Clinical Process Analysis Ambulatory Operations Project
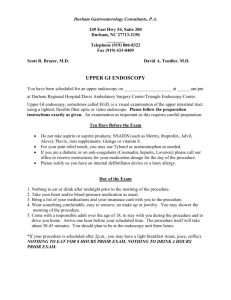
advertisement

Clinical Process Analysis Ambulatory Operations Project: Endoscopy Center Summary April 6, 2013 STAFF Laurie Kaufman MSN, RN Manager Gina Aranzamendez MS, RN-BC Courtney Barnes MBA Beverly Hayes Valerie Haywood MBA, BSN, RN Duke Rohe, IE Marvetta Walker, MHA, RN Manager Endoscopy Time Driven Activity Based Costing (TDABC) • Harvard University Business School – Michael Porter, PhD – Robert Kaplan, PhD • Institute for Cancer Care Excellence (ICCE) – Thomas Feeley, MD – Heidi Albright, Director – Head & Neck Center Pilot • Office of Performance Improvement – Process Flow Charting TDABC & Clinical Process Analysis MDACC’s Framework for Improving As A System Based on W. Edwards Deming’s “Profound Knowledge” Adapted From: A Framework for the Continual Improvement of Health Care. Batalden PB. Journal of Quality Improvement Vol 19 No. 10 1993 2. HOW WE IMPROVE WHAT WE DO Vision: Making Cancer History Design and Redesign Plans to Improve Our: • • • • • • • • • • • • 1. 2. 3. 4. Performance as a System Knowledge of Variation Use of the Theory of Knowledge Application of Psychology Patients Families Staff Suppliers Equipment Supplies Partners Etc. I N P U T S 1. WHY WE DO WHAT WE DO To Cure Cancer To Provide Patient Care To Develop Our Workforce To Maintain Financial Viability Processes that produce: Research Patient Care Work Force Development Financial Viability 3. HOW WE PERFORM OUR SERVICES O U T P U T S Outcomes Costs = Value 4. WHAT WE DELIVER Clinical Process Analysis Program Aim: Create a comprehensive visual display of current work processes for analysis to drive improvement in clinical quality & financial performance. Why do this? How to do this? • Create a shared sense of the future • Align with strategic goals • Develop clearly defined aim and scope • Engage all levels of leadership support • Avoid competing priorities w/optimal scheduling in roll-out • Create two-way communication • Instill psychological safety for staff to share current processes • Mobilize clinicians to make changes needed for healthcare (Berwick, 2011) • Capture the voice of the patient (Institute of Healthcare Improvement) • Illustrate frontline reality (James, 2012) • Align data reporting to frontline processes (James, 2012) The Process INPUTS PHASE I PHASE II Current Work Activities Clinical Leadership Content Experts Clinical Process Analysis Team Precursory Work Weekly Interviews PHASE III Summary & Evaluation OUTPUTS Process Flow Charts In-sync Data Reporting Direct Labor Costs Opportunities for Improvement Embed QI Knowledge Performance Improvement Phase Workforce Engagement PI Projects CPA Methodology Process Flow Chart, Direct Labor Cost & Opportunities for Improvement Performance Improvement Phase Weeks 4 - 14 Participants: • Clinical Lead: Designated clinical point person for the project • Clinical Leadership: Clinical Administrative Director; Center Business Manager; Nurse Manager; Medical Director; Quality Officer • Content Experts: Frontline staff • CPA Team: Clinical Process Analysis Team, Performance Improvement • SOT: Senior Operations Team • Center Process Flow Charter: Maintains process flow charts for the Center after CPA Project is completed The Office of Performance Improvement, © 2012 The University of Texas MD Anderson Cancer Center Background: Endoscopy Center Project • Center Variation • Scope Development The Office of Performance Improvement, © 2012 The University of Texas MD Anderson Cancer Center The Office of Performance Improvement, © 2012 The University of Texas MD Anderson Cancer Center The Office of Performance Improvement, © 2012 The University of Texas MD Anderson Cancer Center The Office of Performance Improvement, © 2012 The University of Texas MD Anderson Cancer Center Process Flow Charts Aligning Data to Frontline Processes & Elements of a Process Flow Chart Direct Labor Cost Process Flow Chart converted to Excel for Direct Labor Costing Costing • Salaries based on FY 2012 from ResourceOne • Data based on information captured in process flow charts from 10.17.2012 – 12.12.12 • Based on estimated times given by frontline staff in the Endoscopy Center • Salaries in this report are average adjusted hourly rates including fringe • Salaries for each Job Code Group are blended by utilizing FTEs to weight the averages: • MD- Professor, Associate Professor, Assistant Professor • PSC- Lead Services Coord, Patient Services Coord • MLP- APN and APN supervisor • Data is reported per patient Costing Summary: Direct Labor Costs Costing Summary: Estimated Times in Minutes OFIs (Opportunities for Improvement) Waste, Delays, Inconsistencies, Rework… Phase II Week 4 Precursory Work Meet with CAD: validate OFI Categories, Control level, & Prioritize Phase II Week 5 to 8 Precursory Work PI Week 1 PI Week 2 PI Week3 PI Week 4 PI Week 5 PI Week 6 Summary Meeting Staff (2) assigned to OFIs complete PDSA 101 Quick Fix 1 (scope: 1 wk turnaround) 4hr/staff member Quick Fix 2 (scope: 1 wk turnaround) 4hr/staff member PDSA Mtg 1 Aim Statement/ Baseline Measure 4hr/staff member PDSA Mtg 2 Cause Analysis/ Intervention 4hr/staff member PDSA Mtg 3 Implementation/ Post Measure 4hr/staff member PDSA Mtg 4 Document/ Presentation prep 4hr/staff member Staff present OFI improvements at Summary Mtg SharePoint Site for Project Storage • Provides storage for project work-ups • Available for bench-marking • Easy placement in Quality Project database OFI Summary • Total OFIs: 53 • OFIs in department's control: 6 • OFIs out of department's control: 14 • OFIs within department's influence: 33 OFI Projects 6 Quick Fixes 8 PDSA 1 CS&E 1. Ready Call pagers 2. Consult processing/patient check-in 3. Optimization of Endoscopy Online Consult Health questionnaire 4. Bedside consenting 5. Nurse sedation practices 6. Guidelines for scheduling an Endoscopy procedure 7. Physician notification process for patient cancellation or reschedule OFI Projects 8. iConsent 9. PYXIS medication availability 10. Anesthesia sedation & recovery charge reconciliation 11. Endoscopy safety procedure checklist 12. Room standardization