6_Acute Inflammation
advertisement

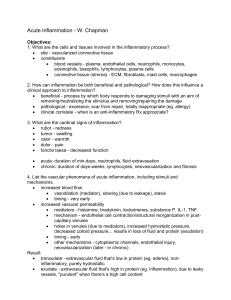
Chapter 6- Acute Inflammation Info not covered in Los: Vasculature (p.7-9) More detail on each leukocyte (p.13-16) 1) Understand that inflammation is the reaction of vascularized living tissue to local injury: (p. 5) -inflammation is defined as the reaction of vascularized, living tissue to local injury. The ultimate goal of the inflammatory response is to destroy, eliminate or wall off the injuring pathogen or agent. Under normal circumstances inflammation is benefical to the host since it allows us to survive in a hostile enviornment. Acute inflammation is actually part of the innate immune response. -In order for inflammation to occur the injured tissue must be vascularized since it is thru the vasculature that leukocytes travel to reach the damaged tissue and the endothelium lining the vasculature at the site of injury coordinates and modulates many activites associated with inflammation such as -blood flow thru the capillary beds -intravascular coagulation status -leukocyte adhesion to the vasculature -leukocyte transmigration into the tissue 2) List five causes of inflammation: 3) Know the five cardinal signs of inflammation: (p.5) -reddness (rubor) -heat (calor) -pain (dolor) -swelling (tumor) -loss of function 4) Know the sequence of events in acute inflammation: (p. 6-7) A) Transient vasoconstriction B) Vasodilation C) Increased blood flow D) Increased vascular permeability E) Hemoconcentration and slowing of flow or statis F) Leukocyte trafficking See Figure 1A and 1B on p. 6 and 7 -this series of events is controlled by coordinated expression of soluble mediators and adhesion molecules, and that the events occur sequentially. Thus, interruption of any one of these steps may decrease the inflammatory response. Will discuss in more detail in later sections 5) Understand Starlings equilibrium: (p.9 and fig 4 on p.10) -Since cell-cell junctions betw most endothelial cells are not water-tight, fluid can move back and forth betw the lumen of the capillary and the extravascular space. Typically, plasma fluid is forced out of the capillary (filtered) at the arteriole end and absrobed at the venous end. Under normal circumstances equilibrium is established across the capillary wall which balances the filtration pressures and the absorption pressures -3 components are essential for the equilibrium to be maintianed: -intact functioning blood vessels -intact functioning lymphatic vessels -adequate intravascular [] of the serum protein albumin -4 forces that govern fluid flow either in or out of the capillary -Promote fluid movement OUT of the capillary: (given a + value) -plasma hydrostatic pressures (blood pressure) -tissue osmotic pressure -Promote fluid movement INTO the capillary: (given a – value) -tissue hydrostatic pressure -plasma osmotic pressure -Net filtration pressure (arteriole side) and the net absorption pressure (venule side) are determined by summing these 4 pressures. -if net filtration is greater, then this means that more fluid is leaving the capillary then is being reabsorbed. Thus, this extra fluid is taken up by lympathic vessels and returned to circulation. 6) List four general causes of edema: (p.10-11) -Edema is the accumulation of fluid in the perivascular tissue space. This fluid came from within the capillaries as a result of an upset to Starling’s euqilibrium. A) Increased Vascular Premeability -Occurs following tissue damage, this is what happens to allow the accumulation of fluid at sites of acute inflammation. -Mild Tissue Damage: results in the degranulation of mast cels and release of histamine, which promotes increased vascular permeability by increasing the size of fenestration betw endothelial cells, allowing water and electrolytes to escape into the perivascualr tissue. However, this minor damage does not cause endothelial denudation so protein and leukocytes remain within the vessel. -Severe Tissue Damage: This results in both mast cell degranulation and damage to the endothelium lining regional blood vessels. Therefore, water, electrolytes, plasma proteins and leukocytes leave the vessel and enter the perivascular tissue. The proteins will pull additional water out of the capillary worsening the edema. B) Lympathics Obstruction -In normal tissues, lymphatic vessels drain the excess filtered fluid from capillary beds. Obstruction or dirsuption of these lympathic vessels will result in the accumulation of excess tissue fluid. Common cause is surgery where the lymphatic vessels at the surgical site are transected, and swelling persists until new lymphatics can be formed to drain the area. Other causes are parasites, neoplasia or inflammation in which the lymphahtics get obstructed with pathogens and WBCs. C) Increased Plasma Hydrostatic Pressure -Most commonly due to increased venous pressure which can either be a local phenomenon (caused by clot or neoplastic obstruction) or generalized (caused by right heart failure). D) Decreased Colloid Osmotic Pressure -Significant loss of plasma protein, namely albumin. This can be caused by glomerulonephritis (albumin is filtered and excreted in urine) or decreased syn by the liver or severe protein malnutrition. 7) Know the major granule products of neutrophils: (p.13) A) Primary granules- large, oval electron dense and contain the most important neutrophil enzyme- myeloperoxidase. Other enzymes included are neutral proteases, lysosomes and acid hydrolases. B) Secondary granules- smaller, less electron dense and more numerous. They contain lysosomes, lactoferrin, collagenase and others. -These are lethal enzymes that can kill bacteria or damaged the host tissue. 8) Understand Oxygen dependent and independent killing mechanisms: (p.14) Oxygen DependentA) Oxygen radical system- during phagocytosis the neutrophils and macrophages demonstrate a respiratory burst which is characterized by 2-3 fold increase in O2 consumption and an increase in glucose metabolism by HMS. A unique membranebound NADPH oxidase is activated and causes the reduction of O2 by electron transfer from NADPH resulting in the formation of O2- and NADP. O2- spontaneously degrades into toxic O2 radicals such as singlet O2 and OH radicals and H2O2. -Singlet O2 and OH radicals are the main participants and kill bacteria by oxidizing lipids in their cell wall. B) Myeloperoxidase-halide system – myeloperoxidase catalyzies the rnx of H2O2 with various halides (Cl, Br, I) to form molecules such as OHCl. These molecules are much more lethal to bacteria than oxygen radicals. Oxygen Independent-enzymes that hydrolyze the bacterial cell wall muramic acid polymerr (lysozyme) -proteases with activity against a host of bacteria and fungi (Cathepsin G, Defensin) -iron-binding proteins that interfere with bacterial respiration (lactoferrin) The other acid hydrolases in the granules are for digestion of the killed bacteria. 