Identification and Management of Neurobehavioral Problems
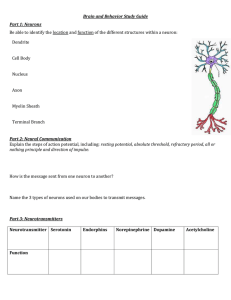
advertisement

Cognitive Rehabilitation and Traumatic Brain Injury Mary Pepping, Ph.D., ABPP-CN Professor and Director Neuropsychological Evaluation Service and Outpatient Neuro-Rehabilitation Program UW Department of Rehabilitation Medicine A quick bit of history for cognitive rehabilitation Pioneer Yehuda Ben-Yishay, Ph.D. and injured Israeli soldiers Observed problems in thinking and behavior for the first generation of longterm survivors Development of milieu-based interdisciplinary neuro-rehabilitation - a day hospital model to address problems Evolution of Cognitive Rehabilitation Identifying and understanding TBI changes in thinking and behavior How much caused by injury to brain? How much caused by injury to the self? Is the person aware of deficits? Are they able to tolerate treatment? Can they form an alliance with the clinicians? What produces the common pattern of difficulties > TBI? Architecture of skull and brain Mechanical forces impacting brain Frontal and temporal lobe injuries common Primary effects, e.g., contusion, shear Secondary effects, e.g., swelling, subdurals Tertiary effects, e.g., chemical cascade Severity of injury - mild, moderate, severe Whose brain was injured? Frontal Lobe Impairments: Neurocognitive problems Attention, concentration, distractibility Tangentiality Problems with planning & organization Impaired initiation and follow-through Trouble with main ideas and inference Concrete thinking, literal-mindedness Problems with word retrieval Frontal Lobe Impairments: Neurobehavioral Difficulties Poor self-regulation of behavior Impulsivity, Disinhibition, Judgment Perseveration Inappropriate behavior Child-like demeanor or response Flat affect and/or emotional lability Reduced awareness of deficits Lack of empathy for others Temporal Lobe Impairments: Neurocognitive Memory - Verbal and/or Spatial Immediate or Working Memory OK Old, Well-Learned Memory OK Storage of New Memories Impaired Short Term Memory Badly Affected Reduced New Long Term Learning Reduced Prospective Memory Skills Temporal Lobe Impairments: Neurocognitive - 2 Auditory Processing Reduced Language Comprehension Changes in Melodic Processing Changes in Prosody Problems with Visual Item Recognition Misperception of Interpersonal Events Temporal Lobe Impairments: Neurobehavioral Heightened Irritability Rage reactions (Limbic dyscontrol) Interpersonal “viscosity” Parietal Lobe Deficits: Sensory-Perceptual Changes in sensation and perception of: Touch Pain Temperature Position and Location, on body and in space Vibration Integration of sensory perceptual information (agnosias) Parietal Lobe Deficits: Further disturbances Apraxia - inability to perform skilled movements in the abstract Difficulty apprehending the Gestalt Visual field disturbances Neglect Paranoia or misperception of people and events Parietal Lobe: Specific Neurocognitive Problems Visual perception - lines and angles Facial perception Mechanical skills - visual and tactual Path-finding, Interpretation of maps, directions Difficulty with reading Difficulty with writing Occipital Lobes Primary visual cortex Elaboration of visual information Synthesis of visual information Visual field defects Abundant connections with other regions of the brain - role in reading, executive functions, visual memory Brain stem and Cerebellum Cranial nerves damaged Spasticity, dysarthria, dysphagia Balance, coordination, gait Motor learning Cerebellar affective sydrome Role of Neuropsychological Evaluation Evaluations designed to identify brain-related abilities and deficits in higher level functions Can winnow through many domains of function and identify main concerns Provides good pre-injury history Look at current levels of emotional distress and coping abilities Identifies personality strengths and vulnerabilities that can affect outcome Can help outline effective treatment plan Neuropsychological Evaluation: The Process Referral Question Record Review Interview with Patient and Family Test Selection and Administration Behavioral Observations Test Scores and Normative Data Analysis and Integration of All Results Review of Results Report with Findings, Recommendations Neuropsychological Evaluation: The Content Intellectual skills: verbal and nonverbal Attention: simple and complex Memory - verbal, spatial, simple, complex Acquisition, Retention, Retrieval, Recognition Language and Academic abilities Visual spatial and tactual spatial processing Executive functions Sensory Perceptual abilities Fine motor speed Current emotional status, ability to engage tx Neuropsychologically-Based Treatment Plans What are the primary obstacles to improved function? Cognitive and communication issues Behavioral disturbances (neurologic) Speed of thinking and performance Reactive emotional problems Physical limitations Personality difficulties (characterologic) Lack of family and social support Disincentives to return to productivity Other risk factors Neuropsychologically-based treatment plans: What are the person’s major strengths? Pre-injury experiences that developed cognitive, emotional, interpersonal, artistic, musical, athletic, vocational, behavioral, common-sense, good judgment or skill-based abilities Any special talents or interest? Pilot? Carpenter? Residual abilities in any or all of the above areas Personal ability to rally coping resources Features of personality strengths Degree and nature of family support Friends and other supports, including pets “Blended” Case Example 20 year old single male High school educated In college at time of accident Severe traumatic brain injury in MVA 2-week coma - 9 months post-injury Classic frontal-temporal injury Very mild residual right hemiparesis Cognitive Rehab Targets: Attention: vulnerable to distraction Memory: spontaneous retrieval Executive functions: plan, organize, time management Speed of thinking mildly reduced Reading comprehension Missing the main idea Not taking effective notes Treatment Plan: Residual Strengths Good pre-morbid school and work history Good basic reasoning skills Strong desire to return to school Able to withstand constructive feedback New learning ability present Willing to participate in treatment Supportive family Laying the groundwork for treatment success Updated Rehab MD review of injury related health concerns and meds Re-establish good sleep-wake cycle Trazadone for sleep was helpful Re-establish decent nutrition Reduce alcohol consumption Review and update exercise regimen Secure or modify basic living situation Three key places to begin for this patient: