Diabetic foot_01 (Evaluation)
advertisement

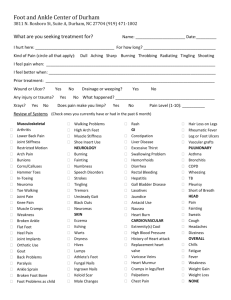
Diabetic foot (Evaluation) INTRODUCTION 1. 2. Foot problems are important cause of morbidity in patients with DM. The lifetime risk of foot ulcer for diabetic patients (type 1 or 2) may be as high as 25%. A potentially preventable initiating event, most often minor trauma that causes cutaneous injury, can often be identified. Foot amputations, many of which are preventable with early recognition and therapy, may be required. These observations illustrate importance of frequent evaluation of feet in patients with DM to identify those at risk for foot ulceration. Systematic screening examinations for neuropathic and vascular involvement of lower extremities and careful inspection of feet may substantially reduce morbidity from foot problems. Evaluation of diabetic foot is provided here. A discussion of DM-related foot infections (cellulitis and osteomyelitis) and management of diabetic foot ulcers are found elsewhere. RISK FACTOR 1. Several risk factors are predictive of ulcers and amputation. Early recognition and management of risk factors is important for reducing morbidity of foot ulceration. Most risk factors are readily identifiable from Hx or PE. The most important are previous foot ulceration, neuropathy (loss of protective sensation), foot deformity, and vascular disease. The significance of these risk factors was confirmed by results of community-based study of 1300 T2DM patients. The incidence of lower extremity amputation was 3.8 per 1000 patient-years. Predictors of amputation were foot ulceration (HR 5.6), ABI < 0.9, elevated HbA1C, and neuropathy. 2. 3. Neuropathy is present in > 80% of patients with foot ulcers; it promotes ulcer formation by decreasing pain sensation and perception of pressure, by causing muscle imbalance that can lead to anatomic deformities, and by impairing microcirculation and integrity of skin. Once ulcers form, healing may be delayed or difficult to achieve, particularly if infection penetrates to deep tissues and bone and/or there is diminished local blood flow. Risk classification A. There is several risk classification systems designed to predict foot ulcer in patients with diabetes. Risk categorization can be used to design preventive and monitoring strategies (table 1). One system, developed by IWGDF, stratifies patients as follows. i. Group 0 - no evidence of neuropathy ii. Group 1 - neuropathy present but no evidence of foot deformity or peripheral vascular disease iii. Group 2 - neuropathy with evidence of deformity or PAOD iv. Group 3 - history of foot ulceration or lower extremity amputation B. In prospective case-control study of 225 patients with DM, stratification using this classification system was predictive of incident ulceration and amputation. During 30 months (mean) of follow-up, ulcers occurred in 5, 14, 13, and 65% of patients in groups 0, 1, 2, and 3. Only patients in groups 2 and 3 had amputations (2 and 26%). HISTORY 1. An abbreviated history combined with PE can usually establish presence and severity of 2. 3. diabetic neuropathy and PAOD, 2 of the most important risk factors for developing foot ulcer. Historical fact to ascertain include duration of DM, glycemic control, presence of micro- or macrovascular disease, history of prior foot ulcers, lower limb bypasses or amputation, presence of claudication, and history of smoking. Two cohort studies have demonstrated increased risk of foot ulcers in those with longer history of DM. This may be related to finding that risk of PAOD appears to increase with duration of T2DM. As example, in observational study of 48,607 men, RR of PAOD in patients with T2DM compared with non-DM was 1.4 and 4.5 for 1 to 5 years and > 25 years of DM, even after controlling for other CV risk factors. Peripheral neuropathy also increases with longer diabetes duration. The patient should be questioned about leg discomfort. If present, further questions should be asked that allow quantitative assessment of symptoms. A. What is sensation felt? — Burning, numbness, or tingling (2 points); fatigue, cramping, or aching (1 point). Maximum is 2 points. B. What is location of symptoms? — Feet (2 points); calves (1 point); elsewhere (no points). Maximum is 2 points. C. Have symptoms ever awoken you at night? — Yes (1 point). D. What is timing of symptoms? — Worse at night (2 points); present day and night (1 point); present only during the day (no points). Maximum is 2 points. E. How are symptoms relieved? — Walking around (2 points); standing (1 point); sitting or lying or no relief (no points). Maximum is 2 points. 