9) Understand the role of myeloperoxidase in oxygen metabolites formation: (maybe the above question) 10) Understand how neutrophils may mediate tissue damage: (maybe p.13) 11) List the major eosinophil granule products and their major function: -Granules contain similar complement of enzymes and bacertiacidal proteins as neutrophil granules, except that they lack lysozyme and phagocytin. -The most abdundant component is Major Basic Protein. It is cationic due to its large # of Arg molecules and it is extremely toxic to parasites. It can also serve to amplify an immune response by causeing mast cells and basophils to degraunulate. It causes bronchioconstriction and can neutralize the anti-coagulant protein heparin. -Eosinophil cationic protein is also found in granules and is extremely toxic to parasites and has pro-coagulant activity. -Also contain substanced that neutralize the mediatoras released by degranulating mast cells. -Histaminase- inactivates histamine -Arylsufatase B- inactivates leukotrienes LT C4, LT D4, LT E4 -Phospolipase D- inactivates platelet activating factor (PAF) -Eosinophils also phagocytose mast cell granules therefore illustrating their ability to have a negative regulatory effect on mast cells. 12) Describe the similarities betw mast cells and basophils: (p. 12 and 16) -Mast Cells: They are resident leukocytes and as such as present in the tissue prior to inflammation. -Derived from the bone marrow -Nuclues is typically ovoid and centrally located in the cytoplasm -2 phenotypically distinct subsets: -Mucosal Mast cells- most numerous within the submucosa of the gut, resp, and urogential tract. -CT Mast cells- found in CT anywhere in the body. -Store massive amts of preformed histamine, heparin, and various proteases within intracytoplasmic granules. -Fe receptors that bind IgE and C5a receptors, when either receptor is bound it leads to the degranulaton of the cell in which histamine is released and causes clinical symptoms associated with acute inflammation- vasodilation, edema, pruritis. -severe form of this is anaphylaxis where you have systemic degranualtion of mast cells and basophils is repsonse to antigen and binding of IgE. This is life threatening and is treated with Epi. -Basophils: Leukocytes that traffic to damaged tissue following injury. -They derive from a stem cell in the bone marrow and are distinguished by the presence of granules that stain dark blue and have multilobulated nucleus. They are not abundant in the peripheral blood. -Contain granules filled with histamine, heparin, and proteases and other biologically important mediators. -Have Fc receptors for IgE on the cell surface that when cross-linked lead to degranualtion. 13) Understand how platelets contribute to acute inflammation: (p. 17) A) Promote vasodilation and increased vascular permeability: activated platelets release serotonin, which mediates these effects B) Express adhesion molecules: activated platelets express P-selectin which allows leukocytes to adhere to the growing platelet mass (thrombus) at the site of vascular damage. C) Express chemokines: Once activated, platelets release chemotactic cytokines such as RANTES which promotes leukocyte (particularly monocyte) recruitment. D) Promote leukocyte activation: acitvated platelets express CD40L (CD40 ligand) which binds to CD40 on the surface of the recruited monocytes, thus causing activation of the latter cell types. E) Promote acitvation of the clotting cascade: the plasma membrane of the acitvated platelet constitutes the suface upon which sevel important reactions in the clottting cascade occur. Ex: athrosclerotic disease is a chronicinflammatory disease in which platelet aggregation and adhesion plays a central role. 14) Know the source and function of histamine and serotonin: (p. 18-19) -They are vasoactive amines that mediate peractue vascular changes and ae produced by cells and are sequestered intracellularly in cytoplasmic granules. Histamine: found in the granules of mast cells, basophils and platelets and are released by degranulation. Histamine receptors (H1 and H2) are found on endothelium, sm muscle, and lymphocytes. It is an extemely important mediator of inflammation serving to promote type 1 epithelial cell activation resulting in vasodilation, increased vascular permeability, and increased surface adhesion molecule expression. This results in decreased blood flow (redness/heat), perivascular fluid accumulation (swelling/edema) and leukocyte adhesion. -Histamine may also cause relaxtion of precapillary arterioles by binding sm mus H2 receptors and causing the relaxtion of the vessel wall. -It can also bind endothelial H1 receptors activating the release of NO. -Stimulates endothelial production of PAF which promotes endothelial cell contraction and increased vascular permeability. -Can be the result in the production of wheal and flare or anaphylatic responses to antigens. Serotonin: Stored in the granules of platelets and in the mast cells of rodents. It binds to specific 5-HT receptors on endothelium and vascular sm muscle. -It promotes type 1 endothelial activtion resutling in vasodilation, increased vascular permeability, and increased surface adhesion molecule expression.(same as histamine) -Thus, in the early stages of inflammation, histamine and serotoinin act very rapidly (min) and produce the cardinal symptoms of inflammation. 15) Know the source and function of nitric oxide: (p.19 and fig 5 on p.20) -made in the endothelial cells -it may have both anit- and pro-inflammatory effects depending on the []. -it is formed from NOS (nitric oxide synthase) -in normal conditions NO is produced by endothelium (eNOS) and interacts directly with vascular sm muscle to produce a basal state of relaxation. This level of NO also has anit-inflammatory effects since it reduced leukocytes adhesion to the endothelium. -during inflammation, iNOS is expressed by macrophages and other cells resulting in excess NO prodcution. At the same time, have activated neutrophils which produce superoxide which combines with NO to form a potent free radical- peroxynitrite- which has antibacterial and anitviral activity. It can also damage host tissue, DNA and promote neoplastic transformation. -damaged to vascular endothelium decreases NO production resulting in increased vasculare tone at the stie of lesion and increased leukocyte adhesion, promoting further vessel damage. 