Pressure, flow, elasticity measurement methods
advertisement

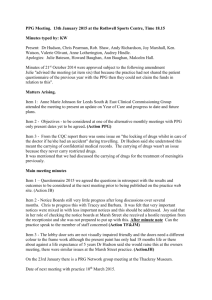
In vitro • Total control of confounding variables – Vasomotion, temperature changes, autoregulation, mean BP • Most accurate because vessel examined directly • Best for detailed information about mechanical properties of vessel material In vivo (invasive) • Realistic clinical information • Limited by technical problems – Measurement errors, transitory changes in diam. BP etc In vivo (non-invasive) • Further technical problems – Especially pressure Measurement of blood pressure • Invasive – Pressure catheter and transducer • Non invasive – Sphygmomanometry • Auscultation (by ear or automatically by microphone) • Oscillometry – Volume clamp – Tonometry Advantages/ drawbacks • Invasive – Accurate reproduction of central pressure waveforms – Risk of thrombosis and arrhythmias • Non-invasive – Quick, cheap, widely used – Lack of central pressure measurement – Requires skilled and experienced operators Sphygmomanometry Manometer (mercury or capsule type) Pulse detector (stethoscope or microphone) www.fmshk.com.hk/sahk/lecture_noninvasive.pp Sphygmomanometry • 1896 Blood pressure cuff (Riva Rocci) • 1905 First report of audible detection of heart sounds used with cuff (Korotkov) • 1968 Microphone used for automatic pressure measurement (Stegall) Sphygmomanometry Mercury sphygmomanometer Capsule manometer Replacing mercury spymomanometer Korotkov Sounds caused by vibration collapse of the arterial wall?? Cuff pressure Systolic Diastolic – Korotkoff IV is a better indication of diastolic pressure according to theory – However Korotkoff V is the commonly recommended measuring point except in pregnant patients because • It is associated with less interobserver variations • It is easier to detect by most observers www.fmshk.com.hk/sahk/lecture_noninvasive.pp Errors • Korotkoff sounds compared to invasive blood pressure measurement – Korotkoff IV is on average 8mm Hg above the invasively measured diastolic blood pressure – Korotkoff V is on average 2mm Hg above the invasively measured diastolic blood pressure Oscillometry • • • • Cuff round the arm Pressurise cuff (> systolic) Allow pressure to drop slowly to zero Measure pressure in the cuff during deflation Oscillometry: set up Microprocessor Air pump Bleed valve Pressure transducer Display Filtered signal Of cuff pressure Principle of oscillometry Variation of cuff pressure as cuff is deflated Limitations • Inaccurate / unreliable in shock patients • Inaccurate / unreliable in patients with arrhythmias – The algorithm of measurement assumes a regular pulse, so the reading is unreliable in patients with irregular pulse Advantages • No skill required • No subjective errors Volume clamp To pump Infra red emitter Pressure Finger Diameter Detected signal Air Change cuff pressure Air Artery Detector Measure cuff pressure Applanation tonometry Detects pressure of arterial pulsations through the skin Problem: • • • • Aortic and peripheral pressures are different. The heart doesn’t care what the pressure is in the radial artery. It only “sees” aortic pressure. Aortic pressure is difficult (impossible?) to measure noninvasively • Can we reconstruct the aortic waveform from the radial? Radial Aortic 120 Systolic 100 80 Mean Diastolic Yes we can. At least in principle • Record radial waveform with tonometry • Apply inverse transfer function • “Reconstruct” aortic waveform – What is an inverse transfer function? – How do we reconstruct the waveform? Fourier analysis H1 H2 H1 + H2 + H3 H4 2 1 0 -1 -2 90 180 270 360 H1 + H2 H3 H1+H2+H3+H4 Mean Measured aortic pressure radial artery pressure Pa(t) = pa0 + pa1Cos(t - a1) + pa2Cos(t - a2) + pa3Cos(t - a3) + ... Pb(t) = pr0 + pr1Cos(t - r1) + pr2Cos(t - r 2) + pr3Cos(t - r 3) + ... For each harmonic (n) Transfer function phase = an - rn Transfer function amplitude = pan / prn Amplification of the pulse AA - RA CA - RA AA - CA How to derive the central pressure from peripheral measurements • Compare Fourier series of “typical” aortic pressure waves with Fourier series of the radial pressure computed from tonometric measurements. • Calculate the amplitude ratio and phase difference for each