Feeding Infants and Toddlers Study (FITS)
advertisement

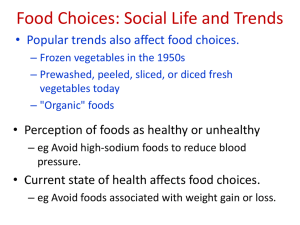
An Ounce of Prevention is worth a pound Shaping Habits That Shape Obesity Ohio Chapter, American Academy of Pediatrics Ohio Department of Health Ohio Dietetics Association Prevalence of Obesity U.S. Adults: 2001-2 • Obese 1/3 (30.6%) • Overweight 2/3 (65.7%) • Extreme obesity (5.1%) All ages Both sexes All ethnic groups All socioeconomic levels Source: Hedley et al. 2004; Freedman et al. 2002 Prevalence of Overweight in U.S. Children: 2002 Age, yrs At Risk (> 85%) (%) Overweight (> 95%) (%) 2-5 6-11 12-19 All 6-19 22.6 31.2 30.9 31.0 10.3 15.8 16.1 16.0 * Overweight among non-Hispanic Black (20.5%) and Mexican-American (22.2%) increased much more rapidly than among whites between NHANES in ‘88-94 and 2002 Source: Hedley et al. 2004 Obesity Among African-American Adults: 2002 Age, yrs Overweight BMI > 25 % Obese BMI > 30 % Extreme BMI > 40 % Males 20-39 40-59 55.4 65.0 24.7 29.7 4.1 2.9 Females 20-39 40-59 70.3 81.5 46.6 50.6 11.8 15.1 Source: Hedley et al. 2004. Overweight Status of African-American Children: 2002 Percentile All Ages % 2-5 yrs % 6-11 yrs % 12-19 yrs % Males 85 95 31.0 17.9 23.2 8.0 20.9 17.0 32.1 18.7 Females 85 95 40.1 23.2 25.6 9.6 37.9 22.8 41.9 23.6 Source: Hedley et al. 2004. Class 3 Obesity in the U.S. 1990 through 2000 BMI <25 25-29.9 Prevalence, % 50 30-34.9 • Class 3 = BMI > 40 • 2-fold higher risk of mortality than BMI 30 10 5 35-39.9 >40 1 • High likelihood of bariatric surgery • Those over age 20 yrs 1990 1992 1994 1996 1998 2000 Year Prevalence increased 3-fold in only a decade and continues to rise – In population 4.9% – In black females 13.5% Medical Consequences of Obesity • Psychosocial • Medical • Cardiovascular – Polycystic ovary disease – Lipidemia – Gall bladder disease – Diabetes mellitus – Osteoarthritis – Hypertension – Cancer – Respiratory • Pregnancy and postpartum ??? – Cardiac • Mortality Diseases that begin in childhood amplify morbidity – and costs Source: Krebs & Jacobson 2003; Dietz 1998a; Dietz 1998b; Must 2003. Prevalence of Diabetes in US Has Risen Dramatically –1990 to 2001 And how many overweight adults and kids have pre-diabetes? Source: Narayan et al. 2003; Sinha et al. 2002; Weiss et al. 2003. Life-Years Lost from Diabetes in the US • If diagnosed at age 40 years – White • male: • female: • If diagnosed at age 10 years – White 1.01 yrs 13.5 yrs – Hispanic • male: 16.5 yrs • female: 18.0 yrs – Hispanic • male: 11.5 yrs • male: 19.0 yrs • female: 12.4 yrs • female: 16.0 yrs – Black – Black • male: 13.0 yrs • male: 22.0 yrs • female: 17.0 yrs • female: 23.0 yrs Source: Narayan et al. 2003 “Because of the increasing rates of obesity, unhealthy eating habits, and physical inactivity,we may see the first generation that will be less healthy and have a shorter life expectancy than their parents” Richard H. Carmona, MD, MPH, FACS Surgeon General U.S. Dept of Health and Human Services, 2004 Obesity Risk Increases with the Age of the Child • Obese at 6 years – 50% risk of obesity at 35 yrs • Obese at 10 years – 70 - 80% risk Obesity is a pediatric disorder with Source: Bray 2002, Dietz 1998a, Dietzs 1998b, adult consequences Guo et al. 2002; Kvaavik et al. 2003; `Must 2003, Whitaker et al. 1997; The State of Ohio’s Teens Youth Risk Behavior Survey 2003 • 57% participate in organized after-school activities • 68% reported participating in vigorous activity in any given