16) Know the major functions of complement components C3a, c3b, and c5a in acute inflammation: (p.22) A) Vascular effects: C3a and C5a promoste increased vascualr permeability and vasodilation by binding to specific complement receptors on mast cells and promoting histamine release. C5a activates the lipoxygenase pathway of arachodonic acid metabolism in neutrophils and monocytes promoting further release of inflammatory mediators. B) Phagocytosis: C3b and C3bi bind to the surface of bacteria, they promote opsonization of the bacteria by neutrophils and monocytes which have the C3b surface receptor. C) Leukocyte activation, adhesion and chemotaxis: C5a is chemotactic for neutrophils, monocytes, eosinophils and basophils bc these cells possess C5a receptors. C5a also activates these cells and promotes firm adhesion to blood vessel walls by increasing the avidity of leukocyte surgace adhesion molecules. C3a has chemotactic abilities too, but to a much less degree. 17) Understand how the kinin system contributes to acute inflammation: (p.22) -Kinins are potent vasoactive peptides (ex: bradykinin) -They are generated by the activation of the clotting cascadeactivation of factor XII this converts inactive prekallekrein to active kallekreinthis converts heavy molecular weight kininogen to bradykinin. -Bradykinin causes a) relaxtion of vascular sm muslce= dilation of blood vessels, b) contraction of visceral sm muscle and c) pain. -Kallerkrien activates the fibrinolytic cascade by cleaving plasminogen to plasmin which splits fibrin into fibrin degradation products (FDPs) which increase vascular permeability. 18) Understand how the clotting cascade contributes to acute inflammation: (p.23) There are 3 main sites where the clotting cascade promotes actue inflammationA) Activation of Factor XII (Hageman Factor)- once activated, this enzyme acitvates the kinin system that promotes vasodilation and sm muscle contraction at sites of inflammation. B) Thrombin acitivation- Activation of the clotting system results in activation of thrombin (Factor 2a) from its precursor prothrombin (Factor 2). Thrombin catalyzes the conversion of fibrinogen to fibrin which produces fibrinopeptides as by-products which serve to increase vascular permeability and are chemotactic for leukocytes. Thrombin is also a potent activator or platelets! C) Activation of the fibrinolytic system- In addition to promoting fibrin formation, factor XII a also directly activates tissue plasminogen activator which subequently catalyzes the conversion of plasminogen to plasmin. Plasmin in turn splits fibrin into fribrin degradation products that may increase vascular permeability. 19) Understand the interaction of the clotting, kinin, plasinogen, and complement pathways: (p.23 and fig 7 on p.24) -Factor XIIa can directly activate that clotting cascade, the kinin cascade and the fibrinolystic cascade. Enzymes generated in each of these pathways such as thrombin, kallekrien and plasmin respectively can direclty activate the complement cascade since all three enzymes are C3 convertases. In addition, kallekrien and plasmin promote additional activation of Factor XII and XIIa, prepetuating the cycle. It is Factor XII that links these 4 enzyme cascades together. Inflammatory mediators may be derived from sources other than cytoplasmic granules and plasma proteins. For example, eicosanoids are a group of mediators that include prostaglandins (PGs), leukotrienes (LTs), and lipoxins (LXs). These mediators serve as both intracellular and extracellular signals, having effects on inflammation, vascular permeability, vascular tone, and hemostatsis. Generally speaking, eicosanoids are formed from raw phospholipid material, particularly arachodonic acid (AA). Following stimulation of a cell by mechanical, physical, or biochemical (e.g. cytokine, C5a, PAF) stimulus, activated phospholipase A2 liberates AA from the plasma membrane. AA can then be metabolized by one of two pathways: - Cyclooxygenase pathway –production of prostaglandins - Lipoxygenase pathway –production of leukotrienes and lipoxins Phospholipase A2 is inhibited by corticosteroids 20) Understand the biosynthesis and function of prostaglandins and TXA2: (p.25,27, fig 8 on p.26) Prostaglandins (PGs) are synthesized from arachodonic acid (AA) via the cyclooxygenase (COX) pathway, which is mediated by two enzymes: COX-1 and COX-2. COX-1 - Constitutively expressed (always present) in most tissues, though principally by endothelium and to a lesser extent, vascular smooth muscle - Involved in the production of physiologic levels of prostaglandins COX-2 - Inducible enzyme (not always present) produced principally by endothelial cells and vascular smooth muscle at sites inflammation and tissue trauma Both COX-1 and COX-2 catalyze the conversion of AA to the precursor molecule, prostaglandin G2 (PGG2). PGG2 is subsequently converted to produce PGD2, PGE2, PGF2 by a cascade of specific enzymes Functions of prostaglandins - In general, PGs promote vasodilation and potentiates edema - PGE2 promotes hyperalgesia (abnormal increased sensitivity to pain/nociceptive stimuli) - PGs (particularly TXA2 and PGI2) play a vital role in vascular homeostasis, as shown below When platelets accumulate at a site of inflammation or tissue damage, they express COX-1 and their major AA product is thromboxane A2 (TXA2). TXA2 promotes platelet aggregation, vasoconstriction and smooth muscle proliferation. If left unopposed, TXA2 would ultimately promote vascular thrombosis. However, endothelium and vascular smooth muscle cells at sites of inflammation or tissue damage are simultaneously induced to express COX-2. Furthermore, their major AA product is PGI2, which promotes vasodilation and inhibits platelet aggregation, effectively opposing TXA2 action. The balance b/w TXA2 (prothrombotic) and PGI2 (antithrombotic) production ultimately determines whether blood flow is blocked by a thrombus (TXA2 dominant) or remains patent (PGI2 dominant) at a site of inflammation or tissue damage. COX inhibitors - Given the role PGs play in acute inflammation, several drugs were developed to block their production, achieved via inhibition of the COX enzymes responsible for their synthesis - The first COX inhibitors were non-selective non-steroidal anti-inflammatory drugs (ns-NSAIDS) that blocked both COX-1 and COX-2. These drugs include aspirin, indomethacin and ibuprofen. Interestingly, the anti-inflammatory benefits of ns-NSAIDS are principally derived from COX-2. - The next generation of COX inhibitors are NSAIDS, which are specific for COX-2 and had the benefit of relieving symptoms of acute inflammation without the undesirable side effects of gastrointestinal ulceration and potential renal damage. These drugs include Vioxx and Celebrex and were found to be potent inhibitors of the symptoms of acute inflammation. However, due to a small number of patients developing detrimental cardiovascular events during therapy, the drugs were indefinitely pulled from the market. 