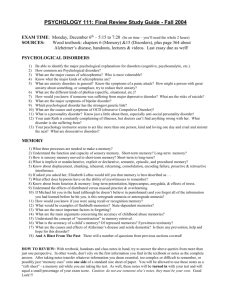
anxiety disorders
advertisement

Myers’ Psychology for AP* Unit 12: Abnormal Psychology David G. Myers Some PowerPoint Presentation Slides by Kent Korek Germantown High School Worth Publishers, © 2010 *AP is a trademark registered and/or owned by the College Board, which was not involved in the production of, and does not endorse, this product. OBJECTIVES: The student will know and understand the Psychological Disorders investigates patterns of behavior that are considered deviant or distressful in our culture and includes how psychologists diagnose these patterns. After completing their study of this chapter, students should be able to: 1)identify the criteria for judging whether behavior is psychologically disordered. 2) Describe the medical model of psychological disorders, and discuss the bio-psycho-social perspective offered by critics of this model 3) Describe the aims of DSM-IV, and discuss the potential dangers associated with the use of diagnostic labels. 4) Describe the symptoms of generalized anxiety disorder, phobias, and obsessive-compulsive disorder. 5) Explain the development of anxiety disorders from both a learning and a biological perspective. 6) Describe major depressive disorder and bipolar disorder. 7) Explain the development of mood disorders, paying special attention to the biological and social-cognitive perspectives. 8)Describe the characteristics and possible cause of dissociative identity disorder. 9) Describe the various symptoms and types of schizophrenia, and discuss research on its causes. 10) Describe the nature of personality disorders, focusing on the characteristics of the antisocial personality disorder. 11) Describe the prevalence of various disorders and the timing of their onset. Unit 12: Abnormal Psychology Unit Overview • • • • • • • • Perspectives on Psychological Disorders Anxiety Disorders Somatoform Disorders Dissociative Disorders Mood Disorders Schizophrenia Personality Disorders Rates of Disorder Introduction • How should we define psychological disorders? • How should we understand disorders? • How should we classify psychological disorders? Normal or Abnormal? Not easy task: *Is Robin Williams normal? Anna Nicole Smith? Marilyn Manson? Karl Rove? *Is a soldier who risks his life or her life in combat normal? *Is a grief-stricken woman unable to return to her routine three months after her husband died normal? Is a man who climbs mountains as a hobby normal? Some abnormalities are easy: Hallucinations (false sensory experiences) Delusions (extreme disorders of thinking) Affective problems (emotion: depressed, anxious, or lack of emotion) CORE CONCEPT: Medical model: takes a “disease” view Psychology model: interaction of biological, mental, social, and behavioral factors According to a study conducted by the National Institute of mental health: *15.4% of the population suffers from diagnosable mental health problems *56 million Americans meet the criteria for a diagnosable psychological disorder (Carson, 1996, Regier 1993). *Over the lifespan, +/- 32% of Americans will suffer from some psychological disorder (Regier, 1988). 1 in 5 in the U. S. in a given year (Allaboutdepression.com,1993). 1 in 4 n the world- 450 million people (WHO.int.com, 2001). SHOW: Psych in Film, Ver.2, #33, Patch Adams Perspectives on Psychological Disorders Defining Psychological Disorders • Psychological disorders –Deviant behavior –Distressful behavior –Harmful dysfunctional behavior • Definition varies by context/culture • Attention deficit hyperactivity disorder (ADHD) Understanding Psychological Disorders The Medical Model • Philippe Pinel-French physician who was instrumental in the development of a more humane psychological approach to the custody and care of psychiatric patients, referred to today as moral therapy. • He also made notable contributions to the classification of mental disorders and has been described by some as "the father of modern psychiatry". • An 1809 description of a case that Pinel recorded in the second edition of a textbook on insanity is regarded as the earliest evidence for the existence of the form of mental disorder known as dementia praecox or schizophrenia in the 20th century. Historical