Type A blood - Advocate Health Care
advertisement
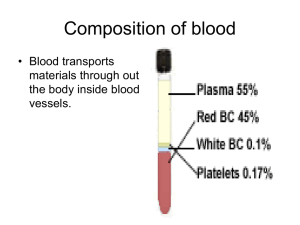
Curriculum Update: The Hematopoietic System, Patients with Special Challenges, Interventions For The Patient With Chronic Care Needs Condell Medical Center EMS System August 2006 Site Code #10-7200-E1206 Program revised by: Sharon Hopkins, RN, BSN EMS Educator Objectives Upon successful completion of this CE module, the EMS provider should be able to: discuss insults to the hematopoietic system discuss the uniqueness when caring for patients with special challenges review acute interventions necessary for the chronic care patient discuss medications used in Region X participate in case scenario review successfully complete the post quiz with a score of 80% or better Hematology Definition - the study of blood and bloodforming organs collectively known as the hematopoetic system. Prehospital care for most patients with hematological disorders is mainly supportive. Understanding some of the hematological disorders enhances EMS assessment skills Blood Cells Produced mainly in bone marrow - the spongy material in the center of bone Assistance to regulation of production, destruction and differentiation (development of a specific function) of cells carried out in the: lymph nodes spleen liver Components of Blood Plasma Platelets thrombocytes White blood cells leukocytes Red blood cells erythrocytes Components by Volume -WBC’s & platelets together form <5% of formed elements - RBC’s 95% of volume of formed elements Components of Blood 78% water 22% solids (plasma, RBC’s, WBC’s, platelets) Plasma Clear fluid part of blood; about 92% water Plasma contains various cellular materials in solution and suspension: proteins (albumin, globulins, fibrinogen) salts metals inorganic compounds Red Blood Cells (RBC’s) Erythrocytes Mainly comprised of water and hemoglobin Hemoglobin (a protein) - oxygen carrying component of the RBC; gives blood its red color; carries oxygen Primary function of RBC: transport oxygen from the lungs to various body tissue transport carbon dioxide from various tissues to the lungs Average life expectancy RBC 90-120 days Pulse Oximetry Estimates the amount of oxygen carried in the bloodstream using infrared technology across the skin White Blood Cells (WBC’s) Leukocytes Helps fight infection and aids in the immune process Helps heal wounds by ingesting matter (dead cells, tissue debris, old RBC’s) Protects the body from foreign material (antigens) Involved in the protection from mutated cells (ie: cancer) Includes: lymphocytes, monocytes, eosinophils, basophils, neutrophils Platelets - Thrombocytes Small, sticky cells Helps in blood clotting Groups together to form clumps to plug holes and leaks to stop the bleeding WBC’s, RBC’s, and platelets make up about 45% of the blood volume Plasma takes up about 55% of the blood volume More Blood Components Fat globules Chemical substances carbohydrates proteins hormones Gases including oxygen carbon dioxide nitrogen Complete Blood Count - CBC A particular and common blood test Measures the size, number, and maturity of different blood cells in a specific volume of blood Can be used to determine abnormalities in production of blood cells in destruction of blood cells Blood Groups Surfaces of RBC’s contain glycoproteins and glycolipids Based on the presence or absence of isoantigens (an antigen substance that can stimulate antibody production), we can classify blood into groups Most common blood grouping is ABO and Rh A, B, AB, and O blood types Person can be Rh+ or Rh Blood Types Type AB blood- universal recipient Can receive any of the 4 types of blood Carries both A & B antigens but does not have antibodies to A or B blood Type O blood - universal donor Can be given to patients regardless of blood type Has both anti-A & anti-B antibodies but no antigens Type A blood has A antigens & anti-B antibodies Can receive type A or O blood only Type B blood has B antigens & anti-A antibodies Can receive type B or O blood only Blood groups Rh blood groups Discovered in the blood of the rhesus monkey in 1940’s If the blood has Rh antigen they are Rh+ If the blood lacks the antigen they are Rh Rh+ & Rh- blood is incompatible; the immune system makes antibodies if mixed When a subsequent infusion of Rh+ blood is