harmonic • Apply this ratio and phase difference to each harmonic of the measured radial wave and reconstruct aortic wave that would when transmitted down the arm, produce the measured radial wave Question • How well does the typical transfer function apply to people of different ages and disease states Answer • Surprisingly well considering the changes that occur in the arterial system with age and vascular disease • However, most believe that more work is needed to validate the method Pressure transducers (for invasive measurement) Diaphragm manometer To pressure to be measured, (via an intra arterial cannula) Fluid filled chamber Stiff diaphragm Measure its movement electronically Advantages • Cheap, disposable • easy to use • Accurate mean pressure Disadvantages • Clotting in cannula, air bubbles • Therefore errors in pulse pressure Pressure transducers (for invasive measurement - 2) Semi conducting strain gauge Cannula tip manometer Diameter may be as small as 0.67 mm Advantages • High accuracy • Especially in very small vessels Disadvantages • No calibration possible when in position • Expensive • Fragile Pressure: comparison of methods Method Sensitivity Invasive Advantages/ disadvantages Auscultation + cuff OK No Subjective, limited to arm or leg. Good in skilled hands Oscillometry + cuff OK No As above but less subjective. No mean pressure. Catheter Good Yes Only direct way to measure in central vessels Volume clamp Good No Limited to peripheral arteries but can do small ones Tonometry V. Good No PPG V. Good No Superficial vessels only, sensitive to movement, good for carotid. No absolute P values. Can be calibrated against cuff methods Superficial vessels only. Used as a pulse detector in conjunction with cuff. PROMISING Flow Measurement • Invasive – Electromagnetic flow velocimetry – Ultrasonic transit time • Non invasive – – – – Doppler ultrasound Ultrasonic transit time Optical (small superficial vessels only) MRI Flow measurement • 1870 Fick principle described Flow in a given period of time = Amount of substance injected in that time/concentration difference before and after point of entry • 1886 Fick method first used by Grehart & Quinquardt • Modern instruments – – – – – Optical Electromagnetic 1936-1937 Kolin Ultrasonic transit time 1959 Ultrasonic Doppler 1961 MRI 1990’s (not commercial) Electrode Vessel diameter E = H.d.V Induced voltage Mean blood velocity Magnetic field strength i.d. 0.5 - 26 mm Principle of Doppler flow velocimetry c fl c l c c+v l ' f f ' cf (c + v ) f ' cf cf + vf ' f - f v f c vf Df c v c f 'l Flow: comparison of methods Method Sensitivity Invasive Advantages/ disadvantages Dilution Adequate No Cumb ersome, slow, mean values only Optical Good No Small superficial vessels only Doppler OK No Absolute flow values difficult to measure Transit time Good Yes None apart from expense and invasiveness E.M OK Yes Electrical noise, hard to calibrate accurately Diameter Measurement • Mechanical • Optical • Ultrasonic – Implanted crystals – Pulse echo • Cine-angiography • MRI Invasive Diameter Measurement • • • • • Ultrasound (external transducers) IVAS TV Mechanical Cine angiography Non-invasive diameter measurement • Pulse echo ultrasound (direct) • PWV (indirect) – Diameter wave – Flow wave – Pressure wave Other diameter methods Springy stainless steel Differential transformer TV camera Ultrasonic crystals (glued or sutured) Measure time delay Artery Transmitter Receiver Principle of pulse echo ultrasound Measure time delay between transmitted and received pulse Diameter: comparison of methods Method Sensitivity Invasive Advantages/ disadvantages Mechanical OK Yes Optical Good Ultrasound (crystals) Very good Yes (no) Non contact but sensitive to wall movement. N.I. method only measures rel. diam. Yes Difficult to set up, insensitive to wall movement Ultrasound (echo) Good No Cumb ersome, but insensitive to wall movement Sensitive to wall/patient movement, but only absolute non invasive method Elasticity measurement • Direct – Stress • pressure, tension, area, wall thickness – Strain • length, diameter • Indirect – Pulse wave velocity • detect pressure, diameter or flow pulse PWV Methods • Pressure pulse – Tonometry • Flow pulse – Doppler • Diameter Pulse – PPG Nature of the PPG Signal • Commonly regarded as a measure of changes in tissue volume due to arteriolar and capillary blood flow time varying absorption of light or i.r. • When detected in the vicinity of a large superficial artery, the signal is dominated by changes in the diameter (volume) of the artery. Optical detection of the diameter wave Upstream probe Infra red emitter Downstream probe Detector SKIN ARTERY FLOW MUSCLE/BONE Loukogeorgakis, et al. (2002). Physiological Measurement 23: 581-96. PhotoPlethysmoGraphy (PPG) for pulse wave velocity measurement. How does it work? d • Infra red probes detect transitory change in conduit artery volume due to the passage of the pulse wave • Measure time delay and distance between the probes • Pulse wave velocity = d/t • Pulse wave velocity (compliance)-1/2 t LED (emitter) Photo-transistor (detector) 20 mm 20 mm Validation experiments. Comparison of PPG with • Echo Tracking. – Does PPG method really measure large artery diameter? • Doppler. – How well do PPG derived pulse wave transit times compare to measurements using an established method? • Intra-arterial pressure wave. – Do transcutaneous transit time measurements compare with intra-arterial ones? PPG/Echo tracking methods Probes on the posterior tibial artery NIUS ultrasound probe PPG NIUS ultrasound probe Probes on the radial artery PPG PPG Relative amplitude 1 PPG Ultrasound 0.1 0.01 400 Ultrasound Phase 300 200 100 0 0 2 4 6 Frequency (Hz) 8 10 PPG/Echo Tracking - Conclusions. • PPG reproduces the diameter wave with reasonable fidelity, when compared to high precision echo tracking system. • Timing of the foot is close Validation experiments. Comparison of PPG with • Echo Tracking. – Does PPG method really measure diameter? • Doppler. – How well do PPG derived pulse wave transit times compare to measurements using an established method? PPG/Doppler methods Probes on the posterior tibial artery Doppler Doppler PPG PPG ECG PPG Probes on the radial artery Doppler ECG used as time reference Comparison of PPG and Doppler transit times TT PPG [ms] y = 0.90x + 12.8 r = 0.95 350 300 250 Leg 200 Arm 150 100 100 150 200 250 TT Doppler [ms] 300 350 Comparison of PPG and Doppler. Difference v mean Doppler - PPG [ms] 50 + 2SD 25 Mean difference = 8.6 ms Leg 0.0 Arm -25 - 2SD -50 0 100 200 Average [ms] 300 400 PPG/Doppler - Conclusions. • PPG transit times agree satisfactorily with Doppler values recorded at the ‘same’ site. • The difference plot shows – the transit time estimated by the Doppler instrument is consistently greater than that derived from the PPG signals (mean difference 8.6 ms) • The discrepancy is due to the Doppler signal processing Validation experiments. Comparison of PPG with • Echo Tracking. – Does PPG method really measure diameter? • Doppler. – How well do PPG derived pulse wave transit times compare to measurements using an established method? • Intra-arterial pressure wave. – How well do transcutaneous transit time measurements compare with intra-arterial ones? Subjects Measurements on 21 volunteers (8 female, age range 33 to 78 years, mean 57) after elective coronary angiography, under the approval of the regional research ethics committee. TP1 Pressure measurement pos. 1 ECG Femoral arteriotomy Inguinal ligament TP1 Pressure measurement pos. 1 ECG DTP DTPPG TP2 TPPG Inguinal ligament PPG measurement pos. Pressure measurement pos. 2 TC Femoral arteriotomy = TP2-TP1 = TPPG-TP1 +TC Comparison of PPG and intra-arterial transit times PPG transit time [ms] 110 y = 0.68x + 22, r = 0.66, P < 0.005 100 90 80 70 60 50 40 40 50 60 70 80 90 Intra arterial transit time [ms] 100 110 Comparison of PPG and intra-arterial transit times. Difference v mean I.A. - PPG [ms] 30 + 2SD 20 Mean difference = 0.0 ms 10 0.0 -10 -20 - 2SD -30 40 50 60 70 80 90 Mean transit time [ms] 100 110 Some limitations. • Non simultaneous measurement of proximal and distal signals – Ethical constraint of one catheter • Proximal signal not transcutaneous – ‘Hybrid’ measurements will avoid this. i.e. aortic signal from Doppler, distal signal from PPG. – Current hardware and software will allow this. • Effect of errors in distance between measurement sites