Perspective Perceived Causes *movements of sun or moon *lunacy- full moon *demons & evil spirits Ancient Treatments *exorcism, caged like animals, beaten, burned, castrated, mutilated, blood replaced with animal’s blood Historical Perspective Hippocrates (400 bc) *first step in scientific view of mental disturbance. *imbalance (excess) among four body fluids called “humors” Humors Origin Temperament Blood heart sanguine (cheerful) Choler (yellow bile) liver choleric (angry) Melancholer spleenmelancholy (depressed) (black bile) Phlegm brain phlegmatic (sluggish) Psychological Disorders Medical Model *concept that diseases have physical causes *can be diagnosed, treated, and in most cases, cured *assumes that these “mental” illnesses can be diagnosed on the basis of their symptoms and cured through therapy, which may include treatment in a psychiatric hospital Understanding Psychological Disorders The Biopsychosocial Approach • Interaction of nature and nurture • Influence of culture on disorders The Biopsychosocial Approach to Psychological Disorders Psychological Disorders Biological (Evolution, individual genes, brain structures and chemistry) Sociocultural (Roles, expectations, definition of normality and disorder) Bio-psycho-social Perspective *assumes that biological, sociocultural, and psychological factors combine and interact to produce psychological disorders Psychological (Stress, trauma, learned helplessness, mood-related perceptions and memories) Origins of the Diagnostic and Statistical Manual: Mental Disorders • United States was the recording of the frequency of "idiocy/insanity" in the 1840 census. By the 1880 census, seven categories of mental health were distinguished: mania, melancholia, monomania, paresis, dementia, dipsomania, and epilepsy. • The American Psychiatric Association Committee on Nomenclature and Statistics developed a variant of the ICD-6 that was published in 1952 as the first edition of Diagnostic and Statistical Manual: Mental Disorders (DSM-I). Classifying Psychological Disorders • Diagnostic and Statistical Manual of Mental Disorders (DSM) –DSM-IV-TR –DSM-5 • International Classification of Diseases (ICD-10) Classifying Psychological Disorders Classifying Psychological Disorders Classifying Psychological Disorders Classifying Psychological Disorders Classifying Psychological Disorders Classifying Psychological Disorders Psychological Disorders- Etiology DSM-V *American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) *a widely used system for classifying psychological disorders *Prior to last May we used the DSM-IV-TR (text revision. Now we use the DSM V *today used as “convenient shorthand” to avoid labeling. DSM-IV-TR organizes each psychiatric diagnosis into five levels (axes) relating to different aspects of the disorder or disability: 1) Axis 1 -- Clinical disorders including major mental disorders, as well as developmental or learning problems. Common disorders in this category include depression, bipolar, anxiety, ADHD, and schizophrenia. 2) Axis 2 -- Pervasive or personality disorders, including mental retardation. Common disorders in this category include borderline PD, schizotypal PD, narcissistic PD, antisocial PD, paranoid PD. DSM-IV-TR continued: 3) Axis 3 -- Acute medical conditions and physical disorders. Common disorders in this category include brain trauma, brain injury, brain disease.. 4) Axis 4 -- Psychosocial and environmental factors contributing to the disorder. Common factors in this category include a man suffering from depression after losing his job, or his wife dying, et. al. 5) Axis 5 -- Global Assessment of Functioning or Children’s Global Assessment Scale (under 18) David Rosenhan suspected that terms such as sanity, insanity, schizophrenia, mental illness, and abnormal might have fuzzier boundaries that the psychiatric community thought. He also suspected that some strange behaviors seen in mental patients might originate in the abnormal atmosphere of the mental hospital, rather than the patients themselves. Education ・AB, Yeshiva College, 1951 ・MA, Columbia University, 1953 ・PhD (psychology), Columbia University, 1958 Professor, Stanford University Dangers of Labeling David Rosenhan Being Sane in Insane