received the immune response causes a severe reaction (hemolysis - breakdown of RBC’s and release of hemoglobin) Acquired Factor Deficiencies Hemolytic disease of the newborn Arises during pregnancy Maternal and fetal blood may be incompatible if Rh factor discrepancy is present Usually the first born is unaffected Future problems in pregnancy prevented by Rhogam injections given after birth to Rhmother delivering an Rh+ baby Rhogam given to Rh- mother binds to any Rh+ antigens left by the fetus and prevent any production of antibodies by the mother that would affect future pregnancies of Rh+ baby Blood Transfusions Blood is the most easily shared human tissue Many lives are saved each year Most often used to alleviate anemia An antibody-antigen reaction can occur causing the transfused blood to hemolyze or burst The liberated hemoglobin causes kidney damage from sludging Hemostasis The sequence of clot formation that stops bleeding Quick, localized and carefully controlled Three mechanisms reduce blood loss: Vascular spasm - local vasoconstriction Platelet plug formation Blood clotting (coagulation) Failure of these mechanisms could result in hypoperfusion and shock Mechanisms of Hemostasis Vascular spasm Contraction of the smooth muscle around the injured vessel Plug formation Platelets stick to the walls (platelet adhesion) Platelets physically change to have projections that hold onto one another Enzymes released that make other platelets more sticky in the same area Mechanisms of Hemostasis Blood clotting A ruptured blood vessel exposes collagen and other structural proteins to the blood Proteins activate an enzyme reaction & certain blood proteins are changed into long fibrin strands A gelatinous mass is formed that further occludes vessel opening Clot reabsorbed by body when no longer needed General Patient Assessment Most patients with hematological problems are dealing with a chronic condition Most patients need help due to a change in their baseline condition Most care administered by EMS providers will be supportive in nature - treat the symptoms When possible, honor patient requests for hospital destination improved continuity of care have release signed if necessary (not closest) Patient Assessment Scene size-up, BSI precautions, general impression Initial assessment Assess airway, breathing, circulation, mental status (AVPU) Check for life threats common issues could include lifethreatening bleeds and massive infections with septic shock Patient Assessment cont’d Focused history and physical exam Patient categorized as: responsive or unresponsive medical patient trauma patient with significant or non-significant mechanism of injury Categorization determines which format is used to complete history and physical Patient Assessment cont’d SAMPLE history anemia - increased heart rate & respirations poor tissue oxygenation - fatigue, malaise, apprehension, confusion, change in skin color clotting problem - excessive bruising, skin discoloration infection - lymph node enlargement (swollen glands), sore throat, pain on swallowing bleeding abnormalities - nausea, anorexia, bloody vomiting or diarrhea, bleeding gums Vital signs, pulse oximetry, pain scale, EKG Patient Assessment cont’d Physical exam eye problems especially with autoimmune disorders (immune system can’t determine which tissues are self and which are not) and sickle cell anemia skin condition liver disease or hemolysis of RBC’s - jaundice polycythemia - reddish tone anemia - pale bleeding under the skin - petechia (tiny red dots), purpura (large purple blotches), bruising pruritis (itching) - excess of bilirubin prolonged bleeding of relatively minor injuries Patient Assessment cont’d GI system Low platelet counts & blood clot abnormalities epistaxis (nosebleed) is common may swallow excessive blood causing nausea and loose, dark bowel movements bleeding of the gums abdominal pain especially associated with problems of the spleen and/or liver Musculoskeletal Pain system & swelling in joints autoimmune diseases (rheumatoid arthritis), hemophilia (bleeding into joint) Patient Assessment cont’d Cardiorespiratory system Anemia dyspnea, tachycardia, chest pain Genitourinary system Hematuria - blood in the urine Heavy menstrual bleeding Frank vaginal bleeding General Treatment