week; only 41% attend PE classes • 32% watch 3 or more hours of TV per average school day • 14% report being overweight, up from 10% in 1999 • 30% report eating fruits one or more times per day in the past week • 38% report eating vegetables one or more times per day in the past week (includes potatoes) • 20% report drinking the recommended 3 glasses per day of milk Source: Bray 2002; Ohio Dept of Health: www.odh.state.oh.us Nutritional Gaps in U.S. Children % Children Consuming Daily Recommended Intake Critical Age 120 100 80 Iron Phosphorus 60 Zinc Vitamin C 40 Vitamin A Magnesium Folate Calcium 20 0 6-11 Mo. 1 Yr. 1-4 Yrs. 5-8 Yrs. 9-14 Yrs. 15-19 Yrs. NHANES, CFSII data compiled by Dr. John Lasekan, Ross Labs Children grow up In 3 environments HOME COMMUNITY SCHOOL The issue of obesity Is multifactorial but parents, especially mothers, have an opportunity to create a healthful home environment Babies are Getting Bigger Year N BW (g) Z score % SGA %LGA 1978-9 5626 3419 -0.91 11.1 8.0 80-81 5659 3426 -0.046 10.3 8.4 82-83 6333 3453 0.013 8.9 9.9 84-85 6222 3449 0.050 8.2 10.0 86-87 6192 3465 0.102 7.8 11.2 88-89 6482 3462 0.078 7.5 10.6 90-91 6985 3456 0.077 7.5 10.7 92-93 6621 3471 0.098 8.1 11.7 94-96 7079 3476 0.128 7.2 11.5 <0.001 <0.001 <0.001 <0.001 P value Births > 37 wks GA Source: Kramer 2002 Babies Are Getting Bigger And Moms Are the Reason • McGill University database 1978-1996 • Mean birth weight and z-score increased over two decades (p < 0.0001) • No trends in premie birth weights – Prepregnancy obesity: from 4.7 to 10.6% – Gestational diabetes: a 20-fold increase Prenatal • Maternal weight gain – An important predictor of later obesity in the child • Breastfeeding – Encourage breastfeeding – Lower incidence of obesity in breastfed infants Is Breastfeeding Protective against Obesity Later in Life? • Von Kries, 1999 German • Hediger, 2001 US 3-5 yr olds • Gillman, 2001 US 9-14 yr old • Liese, 2001 German 9-10 yr old • Armstrong, 2003 Scottish 3-4 yr olds • Bergman, 2003 German 6 yr olds • Toschke, 2003 Czech 6-14 yr old 5-6 yr olds Healthy People 2010 Breastfeeding Recommendations • Increase the proportion of mothers who breastfeed to 75% in the postpartum period • Increase rates to 50% at 6 mos • Increase rates to 25% at 12 mos In-Hospital Breastfeeding Rates 1965-2001 80% 69.5% 61.9% 70% 51.5% 60% 50% 55.0% 40% 43.5% 24.7% 46.3% 30% 20% 21.7% 10% 0% '65 '67 '69 '71 '73 '75 '77 '79 '81 '83 '85 '87 '89 '91 '93 '95 '97 '99 '01 Any BF Exclusive BF Breastfeeding Rates at 6 Months 1971-2001 50% 40% 30% 32.5% 27.1% 17.6% 20% 10% 19.8% 17.2% 10.4% 0% '71 '73 '75 '77 '79 '81 '83 '85 '87 '89 '91 '93 '95 '97 '99 '01 Any BF Exclusive BF Largest Increases in In-Hospital Breastfeeding 1996-2001 Demographic 1996 2001 % Change African American 37.1 52.9 42.6 < 20 yrs of age 43.3 57.2 32.1 WIC participant 46.6 58.2 24.9 20-24 yrs of age 52.7 65.9 24.5 High school education 49.2 61.1 24.2 National 59.2 69.5 17.4 Source: Ryan 2002 Obesity (Pre- or In-Pregnancy Weight) Threatens Breast-feeding (BF) • Pediatric & Pregnancy Nutrition Surveillance Surveys – 51,329 women and babies – Pregnant and gestational weight gain + BF – Both pre- and in-pregnancy obesity resulted in: • Less initiation of BF • Shorter duration of BF • Increasing obesity may threaten recent gains in breast-feeding Source: Li 2003 Train parents in how and what to feed their baby Where Do Parents Look for Nutrition Information? • #1 Pediatrician/ Family