Places In 1973 sociologist David Rosenhan designed a clever study to examine the difficulty that people have shedding the "mentally ill" label. He was particularly interested in how staffs in mental institutions process information about patients. Rosenhan & seven associates had themselves committed to different mental hospitals complaining of hearing voices. All but one were diagnosed as schizophrenic. •Once admitted, they acted totally normal. •Remained hospitalized for average 19 days (9 to 52) •Only the patients detected their sanity •When discharged their chart read, “schizophrenia in remission” No professional staff member at any of the hospitals ever realized that any of Rosenhan’s pseudopatients was a fraud. Failure to detect sanity during the course of hospitalization may be due to the fact that physicians operate with a strong bias toward what statisticians call the Type 2 error [5]. This is to say that physicians are more inclined to call a healthy person sick (a false positive, Type 2) than a sick person healthy (a false negative, Type 1). The reasons for this are not hard to find: it is clearly more dangerous to misdiagnose illness than health. Better to err on the side of caution, to suspect illness even among the healthy. Power of labels Preconception can stigmatize Insanity label-mental illness of such a severe nature that a person cannot distinguish fantasy from reality, cannot conduct her/his affairs due to psychosis, or is subject to uncontrollable impulsive behavior. Insanity is a concept discussed in court to help distinguish guilt from innocence Stereotypes of the mentally ill Self-fulfilling prophecy Psychological Disorder – a “harmful dysfunction” in which behavior is judged to be: • atypical- (not enough in itself) • disturbing- (varies with time & culture) • maladaptive- (harmful) • unjustifiable- (sometimes there’s a good reason) Show THE WORLD OF AbNORMAL BEHAVIOR: #1 Looking at Abnormal Behavior #2 The Nature of Stress Carol D. Ryff argues that we must define mental illness in terms of the positive. She names 6 core dimensions: 1) Self-acceptance: positive attitude towards self multiple aspects of self positive about past life 2) Positive self relations with other people: warm, trusting, satisfying interpersonal relationships capable of empathy, affection, intimacy 3) Autonomy independent, self-determined able to resist social pressures 4) Environmental mastery: sense of mastery and competence makes good use of opportunities creates contexts that support their personal needs 5) Purpose of Life: has goals and directedness feels there is meaning to past and present life 6) Personal Growth: see oneself as growing and expanding open to new experiences change in ways that reflect self-knowledge and effectiveness Psychological Disorders- Etiology Neurotic disorder (term seldom used now) *usually distressing but that allows one to think rationally and function socially *Freud saw the neurotic disorders as ways of dealing with anxiety Psychotic disorder *person loses contact with reality *experiences irrational ideas and distorted perceptions PREPAREDNESS HYPOTHESIS: Suggests that we have an innate biological tendency, acquired through natural selection, to respond quickly and automatically to stimulti that posed a survival threat to our ancestors. (Ohman & Mineka, 2001) This explains why we develop phobias for snakes and lightening more easily than others. •ANXIETY DISORDERS •MOOD DISORDERS •DISSOCIATIVE DISORDERS •SCHIZOPHRENIA •PERSONALITY DISORDERS •BIOPSYCHOSOCIAL DISORDERS •SUBSTANCE ABUSE DISORDERS •SEXUAL DISORDERS •DEVELOPMENTAL (CHILDHOOD) DISORDERS Anxiety Disorders 1) PANIC DISORDER w/AGORAPHOBIA 2) GENERALIZED ANXIETY DISORDER 3) PHOBIAS a) simple b) social c) agoraphobia 4) 5) POST TRAUMATIC STRESS DISORDER (PTSD) 6) STOCKHOLM SYNDROME 7) SOMOTOFORM a) hypochondria b) conversion (hysteria) Anxiety Disorders • Anxiety disorders –Generalized anxiety disorder –Panic disorder –Phobia –Obsessive-compulsive disorder –Post-traumatic stress disorder Anxiety Disorders Anxiety Disorders *distressing, persistent anxiety or maladaptive behaviors that reduce anxiety Panic Disorder • Panic disorder = an anxiety disorder marked by unpredictable minutes-long episodes of intense dread in which a person experiences terror and accompanying chest pain, choking, or other frightening sensations. –Panic attacks Anxiety Disorders 1) Panic Disorder *marked by a minutes-long episode of intense dread in which a person experiences terror and accompanying chest pain, choking, racing heart, sweating, musclespasms, or other frightening sensations *common thinking patterns include: "I’m losing control.....” "I feel like I’m going crazy.....” "I must be having a heart attack.....” "I’m smothering and I can’t breathe.....” 