21) Understand the biosynthesis and function of leukotrienes: (p.27, fig 8 on p.26) Leukotrienes (LTs) are synthesized from arachodonic acid (AA) via the lipoxygenase (LO) pathway, the mechanism of which follows: - Enzyme 5-lipoxygenase (5-LO), found principally in leukocytes, catalyzes the conversion of AA to 5HPETE. 5-HPETE is subsequently converted to either 5-HETE or LTA4. LTA4 may be further metabolized to leukotriene LTB4. Within leukocytes, LTA4 is converted to LTC4. After release into the tissue fluid, LTC4 is converted extracellularly to LTD4 and LTE4. Functions of leukotrienes - Both 5-HETE and LTB4 are chemotactic for neutrophils - LTB4 activates neutrophils by promoting aggregation, adhesion to endothelium, and release of cytoplasmic granules - LTC4, LTD4, and LTE4 promote vasoconstriction, increased vascular permeability (in venules), and bronchospasm - Generally speaking, LTs are particularly important in the pathogenesis of asthma - 5-LO inhibitors such as Zileuton are sometimes used to treat patients with severe asthma It is interesting to note that although non-leukocytes lack sufficient quantities of 5-LO to produce leukotrienes from AA, many cells express distal LTA4 metabolizing enzymes and can metabolize leukocyte-derived LTA4 into other bioactive leukotrienes in a process called “transcellular biosynthesis” (as described in lipoxin biosynthesis below) 22) Understand the biosynthesis and function of lipoxins: (p.27, fig 8 on p.26) The key to lipoxins synthesis is transcellular passge of AA metabolites. For example, platelets contain the enzyme 12-lipoxygenase, which catalyzes the formation of lipoxins LXA4 and LXB4 from the leukotriene LTA4. However, platelets do not have the capacity to produce LTA4 themselves. Instead, they collect LTA4 from neutrophils at a site of inflammation and then convert it to lipoxin. Thus, lipoxin synthesis requires cell-to-cell contact in order to facilitate the necessary transfer of LTA4. Functions of lipoxins - Inhibit neutrophil chemotaxis and adhesion - Promote monocyte chemotaxis and adhesion - LXA4 promotes vasodilation and attenuates vasoconstriction promoted by LTC4. 23) Know which drugs inhibit various steps in the biosynthesis of prostaglandins, leukotrienes, and lipoxins: (p.25, 27) See questions 20 and 21 for the discussion of COX inhibitors (prostaglandin synthesis inhibition) and 5-LO (leukotriene synthesis inhibition) 24) Understand the source and function of PAF: (p.27, 28) - Platelet activating factor (PAF) is an inflammatory mediator derived from membrane phospholipids (chemical structure is acetyl-glyceryl-ether-phosphorylcholine – AGEPC) - Cells known to produce PAF include neutrophils, basophils, monocyte/macrophages, endothelial cells and platelets - Stimuli reported to promote PAF formation include C5a, thrombin and antigen binding to surface-bound IgE (basophils) - PAF is short-lived and metabolized by PAF acetylhydrolase Upon elaboration from cells known to produce PAF, PAF binds to a specific receptor on the surface of target cells, which include leukocytes, smooth muscle, and endothelium. Binding initiates a complex intracellular signaling pathway that causes the following profound cellular changes Functions of PAF at high concentrations - Platelet activation and aggregation - Smooth muscle contraction resulting in vasoconstriction and bronchoconstriction Functions of PAF at lower concentrations - Promotes vasodilation and increased vascular permeability in postcapillary venules - Stimulates leukocytes, resulting in leukocyte adhesion to blood vessel walls (via increasing integrin affinity), chemotaxis, degranulation, and the oxidative burst - Stimulates leukocytes to elaborate other inflammatory mediators (e.g. eicosanoids), thus amplifying the local immune response 25) Know which mediators cause hyperaesthesia (pain): General Concepts Regarding Cytokines (p.28) It is the goal of the body to destroy, eliminate or wall off the injuring pathogen, sometimes at the expense of tissue damage. Subsequently, damaged tissue is removed, remodeled, and repaired in a complex series of events that requires careful coordination and communication between various cell types. One major mechanism of cell-cell communication involves the production of cytokines, small proteins (8-30 KDa) that modulate the function of other cell types, particularly leukocytes and endothelial cells. Cytokines are produced by many types of cell types, including “activated leukocytes”, endothelium, fibroblasts, and epithelium. Chemokines are a specialized subset of cytokines that promote leukocyte chemotaxis and activation (see discussion of leukocyte trafficking). Generally speaking, cytokines have either pro-inflammatory or anti-inflammatory effects (note that a given cell may produce a variety of both pro- and anti-inflammatory cytokines and a given target cell may express multiple cytokine receptors). Furthermore, the cytokine environment at a site of inflammation serves to determine the types of leukocytes recruited. The state of the environment at a site of inflammation may be described as follows: Complex cytokine milieu in which leukocytes are suspended, constantly bombarded by both pro- and anti-inflammatory signals. Whichever signal is stronger determines whether inflammation will continue or resolve. We can therapeutically manipulate this environment by blocking specific cytokines in order to shift the equilibrium (i.e. blocking pro-inflammatory cytokines to shift the equilibrium towards antiinflammatory signaling) 26) Know the principle functions of TNF-a, IL-1, IL-6, IL-8, IL-17, IL-23: (p. 28-32) Table 2 on p.31 is a good summary of the effects of key inflammatory mediator TNF-α and IL-1 - Two of the most important cytokines involved in acute inflammation - Highly synthesized by dendritic cells and macrophages