. The amplitude of the CMAP is thus dependent on the state of the motor axons. Amplitude is measured from the baseline to the peak of the CMAP. However, other processes besides axonal failure can result in a low CMAP amplitude. If muscle mass is decreased from any cause such as a previous central nervous system injury or malnutrition, the CMAP amplitude can be lowered. Also, severe myopathy or neuromuscular junction disease can result in a low CMAP amplitude. EMG is thus needed to clarify the cause of the low CMAP amplitude. The area of the CMAP correlates with the amplitude and may better reflect the amount of muscle being depolarized owever, other processes besides Evaluating the amplitude and degree of dispersion of the CMAP can greatly assist in understanding the underlying pathophysiology of the nerve lesion. Neurapraxia refers to nerve conduction failure without axonal loss and implies a demyelinating lesion. If enough fibers fail to conduct impulses because of conduction block across a given segment, the CMAP amplitude will decrease during nerve stimulation proximal to the block; 25 to 30 percent is a significant degree of change in most nerves. Focal slowing affecting fast conducting fibers will delay the CMAP. If there is differential slowing of slow conducting fibers along a nerve segment, the CMAP waveform will be dispersed, thus demonstrating a desynchronization of fiber firing. Motor NCSs are difficult technically and errors may result from improper placement of electrodes, incorrect measurements, or submaximal stimulation. Once again, height, age, and skin temperature are Another parameter that can be measured to evaluate conduction along a motor nerve is the F-wave, one type of late response. This response is obtained with supramaximal stimulation while motor conduction studies are being performed. When a nerve is stimulated there is depolarization of that nerve in both directions. The F-wave response is caused by recurrent firing of the anterior horn cell after antidromic conduction. Therefore both the afferent and efferent limbs of this response are motor. Because this response evaluates proximal nerve conduction, it can be useful in evaluating patients for root or plexus injury. It may be especially useful in the acute stage before evidence of peripheral nerve degeneration and denervation changes (as detected by EMG) has developed. Because of the length of nerve traveled by the impulses, normal values are different based on the subject's height. F-wave latencies are determined by analyzing at least 10 Fwaves and recording the earliest latency. Another type of late response, the H-reflex, is different from the F-wave in that the afferent limb of the H-reflex is sensory and the efferent limb is motor. The H-reflex is tested by stimulating the tibial nerve in the popliteal fossa and recording from the gastrocnemius muscle. The H-reflex afferent limb is through the S1 root. Responses are determined with submaximal stimulation and are compared to the responses on the contralateral side. An asymmetry of 2 ms is considered significant. Normal patients may have bilaterally absent Hreflexes so that bilateral absence of response is not necessarily pathologic. Both F-wave latency and Hreflexes are most useful when peripheral conduction studies are normal; abnormal responses suggest a proximal lesion. However, when routine motor conduction is abnormal, abnormality of these late responses may not necessarily be indicative of a proximal lesion. After nerve injury, such as with a remote history of a radiculopathy, late responses may remain abnormal indefinitely. Therefore the interpretation of an abnormality would benefit from comparison with a previous study. To summarize, distal latency and conduction velocity measurements are particularly helpful in evaluating the speed of conduction along distal and midportions of a peripheral nerve, respectively. The F-wave latency is particularly useful in evaluating conduction along proximal segments of a motor nerve if the distal segments are normal. When the electromyographer uses the term demyelinating features. reference is made to prolonged distal latency, slow conduction velocity, prolonged F-wave latency, or dispersed waveforms. The amplitude of the CMAP is altered by failure of conduction to the muscle and the waveform may be helpful in understanding the reason for the altered conduction. Axonal features usually imply low amplitudes. However, an EMG study of the muscle is needed to clarify the reasons for a low CMAP amplitude Both sensory and motor conduction studies are highly reproducible, although there is better intra-examiner reliability than inter-examiner reliability. Conduction studies are focused on an area of clinical abnormality; distant areas are studied also, to classify the abnormality as focal, multifocal, or diffuse. In studies in which a focal conduction block is suspected but not definitely proven by the routine studies, a technique called inching can be used. The region of the suspected block is studied by nerve stimulation above and below the presumed site of the block at 1-cm intervals searching for a focal dramatic change in distal latency. These studies are frequently useful in the evaluation of a suspected carpal tunnel syndrome, ulnar neuropathy at the elbow, and peroneal neuropathy at the knee. excess of acetylcholine packets and receptors are present, which ensures successful neuromuscular junction transmission. However, in patients with neuromuscular junction disorders this safety factor is diminished and repetitive stimulation, usually at 1 to 3 Hz, causes failure of neuromuscular junction transmission, resulting in a excess of acetylcholine packets and receptors are present, which ensures successful neuromuscular junction transmission. However, in patients with neuromuscular junction disorders this safety factor is diminished and repetitive stimulation, usually at 1 to 3 Hz, causes failure of neuromuscular junction transmission, resulting in a decremental response in CMAP amplitude or area. Standard guidelines include comparing the response produced by the first stimulus to the response produced by the fourth stimulus; an abnormality is defined as a decrement of at least 10 percent (Fig-3). Decrements on repetitive stimulation are not specific for primary neuromuscular junction disease and can be seen in any circumstance in which neuromuscular junction transmission is faulty. Such circumstances include motor neuron disease and patients receiving drugs that are active at the neuromuscular junction. The sensitivity of repetitive nerve stimulation is higher when a clinically weak muscle is being tested. A normal test in a clinically normal muscle does not rule out the presence of neuromuscular junction disease, and additional muscles should be studied to increase the yield. Commonly studied muscles include the abductor pollicis brevis, abductor digiti quinti, extensor digitorum brevis, trapezius, and facial muscles A repetitive nerve stimulation study demonstrating a 61 percent d to the fourth stimulation. ecrement in area and a 54 percent decrement in amplitude from the first Blink responses, like the corneal reflex, allow evaluation of trigeminal sensory and facial motor conduction. Surface electrodes are placed on the orbicularis oculi muscles bilaterally, along with surface reference electrodes and a ground. Stimulation of the supraorbital nerve or a glabellar tap results in an ipsilateral response via a pontine pathway through the main sensory trigeminal nucleus and the facial nucleus. The response is designated R1. Thus, , this R1 response evaluates trigeminal and facial nerve conduction. Subsequent to the R1 response is a second bilateral response, designated R2, that is polysynaptic and more diffuse in brain stem localization. The RI response is best used for evaluating conduction velocity along the trigeminal and facial nerves because it is a shorter reflex. The R2 response is best used in localizing the lesion to right or left trigeminal or facial nerves. These studies along with routine motor conduction studies of the facial nerve and EMG of the facial muscles may be useful in analyzing several disorders affecting the facial and trigeminal nerves.