MD • Social environment • Magazines • Internet • Dietitian • TV • Nutrition Center • Food labels • Media Source: Van Dillen 2003 The 12 Well-Child Visits 11 12 7 5 10 9 2 8 4 3 Anticipate problem feeding and activity practices 6 Newborn/First Visit • For Breastfed and Formula Fed Infants – Help sustain breastfeeding by building skills and offering resources for support – Iron-based formulas only – Hunger and satiety cues – Babies should regulate their own intake – Crying does not always represent hunger • It is normal for 1-3 month old babies to cry up to 3 hours per day How are Infants Fed? Milk Feeding 2000 Cow's Milk 100 90 % of Milk Feeding 80 70 Formula 60 50 40 Human Milk & Formula 30 20 10 0 In Hospital Human Milk 1 to 3 4 to 6 7 to 9 10 to 12 Months Source: Ryan et al. 2002 Calorie Intake (kal/kg/day) Volume of Intake (mL/kg/day) Infants Adjust Their Calories 200 53 kcal/100ml 67 kcal/100 ml 100 kcal/100 ml 180 160 140 120 100 130 By 6 weeks, the baby regulates its own energy intake 120 110 100 90 814 28 42 56 84 Age (days) 112 Source: Fomon 2004. From birth to 24 months, the child assumes the eating habits of the family The Feeding Infants And Toddlers Study (FITS) Source:Dwyer, 2004 FITS Study Methodology • Adds critical information to augment NHANES, CFSII, Ross Mother’s Survey information • 5 Gerber sponsored FITS surveys over 30 yrs • Snapshot of eating habits in first 2 years (2002) • Random sample of 3022 (Experian database) – Recruitment and household review – 24-hr dietary recall and subject information – Second dietary recall for subset (n=703) – Response rate for recalls 94% Source: Devaney et al. 2004a FITS: Nutrient Intakes 0-24 months of age • Examined transitional times for feeding – 4-6 months • Exceeds adequate intake for all nutrients, 0-12 months and almost all nutrients, 12-24 mos – 7-11 months • Vitamin E low 12-24 mos – 12-24 months • Fiber low in toddlers • Diets found to vary widely day-to-day • Nutrition is good over the first 24 months • But energy intake exceeds Estimated Energy Requirement (EER) at all ages Source: Devaney et al. 2004 b Energy Intake Infants and Toddlers • Energy intake exceeds EER • Feeding – Breast < EER – 4-6 mo 10% – BF/ formula = EER – 7-11 mo 23% – Formula – 12-24 mo 31% > ERR – Solids and cereals add to energy intakes, especially when coupled with formula Two-Month Visit • Infant Feeding – Set expectations: • the baby will increase to 24-28 oz/day over the next 2 months – Provide 4 oz four to six times per day – No cereal, no baby food, no juices – Nothing added in the bottle Not all Crying Needs Food Two Months • Learn to interpret the infant’s cries • Parents eager to “empty the bottle” encourage overeating • Satiety cues between 4-12 weeks: – Turns head away or releases nipple – Falls asleep • Comfort the baby – Rocking, massaging, cuddling, or listening to music Recommendations for Iron • Healthy People 2010: “…reduce iron-deficiency among children aged one to two years to 5%” • AAP Committee on Nutrition – Supplement breastfed infants with iron – Iron-fortified formula is the appropriate substitute for breastfeeding in the first 12 months – Iron fortified infant cereals and grains, as well as meats are important sources of iron, especially for infants who continue to breastfeed beyond 6 months of age Physical Activities Two Months • Minimize stationary devices • Use crib mobiles • Encourage reaching, kicking, stretching, and belly play time • No