within sites of tissue damage - Help mediated the acute inflammatory response at both local and systemic levels and via various communicatory mechanisms: Autocrine – Both IL-1 and TNF-α may be secreted from a macrophage and then bind to receptors on that macrophage. Via this autocrine amplification loop, there is an increase in cytokine production, phagocytic capability of the macrophage, and cell motility Paracrine – Both IL-1 and TNF-α act on neighboring endothelial cells to promote endothelial activation. This process involves upregulation of endothelial adhesion molecules, enhanced thrombogenesis, and increased expression of cytokines, chemokines, eicosanoids, and nitric oxide. These changes favor leukocyte recruitment into the inflamed tissue. Endocrine – Both IL-1 and TNF-α can act systemically to promote fever, inappetance, neutrophilia, ACTH and corticosteroid release, and the formation of acute phase reactant proteins by the liver. Furthermore, TNF-α indirectly promotes features of endotoxic shock (hypotension, decreased blood pressure, increased heart rate). - Play important roles in chronic inflammatory diseases, including rheumatoid arthritis, psoriasis, multiple sclerosis, and inflammatory bowel disease - Several potent TNF-α antagonists, including Enbrel (soluble TNF-α receptor) and Adalimumab (antiTNF-α antibody) have shown great efficacy in treating rheumatoid arthritis patients via blockage of this cytokine IL-6 As mentioned above, there is a massive influx of neutrophils into damaged tissue following injury. Within the first day or so, the population of infiltrating leukocytes begins to switch from neutrophils to monocytes and lymphocytes. This leukocyte shift is partly mediated by IL-6. - Expressed in many different cell types, including macrophages, lymphocytes, fibroblasts and smooth muscle cells - Suppresses the production of IL-8 within inflamed tissue, resulting in decreased neutrophil trafficking and influx. In addition to the decreased neutrophil influx, neutrophils present only live for ~6 hours before undergoing apoptosis, further reducing their numbers - IL-6 is ultimately responsible for initiating the transition from a neutrophilic to mononuclear cell infiltrate in acutely inflamed tissues by shutting down the production of IL-8 and increasing the production of MCP-1. It does this via the following mechanism: Apoptotic neutrophils release massive quantities of a soluble IL-6R (sIL-6R), which binds IL-6 in the local environment. Within tissue, this IL-6/sIL-6R complex binds to a receptor on fibroblasts, stimulating the production of MCP-1 (monocyte chemotactic protein-1). MCP-1 then promotes monocyte and lymphocyte recruitment to the inflamed tissue. - IL-6 is spread systemically via blood to the liver where it induces a hepatic acute phase response - Functions in secondary lymphoid tissues to promote B cell maturation and antibody production IL-8 - Important during acute inflammation - Behaves as a chemokine to promote neutrophil recruitment and activation within acutely damaged tissues - In quiescent tissues, IL-8 is synthesized by endothelial cells and stored (preformed) in Weibel-Palade bodies for immediate release upon endothelial cell activation - Within endothelial cells and injured tissues, IL-8 may be newly synthesized by resident macrophages, epithelial cells, fibroblasts, and other cells - Within a few hours after tissue injury, massive quantities of IL-8 are made locally within the injured tissue, a response largely responsible for the wave of trafficking neutrophils to the site IL-23 - Produced by dendritic cells and macrophages (to a lesser extent) - Synthesized following cell stimulation through pattern recognition receptors (e.g. TLRs, NOD) during exposure to invading pathogens - Supports the differentiation and expansion of Th17 CD4+ T cells, which subsequently produce IL-17 IL-17 - Induces production of G-CSF and IL-8 by epithelial cells and fibroblasts, resulting in increased neutrophil production by the bone marrow and enhanced neutrophil trafficking to the site of bacterial invasion - Net effect of IL-17 in acute inflammation is to provide enhanced resistance to extracellular bacteria. Consequently, mice deficient in IL-23, IL-17 or their receptors have enhanced susceptibility to specific bacterial pathogens An acutely inflamed tissue contains a complex mixture of inflammatory mediators, many of which have direct effects on the blood vessels supplying the tissue while others serve to attract and/or activate leukocytes responding to the injury. The observed clinical signs of inflammation (redness, heat, swelling, pain, loss of function) are a direct result of these processes. 27) Understand the differences between innate and adaptive immunity: (p.32, 33, Table 3 on p.33) Immunity serves a general function of protecting organisms against pathogens. Two functional arms of the immune response – innate immunity and adaptive immunity – serve to convey this protection, though do so via different mechanisms and pathways. Innate immunity - Responsible for controlling the proliferation of invading pathogens until an efficient lymphocyte (adaptive) response can be generated - Highly conserved throughout evolution, as indicated by the ability of phylogenetically lower organisms (i.e. jellyfish, fruit flies) to survive in the modern environment - Plays a major role in establishing acute inflammation during infection - Mediated by pattern recognition receptors Adaptive immunity - Allows for a long-lasting, antigen-specific response - Relies on clonal expansion of antigen-specific T and B lymphocytes - Although efficient at eliminating most pathogens, the immune response time is longer (5-7 days), requiring time for lymphocyte clonal expansion and differentiation into effector cells - The average bacterial generation time is on the order of 20 minutes, meaning organisms cannot rely solely on adaptive immunity to control an infection, as invading bacteria would overwhelm the immune system more quickly than a response could be generated The receptors of innate immunity are distinct from the antigen-specific receptors of adaptive immunity in several important ways Innate pattern recognition receptors - Innate receptors are highly conserved throughout evolution, are encoded in germ-line DNA, rarely mutate, and have identical specificities - Innate receptors are constitutively expressed on most leukocytes (NK cells, dendritic cells, macrophages, granulocytes) and many non-leukocytes (endothelial cells) - Because pattern recognition