Airway & breathing Supplemental oxygen usually with non-rebreather Watch for dyspnea and fatigue Circulation Fluid volume replacement with crystalloid solution (ie: NS or LR) does not carry oxygen Watch for & treat dysrhythmias Comfort measures Morphine, oxygen, positioning Psychological support for patient & family Diseases of Red Blood Cells Anemias The most common disease of RBC’s Defined as a hematocrit less than 37% in women; 40% in men Sickle cell anemia = sickle cell disease Disorder in production of red cells (sickle shape when oxygen levels become low) Polycythemia Excess production in red blood cells Anemia A sign and not a disease process Bone marrow must be able to keep up with the destruction of older RBC’s to maintain adequate percentages Anemia is a significant drop in the percentage of red blood cells (RBC’s) (low hematocrit) Oxygen carrying capacity of the blood is reduced due to decrease in hemoglobin Females may temporarily decrease RBC levels during menstruation Anemia Signs and symptoms Fatigue, intolerance of cold, pale skin, dizziness, irritability, tachycardia, shortness of breath, chest pain Many actual types of anemia: Iron deficiency - inadequate iron intake Pernicious - poor absorption vitamin B12 Hemolytic - RBC’s destroyed faster than produced Aplastic - bone marrow fails to produce blood cells Sickle Cell Anemia/Disease Inherited disorder of red blood cell production RBC’s have sickle shape when oxygen levels are low; red blood cells become rigid Average sickled RBC life span 10-20 days (normal is 120 days) Generation of new RBC’s can’t keep up with the hemolysis (destruction) Blood viscosity increased sludging of blood obstruction of capillaries & small blood vessels blood flow to tissues & organs disrupted tissues & organs eventually damaged adults often have multiple organ problems cardiopulmonary, renal, neurological diseases Sickle Cell Crisis Disease not limited to 1 ethnicity but can affect many including Caucasian 3 presentations of crisis common: Vasoocclusive crisis musculoskeletal abdominal pain pain priapisms pulmonary problems renal crisis (renal infarction) central nervous system crisis (cerebral infarctions) Sickle Cell Crisis cont’d Hematological Crisis fall in hemoglobin level stagnation of red blood cells in spleen problems with bone marrow function Infectious patient crisis functionally immunosuppressed vulnerable to infection & sepsis loss of splenic function makes patient susceptible to massive bacterial infection Sickle Cell Complications Sepsis - due to immunosuppression Acute chest syndrome infection or sickled red cells trapped in lungs dyspnea, coughing, chest pain Hand-and-foot syndrome painful swelling due to severe vascular occlusion Splenic sequestration crisis accumulation of sickled cells in spleen pale, enlarged spleen, abdominal pain, shock Sickle Cell Complications cont’d Aplastic crisis severe anemia when bone marrow temporarily stops producing red blood cells pale, tired, less active than normal Stroke cerebral vascular occlusion due to sickled cells can affect any age extremity weakness, change in level of consciousness Painful episode acute and severe pain anywhere but most often hands, arms, chest, legs, feet Prehospital Care Sickle Cell Anemia/Disease Care is primarily supportive Oxygen via nonrebreather mask to increase the saturation of the circulating RBC’s - evaluate pulse oximetry IV of normal saline to hydrate patient Pain relief with analgesics larger than normal amounts of morphine are often required for pain control involve medical control for higher dosing Polycythemia Abnormally high percentage of RBC’s (high hematocrit) Rare disorder; typically in people over 50 No cure but can be treated Can be caused by: Unregulated increase in RBC production Tissue hypoxia Dehydration Blood doping - athlete training at high altitudes to increase RBC production Makes it harder to pump blood through the body because it’s thicker Increases risk of thrombosis Polycythemia Signs and symptoms Bleeding abnormalities epistaxis, Headache, spontaneous bruising, GI bleeding dizziness, blurred vision Itching Severe cases with congestive heart failure Treatment Supportive IV - O2 - monitor Hospital treatment - phlebotomy (“blood letting”) to remove excess red blood cells Diseases