4. The total symptom score can then be determined. A. 0 to 2 — Normal B. 3 to 4 — Mild C. 5 to 6 — Moderate D. 7 to 9 — Severe PHYSICAL EXAMINATION 1. PE should include assessment for presence of existing ulcers, peripheral neuropathy, PAOD, and foot deformities that may predispose patient to development of foot ulcers (table 2). Several reports indicate that adequate examinations relevant to foot ulceration are often not performed in DM patients. A. When 1434 clinicians in the US were surveyed about how closely they were adhering to nationally promoted and ADA endorsed recommendations for routine care, only 50% did semiannual neurologic and foot examinations. B. In major California HMO that provides care for 14,539 DM patients, only 6% had documented foot examination within previous year. 2. Physical signs of neuropathy A. Neuropathy is present in over 80% of patients with foot ulcers; it promotes ulcer B. formation by decreasing pain sensation and perception of pressure by causing muscle imbalance that can lead to anatomic deformities, and by impairing microcirculation and integrity of skin. PE may reveal several abnormalities that result from diabetic neuropathy, such as claw toes and Charcot arthropathy (also called diabetic neuropathic arthropathy). Chronic motor neuropathy often affects small intrinsic muscles of feet so that action of larger muscles in anterior tibial compartment is unopposed. This leads to subluxation of proximal interphalangeal-metatarsal joints, resulting in claw toe appearance. One consequence of this abnormality is increased pressure on metatarsal heads, which are common site of ulcer development. C. D. 3. A later complication is Charcot arthropathy, which is characterized by collapse of arch of mid-foot and abnormal bony prominences. These changes are induced by triad of small muscle wasting, decreased sensation, and abnormal distribution of weight when standing. The associated autonomic neuropathy can lead to several additional problems. Sweating is diminished or absent; as result, skin of feet remains dry and has tendency to become scaly and cracked, thereby allowing infection to penetrate below skin. Lack of autonomic tone in capillary circulation causes shunting of blood from arteries directly into veins, bypassing tissues that need nutrition. This results in foot that feels warm and has distended veins and bounding pulses. Despite these apparent signs of adequate perfusion, foot is vulnerable to local "microvascular" gangrene, will heal very poorly and slowly, and will be less able to resist infection. Screening test for peripheral neuropathy A. In clinical practice, peripheral neuropathy is most frequently assessed by determination. i. Vibration sensation ii. Pressure sensation (monofilament) iii. Superficial pain (pinprick) or temperature sensation B. The tests are designed to identify LOPS, important risk factor for ulcer formation. Screening with simple vibration testing, monofilament examination, or superficial pain sensation appear to have similar sensitivity and specificity for predicting diabetic neuropathy and therefore risk of foot ulcer. One study found that failure to detect pressure from monofilament at any of 12 places on foot was single most practical measurement of risk assessment. C. Vibration sensation i. Vibration testing is typically conducted with 128-Hz tuning fork applied to bony prominence at dorsum of first toe, just proximal to nail bed. The quickest method of testing is to ask patient to report perception of both start of vibration sensation the cessation of vibration on dampening. The test should be conducted twice on ii. iii. each great toe. The sensitivity and specificity of vibration testing for peripheral neuropathy have been estimated to be 53 and 99%. Vibration sense can also be estimated quantitatively with Biothesiometer (Bio-Medical Instrument Company). This device is essentially electronic tuning fork that allows vibration to be adjusted up or down depending upon voltage applied. The vibration-perception threshold (VPT) is defined as the lowest voltage at which vibration can be sensed on pulp of big toe. The value in normal subjects increases with age from approximately 6 volts at age 30 years to 20 volts at age 75 years. In prospective trial of 469 diabetic patients with no history of foot ulceration, VPT was found to be excellent predictor of future foot ulceration. < 4% of patients with VPT < 25 volts developed new ulcers vs. almost 20% of those with VPT > 25 volts. Furthermore, there was excellent correlation between VPT and severity of findings on PE. A simpler alternative to the Biothesiometer is the graduated tuning fork, which can also provide quantitative estimate of vibration sense. D. Pressure sensation i. Another simple device, monofilament pressure esthesiometer, permits quantitative ii. 4. assessment of cutaneous pressure perception threshold. The 5.07 (10-g) monofilament is placed at right angle to skin on plantar surface of foot; pressure is then increased until filament buckles, indicating that known amount of pressure has been applied. The patient is asked if he or she felt pressure induced by monofilament. In cross-sectional study of 314 diabetic patients, those with foot ulcers had higher pressure threshold than those without ulcers. A cutaneous pressure threshold of 4.21 U or above had sensitivity of 84%, specificity of 96%, and PPV of 76% for foot ulceration. Prospective studies have shown that insensitivity to this monofilament correlates with increased likelihood for developing plantar ulceration or lower extremity amputation in future. E. Pain and temperature sense i. Either pain or temperature sense can be tested; it is not necessary to evaluate both. Physical sign of PAOD A. The feet should be examined for signs of PAOD such as absence of foot pulse, decrease in skin temperature, thin skin, lack of skin hair, and bluish skin color. However, these signs are neither sensitive nor specific enough to be helpful in individual patient. More useful tests are examination of lower limb pulses and measurement of venous filling time. The absence of pedal pulses, presence of femoral bruits, or prolongation of