T.V. 4-Month Visit • The addition of cereal – No solids until developmentally ready to use a spoon, usually 4-6 mos of age – Cereal only with a spoon, not in the bottle – Start a single grain, iron-fortified cereal – Portion: increase to 1-2 Tbsp twice daily • First baby food: vegetables at 6 mos Excessive Juice is a Risk for Obesity • Both short stature and obesity are tied to excessive intake of juices – Only 100% juice – Only after 6 months of age – Only from a cup, not from a bottle – Limit to 3 oz initially with a maximum of 4-6 oz / day for 1-6 year olds Promote Vegetables for Infants & Toddlers • Fail to consume vegetables as a discrete food: • Potatoes – consume daily – 4-6 mos 3.6% – 9-11 months 27 % – 7-8 mos 12.4% – 12 months 18-23% – 9-11 mos 24.1% – 12-14 mos 33.2% – 15-18 mos 42.0% – 19-24 mos 40.6% – Dark Green Vegetables are consumed by fewer than 10% of toddlers – Deep yellow vegetables decrease from 39% at 9 mos to 14% at 18 mos – By 24 mos 25% of toddlers consume fried potatoes on any day Source: Fox et al. 2004 Feeding the Baby • Infants innately prefer sweet and salty. • Infants may reject bitter and sour • Infants tend to resist new foods (neophobic) Implications… • More than 10 exposures may be needed to establish a new food. • Children like and eat what is familiar • Parental eating habits influence the baby’s choices at this age Physical Activities Four Months • Non-restrictive play – Belly play time – Sits with support – Reaches and holds objects – Play gyms – No TV Top 5 Fruits FITS Study, 2004 Age (mos) #1 2 3 4 5 4-6 Applesauce Baby bananas Pears Peaches Fresh bananas 7-8 Applesauce Baby bananas Pears Peaches Fresh bananas 9-11 Bananas Applesauce Baby bananas Pears Cand applesauce 12-14 Banana Applesauce Grapes Apple Peaches 15-18 Banana Grapes Apples Strawberries Peaches 19-24 Banana Apple Grapes Raisins Strawberries Source: Fox et al. 2004 Six-Month Visit • Start vegetables and offer first at each meal • Add one new food every 3-4 days • Portion sizes – Cereal 2-4 tablespoons twice per day – Vegetables 2 tablespoons twice per day – Fruits 2 tablespoons twice per day Meats & Proteins for Infants & Toddlers Age (mos) Chicken, Turkey (%) Hotdogs, Sausages (%) Beef (%) Pork, Ham (%) Fish, shellfish (%) 4-6 2.0 % 0.0 % 0.9 % 0.3 % 0.0 % 7-8 7.3 2.1 2.6 1.7 0.5 9-11 22.4 7.1 7.7 4.0 1.9 12-14 33.0 16.4 16.1 9.7 5.5 15-18 46.9 20.1 16.3 11.3 8.7 19-24 47.3 27.0 19.3 13.9 7.1 Source: Fox et al. 2004 Common Early Feeding Traps • Anticipate that daily milk intake will fall as baby’s food intake increases • Avoid “combo dinners” and baby desserts • The extrusion reflex is normal and does not mean that the baby doesn’t like the food • New foods require multiple presentations • Focus on new eating experiences and skills Physical Activities Six Months • Minimize stationary devices • Sits without support • Starting to crawl • First signs of independent mobility • No T.V. until after 24 months of age Nine-Month Visit • Offer many new foods and textures • Introduce a cup as the diet advances • Discuss choking hazards Aim to Develop Self-feeding Skills • Never use food as reward or bribe • Offer variety: finger and table foods – New food types and textures – Veggies & fruits at every meal – Establish a variety of meats What Infants & Toddlers Drink Age All Milks (mos) (%) 100% Juice (%) Fruit Drinks (%) Soft Drinks (%) Water 4-6 100 21.3 1.6 0.1 33.7 7-8 100 45.6 7.1 1.1 56.1 9-11 99.7 55.3 12.4 1.7 