not investigated – Careful comparison between I.A. and external distance measurements required. PPG/Intra-arterial - Conclusions. • Reasonable correlation between intra-arterial and PPG transit times and pulse wave velocities. • Mean difference between the two methods close to zero • Transcutaneous estimation of pulse wave transit time provides an acceptable estimate of its intra-arterial value. – Errors in distance measurement must be carefully considered Summary of validation results. Comparison of PPG with • Echo Tracking. – Does PPG faithfully measure large artery diameter changes and pulse wave timing? • Yes! Doppler. – How well do PPG derived pulse wave transit times compare to measurements using an established method? Reasonably • Intra-arterial pressure wave. – Do transcutaneous transit time measurements compare with intra-arterial ones? Reasonably Examples of current usage • Paediatric PWV studies – Kawasaki disease – Twin to twin transfusion syndrome – Children of diabetic mothers – Zambian schoolchildren of known birthweight and nutritional status Conclusions • PPG measurements of PWV in superficial arteries compare well with other methods • Although we don’t yet know quite what we’re measuring – Capillary and/or large artery volume changes? – More work needed Assessment of endothelial function • Endothelial function – The ability of the vascular endothelium to release vasodilators in response to reduced mean shear stress • Nitric oxide • PGI2 • EDHF • Endothelial function is a reliable indicator of vascular “health” – Continuous production of nitric oxide maintains a low basal level of vascular tone and peripheral resistance – If NO production is impaired: • Coronary arteries angina • Peripheral arteries mean BP increases • Peripheral endo function closely mirrors that in coronary artery Assessment of endothelial function Impaired endothelial function has prognostic and diagnostic value • a strong predictor of cardiovascular morbidity and mortality • associated with a wide range of CV pathology – – – – Angina Type II diabetes Smoking Essential hypertension How to assess endothelial function • Direct – Measure diameter of muscular artery in response to change in shear stress (flow) • Normally induced by reactive hypersaemia after a period of downstream occlusion • B mode or echo tracking ultrasound (+ doppler) – Expensive – Highly skilled operators needed – Not in routine clinical use • Indirect – – – – Venous occlusion plethysmography Peripheral artery tonometry Distal temperature changes Change in arterial compliance Principle • Relaxation of vascular smooth muscle reduction in arterial stiffness • Reduced stiffness reduced pulsewave velocity Protocol Experiment A Effect of exercise on brachio-radial PWV • • • • Base line PWV measurement 5 minutes biceps curl PWV measurements at 1, 2, 5 and 10 minutes 47 healthy volunteers Experiment B Effect of ischaemia on brachio-radial PWV • • • • Base line PWV measurement 3 minutes forearm artery occlusion (BP cuff) PWV measurements at 0.5, 1, 2 and 5 minutes 36 healthy volunteers Results Exercise test Mean pulse wave velocity change relative to baseline 0.3 0.2 0.1 0 0 1 2 3 4 5 6 7 -0.1 -0.2 -0.3 Time after exercise [minutes] 8 9 10 11 Results Mean pulse wave velocity change relative to baseline Forearm ischaemia 0.4 0.3 0.2 0.1 0 1 2 3 4 -0.1 -0.2 -0.3 -0.4 Time after cuff deflation [minutes] 5 6 Conclusions • PPG is a reliable, repeatable low cost and robust alternative to the range of methods available for measuring PWV • It is ideal for paediatric studies • Changes in PWV may be a simple, low cost method for assesing endothelial function. – Very preliminary study Flow-mediated changes in pulse wave velocity: a new clinical measure of endothelial function. Naka KK. Tweddel AC. Doshi SN. Goodfellow J. Henderson AH. European Heart Journal. 27:302-9, 2006 Feb. Leg Arm Hyperaemia increased brachial artery diameter by 8% at this time. GTN had similar effect Hyperaemia had negligible effect on brachial artery diameter. GTN reduced diameter by similar amount to controls Mandrel: diameter 4-10 mm Centralising lid Sleeve: i.d 4 - 12.5 mm o.d 18 mm Artery Outer Container Ejection screw Frozen A rtery Reaming T runnion