of White Blood Cells (WBC’s) White blood cells are body’s principal defense system against infection Problems could include: Leukopenia/neutropenia decrease in number of WBC’s Leukocytosis increase in number of circulating WBC’s could indicate: bacterial infection, rheumatoid arthritis, DKA, leukemia, pain, excercise Leukemia Lymphomas Leukemia Malignant disease (cancer) of blood forming tissue Classifications Acute lymphocytic leukemia (ALL) primarily of children and young adults Acute myelogenous leukemia (AML) primarily of older people in their 60’s and 70’s Chronic lymphocytic leukemia (CLL) primarily of older people in their 60’s and 70’s Chronic myelogenous leukemia (CML) Leukemia Common presentations: moderate to severe anemia abnormal decrease in platelets patient appears acutely ill; febrile, weak, & fatigued; lymph node enlargement; history of weight loss & anorexia; enlarged liver & spleen with abdominal tenderness; tender sternum Common complication - infection primarily due to low number of circulating neutrophils (main blood component protecting against bacterial or fungal infection) Leukemia & EMS Care Patient at risk for infection Isolation techniques (gloves and masks) to prevent spread of your germs to the patient Care primarily supportive Position of comfort Oxygen via nonrebreather mask if needed IV (fluid bolus if patient is dehydrated) Analgesics (ie: morphine) for pain Lymphomas Cancer of the lymphatic system Most prominent in the lymph nodes Malignant lyphoma classification: Hodgkin’s lymphoma 7,500 diagnosed annually in USA long-term survival better treatable with radiation, chemotherapy, or both can be curable Non-Hodgkin’s 40,000 lymphoma diagnosed annually in USA cure rate depends on type of lymphoma identified Lymphoma Presenting signs & symptoms may report fever, night sweats, anorexia, weight loss, fatigue, itching many with Hodgkin’s have no symptoms non-Hodgkin’s most commonly have swollen lymph nodes Field treatment supportive consider IV, O2, pain control necessary isolation techniques gloves & mask if Diseases of Platelets & Blood Clotting Abnormalities Thrombocytosis patients - increased platelets usually asymptomatic Thrombocytopenia easy - decrease in platelets bruising & bleeding Hemophilia absence von of protein necessary for blood clotting Willebrand’s disease inherited disease affecting both sexes excessive bleeding after injury or surgery aspirin contraindicated Hemophilia Inherited clotting deficiency Females are carriers 1 in 10,000 males have the disease Bleeding may occur spontaneously or after minor trauma Can be caused by deficiency of different clotting factors - factor VIII or factor IX Bleeding takes longer to stop because body cannot form stable fibrin clots Hemophilia Signs and symptoms numerous bruises deep muscle bruising joint bleeding - hemarthrosis Characterized by blood in the urine, bloody noses and painful, swollen joints Permanent joint damage with repeated bleeding Transfusion of specific clotting factor near time of injury may lessen the bleeding but will never make the disease go away Field Treatment Hemophilia The platelet plug is not stable but the mechanisms of vasoconstriction and platelet aggregation will still occur Patients may have prolonged bleeding and possible rebleeding IV - O2 via nonrebreather- monitor Ice application Superficial injuries - patience & pressure If joint injury, splinting will reduce pain Transport to ED necessary for replacement of deficient factor Other Hematopoietic Disorders Disseminated intravascular coagulation - DIC Disorder of coagulation High mortality rate Most commonly results from: sepsis, hypotension, obstetric complications, severe tissue injury, brain injury, cancer, major hemolytic blood transfusion reactions Fibrin clots formed throughout circulation instead of just at the affected area of need Simultaneous clotting and bleeding Patient experiences widespread thrombosis and end-organ ischemia DIC Signs & symptoms Oozing blood at venipuncture and wound sites Purpuric rash often over chest and abdomen Minute hemorrhages just under skin Prehospital care Supportive and focused on symptoms IV - O2- monitor Patient often hemodynamically unstable Hospital treatment Fresh frozen plasma & platelets at hospital Additional Hematopoietic