receptors of the innate immunity are so widely expressed by both leukocytes and non-leukocytes, an invading pathogen can immediately activate massive numbers of immune cells. This results in the release of cytokines and inflammatory mediators, ultimately promoting development of an acute inflammatory response at precise site of invasion - Rapid innate response may be sufficient to eliminate pathogen Adaptive receptors (TCRs and BCRs) - The receptors of adaptive immunity, TCRs and BCRs (antibodies), undergo extensive mutation in order to acquire antigen-specificity - Display limited expression on T cells or B cells (0.0001%) - Because there are so few antigen-specific T and B cells of the adaptive response, these cells must proliferate until there are sufficient numbers of activated cells to eliminate the pathogen, a process that can take 7 to 10 days 28) Know the major classes of innate receptors: (p.33-35) Functionally, innate pattern recognition receptors can be divided into 3 basic categories: 1. Endocytic receptors – constitutively expressed on macrophage and dendritic cell surfaces Macrophage mannose receptor – binds to microbial structures bearing mannose, fucose and Nacetylglucosamine on their surface Macrophage scavenger receptor – involved in uptake of gram-positive bacteria, gram negative bacteria (e.g. LPS), complex carbohydrates, nucleic acids and low density lipoproteins (LDLs) 2. Signaling receptors - Expressed by cells of the innate immunity - Recognize protein, carbohydrate, and nucleic acid pathogens, resulting in cellular activation and cytokine production Toll-like receptors (TLRs) - Expressed by cells of the innate immunity (play an essential role in innate immunity) - Recognize various pathogen molecular patterns and transmit a signal intracellularly - At least10 TLRs have been identified in the mice and humans TLRs expressed on the cell surface TLR-1: Triacyl lipoproteins TLR-2: Lipoproteins, bacteria, fungi, viral glycoproteins TLR-4: LPS from gram-negative cell walls, viral glycoproteins TLR-5: Bacterial flagellin TLR-6: Diacyl lipoproteins TLR-10: Unknown TLRs expressed on the plasma membrane of endosomes TLR-3: Double-stranded viral RNA TLR-7: Uracil-rich single-stranded viral RNA such as HIV TLR-8: Single-stranded viral RNA TLR-9: Unmethylated CpG DNA of bacterial and viral genomes CD14 - Expressed on surfaces of phagocytes (monocytes, macrophages and neutrophils) - Cooperates with TLR-4 to activate macrophages following binding of LPS NOD (nucleotide-binding oligomerization domain) family NOD proteins are cytosolic proteins that allow intracellular recognition of peptidoglycan components. Binding of these components to NOD proteins leads to the activation of genes coding for proinflammatory cytokines NOD1 recognizes peptidoglycan more common in gram (-) bacteria than gram (+) NOD2 recognizes peptidoglycan found in most bacteria RNA helicases - Cytosolic proteins that allow intracellular recognition of double-stranded viral RNA, resulting in cellular activation and cytokine production 3. Secreted receptors (collectin family) - Facilitate microbial clearance via aggregation, complement activation, opsonization, activation of phagocytosis, and inhibition of microbial growth Mannose-binding lectin - Secreted into the blood by the liver to bind mannose residues on invading pathogens - Potent activator of the complement cascade via the Lectin pathway Surfactant proteins A and D - Enhance clearance of organisms by alveolar macrophages in the lung - May participate in the clearance of naked DNA and RNA 29) Describe how the innate and adaptive immune repsonses are linked: (p. 35, 36) Innate and adaptive immune responses are linked at the level of the antigen presenting cell (APC). Following exposure to an antigen, APCs activated through pattern recognition receptors secrete large amounts of pro-inflammatory cytokines that initiate an acute inflammatory response (innate immunity). Activated APCs (principally dendritic cells) migrate to regional lymph nodes and present antigen, in the context of MHC class I or II molecules, to CD8 and CD4 lymphocytes. T cell antigen recognition (signal 1) is followed by APC up-regulation of costimulatory molecules (signal 2), resulting in activation of T cells that then provide long-lasting immunity against the pathogen. 30) Understand that acute inflammation is a major component of innate immune response: 31) Know the steps involved in leukocyte trafficking and the major adhesion molecules invovled during each step: (p.36-41) Following tissue injury, leukocytes (that developed in bone marrow) travel through the bloodstream and traffic to the site of the lesion to participate in acute inflammation. This process requires crossing of 3 physical barriers: a) Endothelial cells b) Endothelial basement membrane c) Pericytes surrounding the vessel Leukocyte trafficking requires a complex navigation system involving several steps that must occur in the proper sequence. If any one of the steps is interrupted, leukocytes are inhibited from trafficking to a tissue. Furthermore, each step involves specific mediators, which can be blocked to prevent leukocyte trafficking and diminish the inflammatory response. Steps in leukocyte trafficking (let’s follow a neutrophil to a site of acute inflammation) Capture (tethering) - Occurs when a neutrophil enters a blood vessel (often a capillary) supplying an inflamed tissue - Selectins and selectin ligands (both glycoproteins) expressed on endothelial cells and leukocytes form a molecular zipper that allows loose neutrophil adherence to endothelium L-selectin is constitutively expressed by leukocytes P-selectin - Expressed by activated platelets - Contained preformed within endothelial Weibel Palade bodies and is rapidly moved to the surface of the endothelial cell upon activation (30 minutes) E-selectin is synthesized de novo by endothelial cells and moved to the plasma membrane following endothelial cell activation (4-6 hours) PSGL-1 is the most common selectin ligand Rolling Once captured, the neutrophil may either detach and move back into circulation or become more firmly adhered, causing rolling along the surface of the endothelium in the direction of the blood flow. Whether the neutrophil remains captured or begins to roll is a function of the number of selectin molecules the cell encounters Few selectin molecules results in capture Many selectin molecules results in rolling Slow rolling - As the neutrophil rolls closer to the inflammatory site, it encounters more