1a) Panic Disorder w/Agoraphobia *fear of leaving home for fear of having a panic attack Generalized Anxiety Disorder • Generalized anxiety disorder = an anxiety disorder in which a person is continually tense, apprehensive, and in a state of autonomic nervous system arousal. *2/3 women *Free floating anxiety = a generalized, persistent, pervasive fear that is not attributable to any specific object, event, or source. 2) Generalized Anxiety Disorder person is tense, apprehensive, and in a state of autonomic nervous system arousal *Chronic (6 months) unrealistic or excessive worry about 2 or more elements in one’s life. SHOW: Psych in Film, Ver 2, #24, Apollo 13 Phobias • Phobias = an anxiety disorder marked by a persistent, irrational fear and avoidance of a specific object, activity, or situation. –Specific phobia –Social phobia –Agoraphobia 3) Phobias a) Simple Excessive, irrational fear of objects or situations b) Social Persistent fear of scrutiny by others doing something humiliating (stage fright or speech phobia) c) Agoraphobia Fear of being in a place or situation with no escape. (childhood environments in which one did not feel safe) Anxiety Disorders Phobias persistent, irrational fear of a specific object or situation Ablutophobia: washing, bathing Genophobia: sex Acrophobia: heights Gynephobia: women Algophobia: pain Ichthyophobia: fish Arachibutyrophobia: peanut butter sticking to roof of mouth Lutraphobia: otters Caligynephobia: beautiful women Medorthophobia: erect penis Cleptophobia: stealing Parthenophobia: virgins Demophobia: crowds Pophyrophobia: color purple Ecclesiophobia: church Somniphobia: sleep Ergophobia: work Testophobia: taking a test Macrophobia: long waits Anxiety Disorders Common and uncommon fears 100 Percentage 90 of people 80 surveyed 70 60 50 40 30 20 10 Snakes Being Mice Flying Being SpidersThunderBeing Dogs Driving Being Cats in high, on anclosed in, and and alone a car In a 0 exposed airplane in a insectslightning In a crowd places Afraid of it small house place at night Bothers slightly Not at all afraid of it of people Phobias Phobias Obsessive-Compulsive Disorder • Obsessive-compulsive disorder = an anxiety disorder characterized by unwanted repetitive thoughts (obsessions) and/or actions (compulsions). –An obsession versus a compulsion –Checkers –Hand washers Obsessive Compulsive Spectrum Disorders Obsessive-Compulsive Disorder *unwanted repetitive thoughts (obsessions) and/or actions (compulsions) *feel obsessed w/something they do not want to think about and/or compelled to carry out some action, often pointlessly ritualistic. New DSM V Disorders Hoarding Disorder, Excoriation (skin-picking) Disorder, Substance or Medication Induced OCD, and OCD due to another medical condition Obsessive Compulsive Disorders *1 in 50 adults has OCD *Exact pathophysiologic process that underlies OCD has not been established. *Research suggests that abnormalities in serotonin (5-HT) transmission in the central nervous system are central to this disorder. *Supported by the efficacy of specific serotonin reuptake inhibitors (SSRIs) in the treatment of OCD. OCD Common Obsessions and Compulsions Among People With Obsessive-Compulsive Disorder Thought or Behavior Percentage* Reporting Symptom Obsessions (repetitive thoughts) Concern with dirt, germs, or toxins 40 Something terrible happening (fire, death, illness) 40 Symmetry order, or exactness 24 Compulsions (repetitive behaviors) Excessive hand washing, bathing, tooth brushing, or grooming 85 Repeating rituals (in/out of a door, up/down from a chair) Checking doors, locks, appliances, car brake, homework 51 46 Obsessive-Compulsive Disorder OCD • PET Scan of brain of