Disorders Multiple Cancer myeloma disorder of plasma cells (cells that produce antibodies) Rarely found in persons under 40 Approximately 14,000 new cases every year Cancer plasma cells overcrowd healthy cells with a reduction in blood cell production Patient becomes anemic and is prone to infection Multiple Myeloma Signs & symptoms Pain in back or ribs Diseased marrow weakens bones and pathological fractures occur (fractures with minimal or no trauma) Fatigue Risk for bleeding due to decrease in platelets Renal failure from elevated calcium levels Increased risk for infection due to a lack of certain antibody secretion Multiple Myeloma Treatment Prehospital care Supportive IV if signs of dehydration Pain control - disease can be painful and pain in presence of pathological fractures Hospital care Chemotherapy Radiation Bone marrow transplants What Is Bone Marrow? Tissue in the center of large bones where new blood cells are produced 2 types of stem cells produced hematopoietic stem cells - forms blood cells: WBC’s - leukocytes RBC’s - erythrocytes platelets - thrombocytes stromal stem cells - mix of cells to generate: fat cartilage bone can differentiate into many kinds of tissue (ie: nervous) Bone Marrow Bone Marrow Transplant Pioneered in 1970 Transplant of hematopoietic stem cells Most often done for life-threatening diseases of blood or bone marrow acute lymphocytic leukemia acute myelogenous leukemia aplastic anemia chronic myelogenous leukemia Hodgkin’s and non-Hodgkin’s diseases multiple myeloma radiation poisoning Types of Bone Marrow Transplant Autologous bone marrow transplant stem cells obtained months in advance of use stem cells isolated from patient; stored in freezer; patient treated to destroy remaining stem cells; harvested stem cells reinfused Allogenic bone marrow transplant involves donor & recipient; must match tissue type recipient requires immunosuppressant drugs donor bone marrow harvested under general anesthesia (>100 needle sticks in large bone) Bone Marrow Transplant Cont’d Peripheral blood stem cell process - apheresis donor blood withdrawn via needle; blood passes thru machine to remove WBC’s; RBC’s returned to donor; WBC stem cells can be stored frozen recipient gets injection to boost stem cell yield Cord blood donation of umbilical cord & placenta after infant delivered cord blood yields higher concentration of stem cells but limited volume (50 ml - 2 T) usually transplanted into children, not adults cord blood can be stored frozen for years Bone Marrow Infusion Stem cells (bone marrow transplant) given IVPB stem cells circulate in the blood stream stem cells migrate into bone marrow spaces stem cells grow & start to produce new blood cells takes several weeks to grow enough new cells Bone marrow transplant mortality rate is high - 10% reserved for life-threatening conditions Case Scenario #1 Your 22 year-old patient with hemophilia presents after falling off his motorcycle at low speed. There are some minor abrasions over the extremities and the patient complains of pain and swelling to the left elbow. Vital signs: B/P 132/70; P - 96; R - 18 What is the order of the assessment steps to take? What interventions are necessary? Case Scenario #1 Assessment steps Scene size-up, BSI, general impression Initial assessment ABC’s, AVPU, check for life threats Focused history & physical exam trauma without significant mechanism of injury perform a head-to-toe SAMPLE, vital signs, pulse ox, pain scale Case Scenario #1 Interventions Manual c-spine control Follow SOP “Spinal clearance, In-field” evaluate mechanism of injury, signs & symptoms, patient reliability IV-O2-monitor as applicable Application of ice Splinting of injured/swollen extremities will help with pain control Direct pressure for bleeding wounds Case Scenario #2 Your 65 year old patient undergoing treatment for leukemia calls for transport. What is a common complication for this group of patients? What method of infectious control needs to be exercised by the EMS responders? Case Scenario #2 A common complication for patients with leukemia is infection primarily due to the low number of circulating neutrophils (WBC component responsible for protecting against bacterial and fungal infection) BSI’s necessary for providers to wear include gloves mask