66.9 12-14 98.2 56.2 29.1 4.5 72.2 15-18 94.2 57.8 38.6 11.2 74.0 19-24 93.4 61.6 42.6 11.9 77.0 (%) Source: Skinner et al. 2004 Nine-Month Visit • Continue breastmilk and/or ironfortified formula until 12 months • 100% fruit juice, 4-6 oz maximum and only from a cup • Avoid all other sugary drinks • ¼ cup (2 oz) fruits and vegetables daily • Promote textures to improve skills AAP Recommendations: Cow’s Milk and Fat Intake • Delay the introduction of cow’s milk until one year of age • Calcium intake for 1-3 year olds should be 500 mg/day • Cow’s milk should be whole milk - not reduced-fat or non-fat - during the second 12 months of life • Fat intake should not be restricted in the first 24 months of life And now, a word about…TV Age (mos) 0-1 1-2 3-4 >5 hours per day 0-11 83 11 4 3 12-23 52 27 11 11 24-35 21 38 25 16 Children watching > 2 hrs a day at age 2 yrs were more likely to watch > 2 hrs a day at 6 yrs too. Television and Obesity Are Linked • TV > 2 hrs/ day in 5-15 yr olds is associated with adult overweight, high cholesterol, and low fitness • Even brief exposure to TV ads can influence a preschooler’s food choices • Mean TV watched by 3-4 yr olds = 2.2 hrs/ day • Maternal obesity and depression correlates with the highest TV viewing by their children Physical Activities Nine Months • Begins to hold cup • Spoon feeds with help • Encourage crawling • Pulls to stand • No T.V. Twelve-Month Visit • Introduce regular milk – Whole milk - not skim or 2% – Taper from 24 oz. to 16 oz. per day – All fluids from a cup – Continue to wean from the bottle • Fluids – Avoid sweetened drinks – Water is best for extra fluid Cereals Infants & Toddlers Age (mos) Any Grain (%) Infant Cereal (%) NonSweet (%) Sweet Cereal (%) Cereal Bars (%) 4-6 65.8 64.8 0.5 0.0 0.0 7-8 91.5 81.2 17.0 1.8 1.1 9-11 97.5 63.8 37.0 9.0 3.4 12-14 97.8 23.9 44.5 17.7 9.8 15-18 98.6 9.2 40.6 26.4 10.0 19-24 99.2 3.1 31.9 22.7 9.7 Source: Fox et al. 2004 Twelve Months • Solid foods – Emphasize eating skills and experiences – 3 regular meals & 2-3 planned snacks – Avoid “grazing” throughout the day – Emphasize vegetables and fruits • Appropriate serving size is 1/2 cup of fresh (or 1/3 cup canned) fruits/ vegetables per serving per meal Parental Control Measures Usually Backfire • Restricting “bad” (ie, palatable and enjoyable) foods encourages their consumption and raises a desire for future intake • Avoid a mixed message that forbidden foods are “bad” except on special occasions • Avoid food as a comfort or a reward • Categorical thinking about “good” and “bad” foods is common and inappropriate Physical Activities Twelve Months • Push toys • Walking • Running • Unrestrictive play • Never inactive for more than 60 mins • No T.V. 15- and 18-Month Visits • No more bottle – Whole milk from a cup in four 4-oz servings / day – Milk limit 16 oz/day – 100% fruit juice 6 oz/ day – No bottle and no “sippy” cup • Snack times – 2-3 planned snacks per day – Watch portion size, nutritional value • Meal times – 3 meals per day – Variety of color, texture, and tastes – New foods at the start of the meal – 10 exposures of each new food Caution: Choking Hazards! • Nuts • Popcorn • Grapes • Round candies • Apple chunks, slices • Hard chunks of uncooked veggies • Sausages • Hot dogs Some foods are dangerous because the infant can’t chew or coordinate swallows and lacks a full set of teeth. Safe Snacks for the Toddler • Cheese • Yogurt • Fruit (watch for seeds and