person with Obsessive/ Compulsive disorder • High metabolic activity (red) in frontal lobe areas involved with directing attention Good examples of obsessions and their closely related compulsions: Obsession: A young woman is continuously terrified by the thought that cars might careen onto the sidewalk and run over her. Obsession: A mother tormented by concern that she might inadvertently contaminate food as she cooks dinner. Compulsion: Every day she sterilizes all cooking utensils in boiling water and wears rubber gloves when handling food Compulsion: She always walks as far from the street pavements as Obsession: A woman cannot rid herself of the thought that she might possible and wears red accidentally leave her gas stove turned clothes so that she will on, causing her house to explode be immediately visible to an out-of-control car. Compulsion: Every day she feels the irresistible urge to check the stove exactly 10 times before leaving for work. Post-Traumatic Stress Disorder • Post-traumatic stress disorder characterized by haunting memories, nightmares, social withdrawal, jumpy anxiety, and/or insomnia that lingers for four weeks or more after a traumatic experience. – PTSD – “shellshock” or “battle fatigue” – Not just due to a war situation • Post-traumatic growth = positive psychological changes as a result of struggling with extremely challenging circumstances and life crises. Post Traumatic Stress Disorder (PTSD) Follows a psychologically distressing event that is outside the normal experience (rape, war, murder, beatings, torture, natural disasters) *1 in 12 adults in the U.S. suffer from PTSD *incessant reliving of event, recurring dreams, intrusive memories, flashbacks, intensive fears, sleep problems. Perpetration-induced traumatic stress (PITS) *soldiers who had killed in combat were found to suffer higher rates of PTSD than other troops *lasting biological effects: causes the brain’s hormone- *other studies include grief, survivor’s guilt, fear regulating system to develop hair-trigger responsiveness p341 Zim SHOW: Psych in Film, Ver 2, #23, Deer Hunter 6) Stockholm Syndrome *captor threatens to kill and is able to do so *victim cannot escape or life depends on the captor *victim is isolated from outsiders *captor is perceived as showing some degree of kindness *victim denies anger at abuser & focuses on good qualities Example of this disorder would be Francine Hughes (The Burning Bed) Francine set fire to her *”fight or flight” reactions are inhibited husband while he was asleep after years of *victim fears interference by authorities--fears repeated physical and the captor will return from jail mental abuse. *victim is grateful to abuser for sparing her life Somatoform Disorders Somatoform disorders • Mental illnesses that cause bodily symptoms, including pain. The symptoms can't be traced back to any physical cause. And they are not the result of substance abuse or another mental illness. • People with somatoform disorders are not faking their symptoms. The pain and other problems they experience are real. Somotoform Disorders Disorders, involving physical complaints for which no organic basis can be found. 1. Hypochondria Fear of having serious disease where no evidence of illness can be found. 2. Conversion disorder. This condition strikes when people have neurological symptoms that can't be traced back to a medical cause. For example, patients may have symptoms such as: paralysis blindness hearing loss SHOW: Psych in Film, ver 2, #29, Freud (therapy) Somatoform Disorders • 3. Somatization disorder. This is also known as Briquet's syndrome. Patients with this type have a long history of medical problems that starts before the age of 30. • The symptoms involve several different organs and body systems. The patient may report a combination of: • pain • neurologic problems • gastrointestinal complaints • sexual symptoms 4. Body Dysmorphic Disorder. • People with this disorder are obsessed with -- or may exaggerate -- a physical flaw. Patients may also imagine a flaw they don't have. • The worry over this trait or flaw is typically constant. It may involve any part of the body. Patients can be obsessed with things such as wrinkles, hair, or the size or shape of the eyes, nose, or breasts. 