adhesion molecules Signaling through the L-selectin and PSGL-1 molecules on the neutrophil surface recruit another class of integral plasma membrane adhesion molecules – integrins - Integrins are dimeric transmembrane protein molecules composed of α and β chains that pair in various combinations to form ~20 unique integrins - In non-activated leukocytes, integrin molecules are present in low affinity conformation that prevents them from participating in leukocyte adhesion to the endothelium - In activated leukocytes, selectin and selectin ligands induce a conformational change of integrin molecules, first to intermediate then to higher affinity states - Integrin molecules on neutrophil surface interact with integrin ligands on endothelial surface Most important integrin ligands ICAM-2 – constitutively expressed on endothelium ICAM-1 – up-regulated by endothelium at sites of inflammation Other important integrin ligands VCAM-1 – up-regulated by endothelium within sites of inflammation (esp. CNS) MAdCAM-1 - Constitutively expressed on Peyers Patch HEVs - Up-regulated during chronic inflammation - LFA-1 integrin molecule and integrin ligand interaction produces slow-rolling of the neutrophil Arrest - As neutrophil reaches the site of acute inflammation, it is exposed to chemokines released by endothelial cells and various other cell types within the damaged tissue - Chemokines (8-10 KDa) can be divided four families based on primary acid structure - Generally speaking, chemokines have two N-terminal cysteine residues that may be immediately adjacent (C-C group), separated by one amino acid residue (C-X-C group) or separated by three amino acid residues (C-X3-C group) - There is a single member of the C group – chemokine lymphotactin - Cell surfaces must express an appropriate chemokine receptor for responding to a chemokine - Chemokine receptors are 7 transmembrane-spanning molecules coupled to G proteins - Upon chemokine binding to its receptor, a cascade of intracellular events is initiated, resulting in a variety of effects on the cell - Increased intracellular Ca++ levels - Enhanced integrin expression and conformational change to a high affinity state Chemotaxis in the direction of the chemokine - Degranulation - Cytokine production and/or respiratory burst - Leukocytes express multiple chemokine receptors on their surfaces and can therefore respond to a variety of chemokines - Chemokine receptors are found on numerous other cell types including neurons, astrocytes, microglia, endothelium, smooth muscle, and epithelium, tumore cells - In this case, the neutrophil slowly rolling along the endothelial surface encounters chemokine IL-8 produced by endothelium - Neutrophil becomes activated, inducing switching of LFA-1 integrin molecules from intermediate to high-affinity configuration - LFA-1 molecules then bind to ICAM-1 molecules on the activated endothelium, ultimately causes the neutrophil to become strongly adhered to the endothelium in neutrophil arrest Adhesion strengthening and spreading - Arrested neutrophil receives signals through high-affinity LFA-1 molecules that cause additional integrin molecules to bind to endothelium - Activated neutrophil also undergoes a shape change, causing it to flatten and spread out along the endothelial surface - At this point, the neutrophil is activated, tightly adhered to the endothelium, and prepared for transition into the extravascular space Intravascular crawling - Neutrophil “crawls” along endothelial surface in search of a thin place to cross into the extravascular space - The endothelial migration of the neutrophil and ultimate crossing across the vessel wall is largely mediated by chemokines (e.g. IL-8) that diffuse from the site of tissue damage and establish a concentration gradient for the neutrophil to follow - As neutrophil crawls, surface LFA-1 molecules engage and signal endothelial ICAM-1 molecules to promote further activation of the endothelium - These integrins, in conjunction with other endothelial-activating molecules (e.g. histamine, TLR agonists, TNF-α, IL-1, etc.), prepare the endothelial cell for neutrophil transmigration Paracellular transmigration - The majority of leukocyte emigration occurs between adjacent endothelial cells via paracellular transmigration (as quickly as 5 minutes) - Endothelial cells are normally adhered to one another via adhesion molecules (e.g. CD99, PECAM1, VE cadherin). However, endothelial activation during intravascular crawling causes these interactions to break down, resulting in increased space between endothelial cells - Increase intercellular space results in increased microvascular permeability and local edema - Because neutrophils express integrin and adhesion molecules (CD99, PECAM1, VE cadherin, LFA-1) while endothelial cell edges express integrin ligands, the neutrophil is able to slide between endothelial cells (transmigration) using adhesion molecules like a molecule zipper - Once reaching the basement membrane, the neutrophil elicits enzymes that help the cell digest and traverse perivascular connective tissue Transcellular transmigration Not only does leukocyte migration involve transmigration between adjacent endothelial cells, but up to 20% of leukocyte migration occurs via transcellular transmigration. Here, leukocytes move directly through the cytoplasm of the endothelial cells (as quickly as 1 minute). - This mode is particularly common in vessels where the endothelium is thin and the cell-cell junctions are tight (i.e. in the CNS). After crossing the basement membrane, neutrophils follow chemokine gradients to the vicinity of invading pathogens. There, they unleash (via degranulation) a formidable array of bactericidal weapons. Neutrophils that do not degranulate during the acute inflammatory response are destined to die via apoptosis within about 6 hours of leaving the bloodstream. 