peels) • Saltines • Fruit smoothies • Graham crackers • Steamed veggies • Pretzels • Puddings • Bagel, bread, toast • Unsweetened cereals • Whole wheat crackers • Mashed/ finely cut meats or fish Avoid the habit of snacking in the car and on the go Desserts and Sweets Age Any Dessert (%) 10.4 Baby Desserts (%) 4.2 Cakes, Pastries, Cookies (%) 4.3 Candy 7-8 45.8 17.7 27.0 1.1 9-11 61.1 17.0 40.9 3.2 12-14 78.8 6.0 50.5 10.2 15-18 88.8 2.3 60.2 15.2 19-24 90.5 0.0 61.6 20.0 (mos) 4-6 Infants Don’t Need Desserts (%) 0.0 Source: Fox et al. 2002 ??? 15- and 18-Month Visits • Meals are social occasions – Establish family meals – Adults should act as role models during meals – Milk with meals – Limit desserts, avoid candy – TV off during meals National Recommendations Fiber = ‘Age plus 5’ • Fiber should equal the age of the child plus 5 grams a day – For a 2-year old that would be 2 + 5 g = 7 g/day – Maximum = age + 10 g/day • Emphasize whole grains to boost fiber Dietary Fiber Intake of 4 to 10-yr-old US Children • Children who meet the ‘Age plus 5’ rule – 4-6 year olds 45% – 7-10 year olds 32% • Children who meet this rule consume more breads, cereals, fruits, vegetables, nuts, legumes and seeds • Low fiber intakes are associated with higher fat and cholesterol Recommendations for Grains and Whole Grains for Children • Healthy People 2010: “Increase the proportion of persons aged 2 and older who consume at least 6 daily servings of grain products, with at least 3 being whole grains” • Serving is defined by the USDA Dietary Guidelines for Americans 2005: 3 or more ounce equivalents of whole grain products per day (at least ½ of grains from whole grains) • Primary sources of whole grains for children: – Ready-to-eat cereals Yeast breads – Corn & other chips Popcorn – Hot breakfast cereals crackers Whole Grain Intakes are Poor Continuing Survey of Food Intakes by Individuals 1994-6 Age Total Grains Whole Grains Mean Servings/ Day 2-18 years 6.6 0.9 2-5 years 5.0 0.8 6-11 years 6.5 0.9 12-18 years 7.7 1.0 Source: Harnack et al. 2003. The Parent’s Role “It is the parent’s responsibility to offer the child a healthful variety of foods and a supportive eating environment ... Satter, J Am Diet Assoc. 1986; 16:355 Source: Satter 1986 The Child’s Role …and it is the child’s responsibility to decide when and how much to eat.” Source: Satter 1986 Two Years • Activity: – Only planned TV & only 1 hour per day – Planned time outdoors every day • Milk – Milk at every meal – Switch from whole milk to 2% • Meals – Begin to decrease the fat content of foods – Appropriate portion sizes at home and away: 1 Tbsp per year of age Subjects for More In-Depth Discussion with Parents • Parents “bias” a child’s food choices • The picky eater grows up just fine • Food jags are normal • Plate and glass sizes alter intake • Food dislikes over time • The problem of “dessert” • Avoid in-car snacking • Food rules should be shared with daycare provider, grandparents • Eating out with a child • Letting the child direct their own intake The Problem of “Dessert” • A place in a balanced meal for dessert foods • Not a required part of meal planning though • Not necessary at every meal • Not a reward or bribe for eating other foods • OK to use fruit, yogurt, cheese • OK for celebrations away from home Eating at Restaurants • Split meals between kids or share yours • Recall portion size: ¼ the adult portion • Buffets promote overconsumption • Drinks: ask for milk