5. Pain Disorder • People who have pain disorder typically experience pain that started with a psychological stress or trauma. • Continue reading below... • For example, they develop an unexplained, chronic headache after a stressful life event. Understanding Anxiety Disorders The Learning Perspective • Fear conditioning –Stimulus generalization –Reinforcement • Observational learning Understanding Anxiety Disorders The Biological Perspective • Natural selection • Genes – Anxiety gene – Glutamate • The Brain – Anterior cingulate cortex- resembles a "collar" surrounding the frontal part of the corpus callosum. It is also involved in rational cognitive functions, such as reward anticipation, decision-making, empathy, impulse control, and emotion. TREATMENTS: *Medical model: antianxiety drugs (valium, librium, xanax), SSRIs (OCD), Ritlin (ADHD) *Psychoanalysis: observational learning, childhood (mom/dad), free association, resistance (transference), hypnosis *Learning Theories: classical conditioning, counterconditioning, systematic desensitization (phobias) *Behaviorists: principles of learning, aversive conditioning, operant conditioning (token economy) *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. Show THE WORLD OF AbNORMAL BEHAVIOR: #3 The Anxiety Disorders MOVIES The Burning Bed (Stockholm Synd) Ordinary People (PTSD) The Aviator (OCDPD) Mood Disorders (Affective Disorders) Mood Disorders • Mood disorders = psychological disorders characterized by emotional extremes. – Major depressive disorder – Persistent Depressive Disorder-chronic major depressive disorder and the previous dysthymic disorder. – Premenstrual Dysphoric Disorder – SEASONAL AFFECTIVE DISORDER (SAD) – Bipolar disorder – Disruptive Mood Dysregulation Disorderchildhood Bipolar – Cyclothmia Mood Disorders Mood Disorders characterized by emotional extremes 1) Depressive Disorders *most common disorders” a mood disorder in which a person, for no apparent reason, experiences two or more weeks of depressed moods, feelings of worthlessness, and diminished interest or pleasure in most activities a) Major Depressive Disorder Unhappy for 2 weeks without reason, appetite changes, insomnia, inability to concentrate, worthlessness, hallucinations b) Persistent Depressive DisorderUnhappy for over 2 years Major Depressive Disorder • Major depressive disorder –Lethargy –Feelings of worthlessness –Loss of interest in family and friends –Loss of interest in activities Major Depressive Disorder • • • • • • • • • Persistent Depressive Disorder Formerly known as Dysthymic Disorder (also known as dysthymia) The essential feature of persistent depressive disorder (dysthymia) is a depressed mood that occurs for most of the day, for more days than not, for at least 2 years (at least 1 year for children and adolescents). Individuals with persistent depressive disorder describe their mood as sad or “down in the dumps.” During periods of depressed mood, at least two of the following six symptoms from are present. Poor appetite or overeating Insomnia or hypersomnia Low energy or fatigue Low self-esteem Poor concentration or difficulty making decisions Feelings of hopelessness Seasonal Affective disorder (SAD) • A type of depression that's related to changes in seasons — SAD begins and ends at about the same times every year. If you're like most people with SAD, your symptoms start in the fall and continue into the winter months, sapping your energy and making you feel moody. • Treatment for SAD may include light therapy (phototherapy), psychotherapy and medications. Symptoms of major depression may be part of SAD, such as: • Feeling depressed most of the day, nearly every day • Feeling hopeless or worthless • Having low energy • Losing interest in activities you once enjoyed • Having problems with sleeping • Experiencing changes in your appetite or weight • Feeling sluggish or agitated • Having difficulty concentrating • Having frequent thoughts of death or suicide • Fall and winter SAD • Symptoms specific to winter-onset SAD, sometimes called winter depression, may include: • Irritability • Tiredness or low energy • Problems getting along with other people • Hypersensitivity to rejection • Heavy, "leaden" feeling