Human Infection with a Novel Avian
advertisement

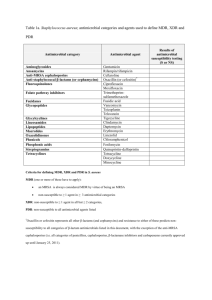
Global Action Plan to combat antimicrobial resistance | Antimicrobial Resistance Global Report on Surveillance 2014 Patients with pneumonia and bacteria in the blood Penicillin increased the chance of survi val from 10% to 90 % Adapted from Austrian et al. Ann Int. Med 1964; 60, 759 | .Antimicrobial Resistance Global Report on Surveillance 2014 % survivors Penicillin Untreated Days The more we use them, the more we lose them From Albrich et al EID 2004 | Antimicrobial Resistance Global Report on Surveillance 2014 Diseases that should be treatable now more likely to kill | Antimicrobial Resistance Global Report on Surveillance 2014 Impact on mutliple sectors of health care Infectious disease Medical Procedures Pneumonia Neonatal care Gonorrhea Transplantation Enteric infections Cancer treatment Blood infections Surgery etc. etc. | Antimicrobial Resistance Global Report on Surveillance 2014 Why now? Increasingly serious global public health threat – New evidence and information – Desperation over "dry pipeline" Economic impact – World Economic Forum 2013 Global Risk Report Growing awareness and commitment – Political, professional, public | Antimicrobial Resistance Global Report on Surveillance 2014 | Antimicrobial Resistance Global Report on Surveillance 2014 Antimicrobial Resistance Global Report on Surveillance 2014 (I) • Focuses on antibacterial resistance (ABR) • Information gathered include: Surveillance of ABR according to WHO regions National and published data on 7 bacteria | Antimicrobial Resistance Global Report on Surveillance 2014 Systematic reviews of evidence of health and economic burden in 5 bacteria/ resistance combinations Identification of gaps Selected Bacteria/Resistance Combinations Bacterium Resistance/ decreased susceptibility to: Escherichia coli 3rd generation cephalosporins, fluoroquinolones Klebsiella pneumoniae 3rd generation cephalosporins, carbapenems Staphylococcus aureus Methicillin (beta-lactam antibiotics) i.e. MRSA Streptococcus pneumoniae Penicillin Nontyphoidal Salmonella (NTS) Fluoroquinolones Shigella species Fluoroquinolones Neisseria gonorrhoeae 3rd generation cephalosporins | Antimicrobial Resistance Global Report on Surveillance 2014 Available National Data* on Resistance for Nine Selected Bacteria/Antibacterial Drug Combinations, 2013 *National data means data obtained from official sources, but not that data necessarily are representative for the population or country as a whole Bacteria Commonly Causing Infections in Hospitals and Communities Name of bacterium/ resistance No. of 194 MS providing national data No. of WHO regions with national reports of 50 % resistance or more Range of reported proportion of resistance -vs 3rd gen. cephalosporins 84 5/6 0-82 -vs fluoroquinolones 90 5/6 3-96 -vs 3rd gen. cephalosporins 85 6/6 2-82 -vs carbapenems 69 2/6 0-68 83 5/6 0.3-90 Escherichia coli Klebsiella pneumoniae Staphylococcus aureus Examples of typical diseases Urinary tract infections, blood stream infections Pneumonia, blood stream infections, urinary tract infections Wound infections, blood stream infections -vs methicillin “MRSA” | Antimicrobial Resistance Global Report on Surveillance 2014 Bacteria Mainly Causing Infections in the Community Name of bacterium/ resistance Streptococcus pneumoniae Examples of typical diseases 66 6/6 0-73 66 3/6 0-96 34 2/6 0-47 42 3/6 0-36 Diarrhoea (“bacillary dysenteria”) - vs fluoroquinolones Neisseria gonorrhoeae Range of reported proportion of resistance Foodborne diarrhoea, blood stream infections -vs fluoroquinolones Shigella species No. of WHO regions with national reports of 25 % resistance or more Pneumonia, meningitis, otitis -non-susceptible to penicillin Nontyphoidal Salmonella No. of 194 MS providing national data Gonorrhoea -vs 3rd gen. cephalosporins | Antimicrobial Resistance Global Report on Surveillance 2014 Systemic Reviews: Evidence of the Burden of Antibacterial Resistance Is there any difference in outcome from infections caused by resistant vs sensitive bacteria? | Antimicrobial Resistance Global Report on Surveillance 2014 Risk of Death is Higher in Patients Infected with Resistant Strains Deaths (%) Outcome (number of studies included) Resistant Not resistant RR (95% CI) 2.02 (1.41 to 2.90) Escherichia coli resistant to: 3rd gen. cephalosporins Bacterium attributable mortality (n=4) 23.6 12.6 Fluoroquinolones Bacterium attributable mortality (n=1) 0 0 Klebsiella pneumoniae resistant to: 3rd gen. cephalosporins Bacterium attributable mortality (n=4) 20 10.1 1.93 (1.13 to 3.31) Carbapenems Bacterium attributable mortality (n=1) 27 13.6 1.98 (0.61 to 6.43) 26.3 16.9 1.64 (1.43 to 1.87) Staphylococcus aureus resistant to: Methicillin (MRSA) Bacterium attributable mortality (n=46) | Antimicrobial Resistance Global Report on Surveillance 2014 Estimates of Burden of Antibacterial Resistance European Union Thailand United States population 500m population 70m population 300m 25,000 deaths per year >38,000 deaths >23,000 deaths 2.5m extra hospital days >3.2m hospital days >2.0m illnesses Overall societal costs (€ 900 million, hosp. days) Approx. €1.5 