Find and use a single effective memory compensatory device Establish a routine schedule Start work on ways to reduce distraction Find and use a single memory system: Some trial and error to find right system The memory system has to be with the person at all times and used every day, multiple times for entries and review Choose a single calendar or device that the person likes and is willing to use iPhone calendar that syncs to Google? Daytimer or Week at a Glance systems? Small pocket calendar? Watch with calendar and alarms? Establish a predictable schedule with a set of routines Evening routine: Check appt book for next day’s schedule Gather items needed for next day’s departure and place them by door to garage or bus Plan route and double estimated time needed Have wallet, cell phone, keys in one place Put out clothes you will wear tomorrow Start quiet time at 9:30pm: relax, light reading, meditation, quiet music, snuggle time with pets No TV, no computer, no thrilling movies, no late exercise Check to make sure alarm is set; in bed by 10pm Morning routine Morning routines Get up when alarm goes off - no snooze! Reward yourself with coffee, tea, or juice Shower and dress Re-check the day’s schedule and to do list Have breakfast, take meds if appropriate Check that burners and lights are off Make sure you have all you need to take with you, e.g., wallet, phone, keys, books, backpack, laptop, money for meals at school Key elements of daytime routine Follow established schedule Class days and times mapped out for term Therapy appts: Time, place, person Bring therapy notebook and school homework Study time scheduled for homework and tests Extra time scheduled for projects and papers Break times and meal times scheduled Exercise or gym time Open time to relax, visit with friends, have fun Bring future assignments and graded papers or tests to speech treatment for review Methods to reduce distraction External distractions Find quiet place to study Turn off phone, TV, music, radio If study materials are on-line,consider printed copies to allow single-minded focus on article, and avoid “pop-ups” or “dings” alerting you to incoming email or messages Read aloud to maintain focus on material Underline what you think is important to know Take brief breaks every 30 minutes after jotting down some of those main ideas Internal distractions What is it that keeps popping into mind? Worries Something you don’t want to forget? Quickly jot it down in memory system at hand Are you hungry or thirsty? Are you sleepy? Jot it down for consideration at a scheduled “worry time review” later Have some coffee, do 10 minutes of exercise What is your optimal time of day for focus? Use of ABODES system for planning and organizing - “A” Assess the situation What is it you want to do? When? Where? With whom? How? Why? Use of ABODES Break the task, goal, project or activity into as many possible steps as you can brainstorm The more steps, the better Even if you are not sure a step is needed, better to include it than not to list it Order the steps from first to last as they would most likely need to be accomplished First break the long list of steps into smaller subgroups that have something in common Then go back and put the steps within each of the subgroups in order Use of ABODES Decide what is needed to accomplish the task, goal, project or activity Materials, supplies, tools or information Reservations, tickets, visas, appointments Money, credit card, debit card, photo ID Space in which to work or gather Help or participation by others A certain kind of weather or time of year? Use of ABODES Estimate time it will take to accomplish the task, goal, project or activity Estimate the time you think is needed to complete each of the specific steps you listed Add in any time needed for coordination with others Triple the time estimated to complete each step Enter each of the steps, in order, into your schedule system on specific dates and times to begin accomplishing them Use of ABODES Survey your work and re-adjust project needs and time frame for completion None of us has perfect ability to plan and implement an entire project without some changes you’ll only learn are needed once you’ve begun! Do not tackle massive organizational projects alone or with limited time, space and resources, unless you know: It can be completed in one day (organizing your spices) You can leave the not-yet-completed steps in reasonably neat order so your overall situation is not worsened Reading Comprehension Getting the main ideas What is the title of the chapter, story or article? Read a paragraph and see if you can put the main point into your own words Is the story about a person, place, thing or idea? Sometimes the first and last line of each paragraph will introduce or summarize main points Are certain nouns (people, places, objects, concepts) mentioned frequently in the paragraphs? Is there something new that you learned by reading the story? Can you go jot down a few main points and details? Taking effective notes For reading comprehension & retention Correct any visual problems as much as possible Use good lighting by which to read Keep a list of main characters and events for books you read on a 4 x 6 card in book Write a brief summary of each chapter’s main people, events or ideas Participate in a study group or book group to discuss main ideas and characters and events Read aloud for multi-sensory input See, say, hear, listen Taking effective notes while listening in classroom Make sure your hearing is okay Sit at front of lecture space Use an outline form to capture main ideas and key details If handouts, slides or outlines are available on-line prior to lecture, review those Review your notes immediately after lecture and try to fill-in or clarify as you can Borrow notes from good note-takers Digitally record lectures and review them Taking effective notes in class You don’t have to jot down everything Try to alternate your listening and writing, so there are times when you are fully focused on the speaker, and not writing Ask occasional questions of the speaker to clarify what has been said Write as good a summary note as possible at the end of the presentation or discussion Final comments on Cognitive Rehabilitation An essential component is the mind of the therapist who understands the underlying causes of cognitive problems and can create, implement, monitor and modify treatment as appropriate. This occurs as part of a larger informed and compassionate view of human needs, limitations, strengths and behaviors. The person with TBI must ally him or herself with the treatment effort, personnel and goals