in the arms or legs • Oversleeping • Appetite changes, especially a craving for foods high in carbohydrates • Weight gain Premenstrual Dysphoric D/O (PMDD) • • • • • • • • • • • • In most menstrual cycles during the past year, five (or more) of the following symptoms occurred during the final week before the onset of menses, started to improve within a few days after the onset of menses, and were minimal or absent in the week postmenses, with at least one of the symptoms being either (1), (2), (3), or (4): (1) marked affective liability (e.g., mood swings; feeling suddenly sad or teaful or increased sensitivity to rejection) (2) marked irritability or anger or increased interpersonal conflicts (3) markedly depressed mood, feelings of hopelessness, or self-deprecating thoughts (4) marked anxiety, tension, feelings of being “keyed up” or “on edge” (5) decreased interest in usual activities (e.g., work, school, friends, hobbies) (6) subjective sense of difficulty in concentration (7) lethargy, easy fatigability, or marked lack of energy (8) marked change in appetite, overeating, or specific food cravings (9) hypersomnia or insomnia (10) a subjective sense of being overwhelmed or out of control (11) other physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “bloating,” weight gain Mood Disorders Bipolar Disorder *a mood disorder in which the person alternates between the hopelessness and lethargy of depression and the overexcited state of mania *formerly called manic-depressive disorder a) Manic Episode a mood disorder marked by a hyperactive, wildly optimistic state, excessive excitement, silliness, poor judgment, abrasive, rapid flight of ideas b) Major depression Lethargic, sleepy, social withdrawal, irritability Symptoms of Mania 1) Mood or emotional symptoms: euphoric, expansive, and elevated. In some cases, dominant mood is irritability. Even when euphoric, manic people are close to tears and if frustrated, will burst out crying. 2) Grandiose cognition: manics believe no limits to their abilities and do not recognize the painful consequences of trying to carry out their plans. May be delusional about themselves. •Between .6 and 1.1 percent of U.S. population will have bipolar disorder in their lifetime. •It affects both sexes equally. 3) Motivational symptoms: hyperactivity has intrusive, dominating, domineering quality. Some •Onset is sudden. engage in compulsive gambling, reckless driving, •First episode promiscuity, or poor financial investment. 4) Physical symptoms: lessened need for sleep. After a few days, exhaustion settles in. occurs between ages 20 and 30. Manic Episode • • • • • • • • A period of at least one week during which the person is in an abnormally and persistently elevated or irritable mood. The person may instead be predominately irritable. This period of mania must be marked by three of the following symptoms to a significant degree. If the person is only irritable, they must experience four of the following symptoms. Inflated self-esteem or grandiosity (ranges from uncritical self-confidence to a delusional sense of expertise). Decreased need for sleep. Intensified speech (possible characteristics: loud, rapid and difficult to interrupt, a focus on sounds, theatrics and self-amusement, non-stop talking regardless of other person’s participation/interest, angry tirades). Rapid jumping around of ideas or feels like thoughts are racing. Distractibility (attention easily pulled away by irrelevant/unimportant things). Increase in goal-directed activity (i.e. excessively plans and/or pursues a goal; either social, work/school or sexual) or psychomotor agitation (such as pacing, inability to sit still, pulling on skin or clothing). Excessive involvement in pleasurable activities that have a high risk consequence. Hypomanic Episode • A is very similar to a manic one, but less intense. It is only required to persist for 4 days and it should be observable by others that the person is noticeably different from his or her regular, nondepressed mood and that the change has an impact on his or her functioning. Disruptive Mood Dysregulation Disorder (DMDD) • The defining characteristic in children is a chronic, severe and persistent irritability. This irritability