venous B. C. D. filling should prompt referral for more detailed evaluation. The venous filling time can be determined by identifying prominent pedal vein with patient in supine position. The leg is elevated to 45º for 1 minute, leading to collapse of vein. The patient then sits up and hangs leg over examination table; important arterial disease is probably present if > 20 seconds elapse before vein bulges above skin. Patients with clinical evidence of PAOD should have ABI. This index is calculated by measuring SBP in brachial, posterior tibial, and dorsalis pedis arteries. The highest of four measurements in ankles and feet is divided by higher of 2 brachial measurement. The normal index is > 1.0, because pressure is higher in ankle than in arm. An index < 0.9 has 95% sensitivity for detecting angiogram-positive PAOD. We typically refer patients with abnormal ABI to vascular specialist. A low index in absence of foot ulcer does not correlate with risk of future foot ulceration; however, low index in presence of foot ulcer suggests that prognosis will be improved with reconstructive vascular surgery. In one series of patients with neuropathic foot ulcers and severe arterial insufficiency, for example, 35 of 42 extremities (83%) with patent bypass grafts achieved and maintained primary healing of their ulcer. A low index also indicates more generalized arteriosclerosis and is associated with increased risk of CV death. 5. Foot ulceration A. Foot ulcers are usually classified into two groups: acute ulcers secondary to dermal abrasion from poorly fitting shoes and chronic plantar ulcers occurring over weight-bearing areas. Chronic ulceration is probably multifactorial, due to combination of diabetic neuropathy (with decreased pain sensation), autonomic dysfunction, and vascular insufficiency. B. Findings that may herald developing foot ulcer include following. i. Lesions between adjacent toes due to pressure from tight shoes cramming them together ii. Macerated areas between toes ("athlete's foot"); these lesions are often painless and may go unnoticed until bacterial infection supervenes iii. Bunions (callused areas) C. Wound evaluation i. The evaluation of existing diabetic foot ulcer includes careful examination and classification of wound. The ulcer is observed for drainage, odor, presence (or absence) of granulation tissue, and any exposed underlying structures, such as tendons, joint capsule, or bone. The wound can be probed gently by experienced clinician or surgeon with sterile, blunt probe to reveal presence of sinus track or communication with deeper structures, which may change wound classification. D. Sign of infection i. The presence of diabetic foot infection is usually presumed if these conditions are present. 1. At least two of following: erythema, warmth, tenderness, or swelling OR 2. Pus coming out of ulcer site and/or nearby sinus tract ii. Osteomyelitis is likely to be present if bone can be seen at floor of deep ulcer, or if it can be easily detected by probing ulcer with sterile, blunt, stainless steel probe. Other signs that suggest osteomyelitis are ulcer size > 2 x 2 cm and otherwise unexplained elevation in ESR. iii. A discussion of diabetes-related foot infections (infected ulcer, cellulitis, and osteomyelitis) is found elsewhere. E. Imaging i. Plain radiographs can detect structural foot deformities, soft tissue gas, foreign bodies, and may be able to detect osteomyelitis. However, radiologic changes occur late in course of osteomyelitis and negative radiographs do not exclude it. Other imaging techniques that have been used include radionuclide bone imaging, MRI, and imaging with indium-labeled leukocytes. F. Wound classification i. Diabetic foot ulcers can be graded according to scheme, such as that proposed by Wagner. 1. Grade 0 — No ulcer in high risk foot 2. Grade 1 — Superficial ulcer involving full skin thickness but not underlying tissues 3. Grade 2 — Deep ulcer, penetrating down to ligaments and muscle, but no bone involvement or abscess formation 4. Grade 3 — Deep ulcer with cellulitis or abscess formation, often with osteomyelitis 5. Grade 4 — Localized gangrene ii. 6. Grade 5 — Extensive gangrene involving whole foot Wound classification is reviewed in more detail separately. SCREENING FOR RISK OF FOOT ULCERATION 1. A meta-analysis of 16 case-control or cohort studies found that the following diagnostic screening tests reliably identified those at risk for foot ulceration. A. Peak plantar pressure (requires special equipment to identify specific areas of high pressure under the foot) B. Vibration perception with tuning fork or Biothesiometer C. Cutaneous sensation with monofilament 2. PE findings of absent ankle reflexes and limited joint motion at both first 3. metatarsal-phalangeal joint and subtalar joint also increased risk of future foot ulcers, as did patient history of previous amputation, ulceration or lower limb bypass procedures. Other physical examination findings, such as absence of pedal pulses and ABI, were less reliable predictors of foot ulcers. In another report, conventional clinical examination had low reproducibility compared with examination using monofilament, and the latter was recommended for screening diabetic patients for neuropathy. 4. 