32) Understand the structure and function of chemokines and chemokine receptors: (p. 38, 39 and Table 4 on p.39) See question 31 33) Understand the structure and functions of integrins: (p. 38) See question 31 34) Understand the functions of vascular endothelium in quiescent tissues: (p.41) Under normal circumstances, the vascular endothelium maintains smooth blood flow, effectively suppressing the clotting cascade, preventing platelet adhesion, opposing leukocyte adhesion, and maintaining some vascular relaxation. Following tissue injury, the endothelium may become activated, a response that can be divided into two categories: 1. Type I activation – response is rapid, independent of new gene expression, and self-limiting 2. Type II activation - response is slower, dependent upon new gene expression, and persists until inflammatory stimulus is cleared How does endothelium maintain smooth blood flow during normal circumstances? - Endothelium is coated with heparan sulfate, which binds to anti-thrombin III (direct thrombin antagonist), thus inhibiting the terminal step in the clotting cascade - Endothelial-derived thrombomodulin binds to thrombin, causing thrombin to cleave protein C to an active molecule, thus inhibiting several steps of the clotting cascade - Endothelium produces abundant NO (nitrous oxide) via action of eNOS, causing relaxation of vascular smooth muscle and the prevention of platelet and leukocyte adhesion - Endothelium constitutively expresses COX-1, which catalyzes PGI2 production and promotes further smooth muscle relaxation - Leukocytes are normally displaced to the vascular wall by RBCs. This “marginated pool” of cells rolls along the endothelium via interaction of L-selectin and PSGL1. However, in the absence of endothelial activation, these cells detach and return to the “circulating pool” 35) Understand the changes that occur in vascular endothelium during type I endothelial activation: (p. 41-42) How does endothelium become activated? - Histamine, released in the tissue following mild injury or mast cell degranulation, binds to a specific receptors on the endothelial surface, causing a cascade of events resulting in immediate, or Type I endothelial activation - Signaling through the histamine receptor induces a shape change in endothelial cells that results in increased vascular permeability to water and electrolytes - Large plasma proteins and clotting constituents remain within the vascular space - Because the histamine receptor can be readily desensitized by continual histamine presence, this form of endothelial activation is self limiting and short lived - Once receptor is desensitized or histamine is removed from the environment, endothelial cells return to their normal resting state What changes occur once endothelium is activated? - Weibel Palade bodies present in endothelial cell cytoplasm travel to the cell surface, fuse with the plasma membrane, and release Factor VIII (vWF), PAF, and IL-8 into circulation - vWF participates in clotting cascade and promotes platelet adhesion to the vascular wall - PAF and IL-8 attract and activate neutrophils - Weibel Palade bodies fused with plasma membrane express P-selectin, which aids in neutrophil capture, rolling, and some margination into perivascular space - Endothelial cells expressing COX-1 synthesize eicosanoids (particularly PGI2) and NO to promote vasodilation and increased blood flow (causes rubor and calor) Therapy/treatment for type I endothelial activation - Depends on the severity of clinical symptoms If inflammation is local (i.e. mild thermal/solar burn) - COX inhibitors (Most of the reduction in the redness and heat of sunburn following a dose of aspirin is due to decreased vasodilation via inhibition of eicosanoid synthesis) If patient is experiencing anaphylaxis (systemic type I activation) - Epinephrine to promote immediate vasoconstriction and restore blood pressure - Anti-histamines to block the histamine receptor - Corticosteroids/COX inhibitors (e.g. aspirin, ibuprofen) to inhibit eicosanoid production 36) Understand the changes that occur in vascular endothelium during type II endothelial activation: (p.42-43) How does endothelium become activated? - Occurs following severe tissue damage (persistent infection, severe thermal/chemical burns) - Endothelium is exposed to cytokines TNF-α and IL-1β (produced by local leukocytes), which bind to receptors and cause type II endothelial activation - Cytokine binding induces shape change and new gene translation in endothelial cells - Inflammatory stimulus, via cytokines, can cause direct endothelial necrosis - Combination of endothelial shape change and necrosis vastly increases permeability, allowing plasma fluid and protein to enter perivascular space (results in severe edema) - TNF-α and IL-1β receptors are not readily desensitized, allowing type II endothelial activation to persist indefinitely at a site of inflammation What changes occur once endothelium is activated? Exposure of basement membrane induces numerous effects - Weibel Palade bodies release vWF, which immediately binds to the collagen matrix and promotes platelet adhesion and activation - Activated platelets expose Gp IIb/IIIa receptors, bind fibrinogen, and cross-link with one another to form a thrombus - Platelets of growing thrombus release TXA2, which promotes local vasoconstriction - Activated platelet surfaces are activation sites for the local clotting system and, thus contribute fibrin to the thrombus - NO production is significantly reduced, resulting in increased vascular tone - Production of bradykinin (vasodilator) via kallekrein pathway increases - Kallekrein and clotting cascades activate complement, liberating C3a and C5a (vasodilators) - COX2 production increases to yield huge quantities of PGI2 and other vasodilatory PGs - Weibel Palade bodies fused with plasma membrane express P-selectin (within 30 minutes) and synthesize E-selectin (within 4-6 hours) to promote additional leukocyte capture and rolling - Endothelium synthesizes chemokines MCP-1, IL-8, and others that promote leukocyte adhesion and pericellular/transcellular migration - Endothelium can capture and display chemokines secreted by other cells, causing further leukocyte recruitment and activation - Endothelium synthesizes and displays integrin ligands ICAM-1 and VCAM-1, allowing chemokineactivated leukocytes to firmly adhere to the endothelium and traffic to tissue - Ultimately, type II endothelial activation results in massive leukocyte margination into tissue Thus, in severely inflamed tissue, there are mediators that promote vasoconstriction (TXA2) and those that promote vasodilation (bradykinin, C3a, C5a, PGI2). The net result on vascular tone depends upon which mediators, vasoconstrictive or vasodilatory, predominate Therapy/treatment for type I endothelial activation - TNF-α antagonists (e.g. Enbrel, Remicade) are used to treat patients with rheumatoid arthritis and other chronic inflammatory diseases - IL-1β antagonists are currently in clinical trials - COX2 antagonists have potent anti-inflammatory effects via inhibition of vasodilatory prostaglandin synthesis (Note: COX2 has been responsible for unexplained cardiac side-affects)