with the kids’ meals • Pre-meal: watch out for breads & crackers • Salad dressing: serve on the side, use as dip Two-Year Visit • Meals: All 5 food groups daily – Begin to decrease the fat content – Appropriate portion sizes at home and away: 1 Tbsp per year of age or ¼ of an adult portion – Plate and cup size matters – Food “jags” are typical & normal – A variety of textures, colors, flavors – Don’t bias your child’s food choices Top 10 Sources of Dietary Fats for Children 2-5 yrs Total Fat Rank Sat. Fat Rank Whole milk 11.3 1 17.8 1 Sweet grain products 8.5 2 6.5 6 Franks, sausage, meat 8.1 3 7.6 3 Mainly grain mix 7.3 4 7.4 4 Nut buttters, nuts, seeds 5.8 5 2.4 14 Natural/ processed cheese 5.2 6 8.2 2 Beef 5.1 7 5.3 8 Butter/margarine 4.9 8 4.2 9 Salty snacks 4.6 9 3.4 11 Low fat milk (1-2%) 4.6 10 7.3 5 Source: Thompson & Dennison, 1994 Milk Intake of Infants & Toddlers Age Breast Formula Cowmilk Low-fat (mos) (%) (%) (%) (%) 4-6 39.6 74.1 0.8 0.3 7-8 25.7 82.2 2.9 0.5 9-11 21.3 75.0 20.3 5.3 12-14 13.6 21.2 84.8 17.7 15-18 4.2 5.1 88.3 20.7 19-24 4.5 1.5 87.7 38.1 Source: Fox et al. 2004 Drinks Matter Early Food Preferences Predict Future Food Preferences • The “displacement theory” is real – Calcium intake falls as milk is replaced – Vitamin C rises as juices replace milks • Beverages are important: – They provide >1/3 of daily calcium, Vits A, C, D, protein and zinc • Fruit drinks are too common : – By 2 years 40% drink them daily and 5% drink > 16 oz/d • Soft drinks are unnecessary: – >11% toddlers 15-24 months consume them daily Source: Skinner et al. 2004 Physical Activites Two Years • Encourage active play with other children • Marching • Jumping • Climbing • Limit T.V. to 1-2 hours per day • Get outside Three- and Four-Year Visits • Meal times – Planned meal & snack times – Establish a family mealtime free of TV – Move toward skim milk – Variety: fruits, vegetables, whole grains – Limit potatoes – Avoid the TV & Food habit – Limit TV to 1-2 hrs per day – Help child choose what to watch Physical Activities Three / Four Years • Throwing and bouncing balls • Jumping • Running • Ride tricycle • Unstructured play at least 30 minutes/ day • Structured play at least 60 minutes/ day • T.V. limited to 1-2 hours per day Five- and Six-Year Visits • Daily diet suggestions – A nutritious breakfast every day – School lunch or a quality brown bag lunch – Milk and dairy at every meal – Fruits and vegetables in abundance – Plan healthful snacks for after-school time – Limit soft drinks and fruit drinks – Caution when eating at restaurants – share your meal with your child Eating a School Lunch Promotes Better Nutrition ?Eating a Lunch While at School ? - or take out pic of lunch box from home • Consume twice the servings of fruits and vegetables • Higher intake of milk and dairy • Larger amounts of meat • Greater amount of grains • More vitamins and minerals • NSLP impact holds true for lunch and for 24-hour intake USDA Food and Nutrition Report No. CN-01-CD1 Five Years • Daily activity suggestions – Plan outdoor time and reading time daily – Limit “screens” to 1-2 hrs/ day, including • computers • games • TV • movies Decreased TV viewing has been proven to alter obesity Obesity & Psychological Issues • Victimization/ bullying • Sense of alienation • Depression • Behavioral problems • Lifelong psychological issues • Low self-esteem • A cycle of food, depression and inactivity Energy-Dense Nutrient-Poor Foods Definition • Tip of the Food Pyramid: fats, oils, sugars • NHANES III 1988-94: 4,265 foods classified – Foods are considered to be in the EDNP group if they are not part of the following food groups: • Dairy – milk, buttermilk, cheese yogurt • Fruit – fresh, frozen, canned, juice • Grains – bread, cereal, pasta, rice • Meat & Beans – meat, fish, poultry, eggs, beans, nuts, seeds • Vegetables – raw, fresh, frozen, canned, juices • Mixed – foods from several groups Energy-Dense, Nutrient-Poor Foods NHANES III • EDNP foods = nearly 1/3 of daily energy intake • As EDNP foods increased – Mean daily total calories increased – Percent energy from carbs increased – Percent energy from fat increased – Fiber, protein, vitamins, decreased – carotenoids, iron, calcium, folate decreased As EDNP foods increase, nutrition from other 5 food groups falls = displacement Source: Kant 2000 Snacking Among Children 1977 to 1996 • 3 dietary surveys in children 2-18 yrs (N = 21,236) • “Snack” = foods grouped outside of meals • Snacking adds 30% kcal to the diet • Highest snack intake is among 2-5 year olds • Energy per snack rose only 3% in 20 yrs • Energy density is greater than meals • Increased frequency, not size of snacks is the trend in America Source: Jahns et al. 2001 American Dietetic Association Snack Guidelines Preschool-/ School-Age • Continue 2-3 planned snacks for preschool age and 1-3 for school age children • Aim for variety of texture, taste, and color • Adjust portion size to age • Allow the child to respond to internal cues of hunger and fullness • Healthy snacks are whole grains (breads, cereals, crackers), fruits and veggies, lean meats, and dairy products (low-fat cheese, pudding, yogurt) Eating Out with Your Child • Include at least two different food groups • Limit sweets to one per meal • Only one fried food per meal • Assure that all foods, especially desserts and drinks, are child-sized Source: Satter 1986 Control Portion Sizes When Eating Out • Share your meal or order a half-portion • Order an appetizer as an entrée • Take half your meal home • Be aware and stop eating when you feel full • Avoid super-sized sweetened drinks • When traveling, pack nutritious snacks Weight Control Information Network, NIDDK, Jan 2003 More Tips for Portion Control • Before eating, assess your hunger • Eat slowly and appreciate your food • Eat small meals more frequently to avoid hunger • Measure your food portions to hone your portion perception • Skip “family style” servings except for veggies • Always serve salad dressing on the side • Interpret labels in terms of single servings Susan Burke, MS, RD, CDE Menu Hints While Eating Out • English muffin, toast, bagel NOT croissant, biscuit, pastry • Ham NOT sausage • Low-fat milk, fruit juice or water NOT soft drinks or shakes • Baked, broiled or poached NOT fried • Catsup, mustard, BBQ sauce, salsa NOT mayo and cheese on burgers • On the side: low-fat dressing, sour cream, gravy, sauces • With (NOT before) the meal: bread, non-water drinks, chips American Dietetic Association, If your Child is Overweight: A Guide for Parents Summary • Childhood obesity can be prevented • No one factor causes obesity and no one intervention will stop it • Physician’s most important role will be in developing sound eating and activity habits • At each well-child visit review the child’s BMI status and deliver core messages • Advocate for better school & community policies that support your well-child advice