billion per year Overall societal costs US$ 84.6–202.8 mill. direct >US$1.3 billion indirect Overall societal costs Up to $20 billion direct Up to $35 billion indirect Source: ECDC 2007 Source: Pumart et al 2012 Source: US CDC 2013 Global information is insufficient to show complete disease burden impact and costs | Antimicrobial Resistance Global Report on Surveillance 2014 Summary: Antibacterial Resistance 1. High proportions of resistance were reported in all regions to common treatments for bacteria causing infections in both healthcare settings and in the community 2. Antibacterial resistance has a negative effect on patient outcomes and health expenditures 3. Treatment options for common infections are running out 4. Despite limitations, the report demonstrates worldwide magnitude of ABR and surveillance gaps | Antimicrobial Resistance Global Report on Surveillance 2014 Resolution on AMR World health Assembly May 2014 ... To develop a draft global action plan to combat AMR ... to ensure that all countries ... have the capacity to combat AMR. – Takes into account existing action plans and all available evidence and best practice – To apply a multisectoral approach by consulting..... Submit to 2015 Health Assembly through the Executive Board January 2015 – November 2014 | Antimicrobial Resistance Global Report on Surveillance 2014 Consultation on draft GAP (1) Online consultation held between 4 July and 1 September 2014 – Open to Member States, organizations – 130 contributions received from all relevant sectors • Member States, Government agencies and organizations: 54 • NGOs and civil society: 40 • Private sector: 16 • Academia: 16 • Other (International organizations): 4 | Antimicrobial Resistance Global Report on Surveillance 2014 Consultation on draft GAP (2) Strengthen tripartite collaboration – FAO, OIE, WHO – Worked together on development of global action plan • Shared actions for the collaboration 16 October consultation with Member States – http://www.who.int/drugresistance/memberstatemeeting/en/ 17 October 3rd meeting of WHO Advisory Group Additional Member State consultations scheduled – Optimizing use of medicines (Oslo, November) – Global surveillance (Stockholm, December) | Antimicrobial Resistance Global Report on Surveillance 2014 Draft global action plan will be based on… 5 Guiding principles – Whole of society engagement – Prevention first – Access, not excess – Sustainability – Incremental targets for implementation | Antimicrobial Resistance Global Report on Surveillance 2014 Five strategic objectives: Improve awareness and understanding Strengthen the knowledge and evidence base Reduce the incidence of infection Optimize the use of antimicrobial medicines Develop the economic case for sustainable investment Commitments to report progress | Antimicrobial Resistance Global Report on Surveillance 2014 Communication, Awareness, Training Public communication programmes Professional education, training, certification Schools curricula Public information and media Role for all stakeholders in promoting public understanding of infection prevention and use of antimicrobial medicines | Antimicrobial Resistance Global Report on Surveillance 2014 Strengthen the knowledge and evidence base Capacity to collect, analyse and report data Global surveillance based on national capacity Integration of data between human and animal sectors Develop global public health research agenda Implement (research funders to support) Repository of information Global health R&D observatory | Antimicrobial Resistance Global Report on Surveillance 2014 Reduce the incidence of infection Hygiene, infection prevention and control Healthcare settings (hospitals) Sanitation, water and food safety Control of STI, vector borne diseases HIV, gonorrhoea, malaria Role of vaccines and immunization Expand use of existing vaccines (e.g. pneumococcal) Reduce prevalence of infection inappropriately treated with antibiotics (e.g. influenza, rotavirus) New priority vaccines to prevent difficult-to-treat or untreatable infections Animal husbandry High density livestock (terrestrial and aquatic) | Antimicrobial Resistance Global Report on Surveillance 2014 Optimize use Regulatory mechanisms for new antibiotics Effective low-cost tools for diagnosis and susceptibility testing Access to medicines accompanied by measures to protect continued efficacy Code of practice | Antimicrobial Resistance Global Report on Surveillance 2014 Sustainable investment Economic case for investment Realizing the global investment needs Developing countries Coordinating initiatives aimed at renewing investment in new antibiotics, diagnostics & other tools | Antimicrobial Resistance Global Report on Surveillance 2014 Implementing, monitoring and evaluation Countries should develop and implement national action plans “building blocks” National priorities, circumstances WHO will develop a framework for monitoring and evaluation WHO to report every 2 years Others to develop own action plans and report within normal reporting cycle | Antimicrobial Resistance Global Report on Surveillance 2014 Thank you | Antimicrobial Resistance Global Report on Surveillance 2014