5. We suggest that all patients with diabetes be screened annually to identify those at risk for foot ulceration. We perform Hx, PE of foot, and use 5.07 U monofilament for screening purposes. As alternative or in addition to monofilament, vibration testing, ankle reflex assessment, or tests of pinprick sensation can be used to identify LOPS. Preventive foot care A. In conjunction with screening, counseling regarding preventive foot care should be given to any patient whose feet are at risk. There are a series of recommendations that can markedly diminish ulcer formation; they are particularly important in patients with existing neuropathy. i. Avoid smoking, walking barefoot, use of heating pads or hot water bottles, and stepping into bath without checking the temperature. ii. iii. iv. The toenails should be trimmed to shape of toe and filed to remove sharp edges. The feet should be inspected daily, looking between and underneath toes and at pressure areas for skin breaks, blisters, swelling, or redness. The patient may need to use mirror or, if vision is impaired, have someone else perform examination. The patient's shoes should fit properly and not be too tight, and the socks should be cotton, loose fitting, and changed every day. Patients who have misshapen feet or have had a previous foot ulcer may benefit from the use of special customized shoes. A prospective study found that shoe variables other than the recommendation for customized shoes (style, width, length, or type of shoe) had no preventive effect. The use of customized shoes, however, reduced the development of new foot ulcers from 58 to 28% over one year of follow-up in second report. In third review, use of viscoelastic insole in conjunction with well-fitting shoes (whether customized, standard "comfort" or athletic shoes) was associated with decrease in plantar pressure; whether this results in reduced incidence of foot ulcers remains to be determined. v. The feet should be washed daily in lukewarm water. Mild soap should be used and feet should be dried by gentle patting. A moisturizing cream or lotion should then be applied. B. A particularly effective strategy is to make specific recommendations to the patient in the form of "contract" and to advise patient to request that his or her feet be examined C. at every visit to doctor or nurse. In addition to foot care measures described above, preliminary data suggest that home temperature monitoring may be effective in preventing foot ulceration in very high risk patients (for example, those with severe neuropathy and history of prior amputations or ulcers). Temperature monitoring involves daily or twice daily measurements of skin surface temperature with thermometer equipped with touch sensor. If temperature difference (elevation) is detected between right and left foot site, patients are instructed to reduce activity until temperature normalizes. D. 6. Whether benefit of monitoring temperature is specifically related to monitoring, or heightened attention to foot care in those performing the monitoring, is not clear. Additional efficacy and feasibility studies are required before home temperature monitoring can be recommended to reduce risk of foot ulcers. Guideline A. Perform comprehensive foot examination annually on patients with diabetes to identify risk factors predictive of ulcers and amputation. Perform visual inspection of feet at each routine visit. B. The comprehensive foot examination can be accomplished in primary care setting and should include inspection of skin for integrity, especially between toes and under metatarsal heads. The presence of erythema, warmth, or callus formation may indicate C. D. E. areas of tissue damage. Bony deformities, joint mobility, and gait and balance should also be assessed. Test for loss of protective sensation using Semmes-Weinstein 5.07 (10-g) monofilament at specific sites to detect loss of sensation in foot, plus any one of the following: vibration using 128-Hz tuning fork, pinprick sensation, ankle reflexes, or vibration perception threshold with biothesiometer. Screen for PAOD by asking about history of claudication and assessing pedal pulses. Obtain ABI in patients > 50 and consider measurement in younger patients with multiple risk factors for PAOD, as many patients with PAOD are asymptomatic. Advice for prophylactic foot care should be given to all patients. F. Refer high risk patients (those with any positive findings from the comprehensive examination) to foot care specialist. SUMMARY AND RECOMMENDATIONS 1. Screening — Foot ulcers are an important cause of morbidity in patients with diabetes. Both vascular and neurologic disease increase the risk of foot ulcers. A. We suggest that all patients with diabetes be screened annually to identify those at risk for foot ulceration. B. We perform a history, comprehensive foot examination, and test for loss of protective sensation using Semmes-Weinstein 5.07 (10-g) monofilament for screening purposes. C. We perform ankle-brachial pressure index (ABI) testing in any patient with symptoms or 2. physical exam findings of peripheral artery disease. D. Counseling regarding preventive foot care should be given to any patient whose feet are at risk for ulceration. High risk for future ulcer — We refer patients to foot care specialist if they are at particularly high risk for foot ulceration due to the following risk factors. A. A previous history of foot ulceration or amputation B. Loss of protective sensation and/or neuropathic foot deformities C. Peripheral vascular disease