is often displayed by the child as a temper tantrum, or temper outburst, that occur frequently (3 or more times per week). • When the child isn’t having a temper outburst, they appear to be in a persistently irritable or angry mood, present most of the day, nearly every day. • “Far beyond temper tantrums, DMDD is characterized by severe and recurrent temper outbursts that are grossly out of proportion in intensity or duration to the situation.” Understanding Mood Disorders • Many behavioral and cognitive changes accompany depression • Depression is widespread • Compared with men, women are nearly twice as vulnerable to major depression • Most major depressive episodes self-terminate • Stressful events related to work, marriage and close relationships often precede depression • With each new generation, depression is striking earlier and affecting more people Understanding Mood Disorders The Biological Perspective • Genetic Influences –Mood disorders run in families • Heritability • Linkage analysis • The depressed brain • Biochemical influences –Norepinephrine and serotonin Understanding Mood Disorders The Biological Perspective PET scans show that brain energy consumption rises and falls with emotional swings Mood Disorders-Depression Understanding Mood Disorders The Social-Cognitive Perspective • Negative Thoughts and Moods Interact –Self-defeating beliefs • Learned helplessness • Overthinking –Explanatory style • Stable, global, internal explanations Understanding Mood Disorders Explanatory Style Understanding Mood Disorders The Social-Cognitive Perspective • Depression’s Vicious Cycle –Stressful experience –Negative explanatory style –Depressed mood –Cognitive and behavioral changes Understanding Mood Disorders The Vicious Cycle of Depression The vicious cycle of depression can be broken at any point Biopsychosocial Approach to Depression Aaron Beck is called the FATHER OF COGNITIVE THERAPY He believed that: •depressed people draw illogical conclusions about themselves. Aaron Temkin Beck (1921-?) Professor, Univ Pennsylvania PhD: Brown, •Created the BECK Yale SCALES for labeling clinical depression. Beck believed that depressed people blame themselves for normal problems and consider every minor failure a catastrophe. Depressive Triad- negative thoughts about themselves, the world and their future. Aaron Beck’s work with depressed patients convinced him that depression is primarily a disorder of thinking rather than of mood. He argued that depression can best be described as a cognitive triad or negative thoughts about oneself, the situation or the future. Cognitive errors included the following: 1) overgeneralizing: drawing global conclusions about worth, ability, or performance on basis of single fact 2) Selective abstraction: focusing on one insignificant detail and ignoring others 3) Personalization: incorrectly taking responsibility for events in the world 4) Magnification & minimization: bad events magnified and good events minimized. 5) Arbitrary inference: drawing conclusions without sufficient evidence 6) Dichotomous thinking: seeing everything in one extreme or its opposite. Mood Disorders-Depression Brain chemistry Cognition Mood Altering any one component of the chemistrycognition-mood circuit can alter the others Generally speaking, a deficit of serotonin is associated with depression. Mood Disorders-Depression Percentage of observations 35% 30 25 20 15 Negative behaviors Positive behaviors Self-ratings A happy or depressed mood strongly influences people’s ratings of their own behavior EXAMPLES of Mood Disorders: Andrea Yates: postpartum depression and the insanity plea. It has been suggested that at the far end of the postpartum psychological spectrum lie postpartum psychosis. In Andrea’s case, it represented a state of mind in which killing one’s children seemed the best way to protect them. Harrison Ford: depression Richard Dreyfuss: bipolar disorder Abraham Lincoln: Brittany Spears: post-partum depression and bipolar disorder depression (melancholia) Drew Carey: Jim Carrey: depression suicidal (twice) Mood Disorders-Suicide Increasing rates of teen suicide 12% Suicide rate, ages 15 to 19 10 (per 100,000) 8 6 4 2 0 1960 1970 1980 Year 1990 2000 REASONS for suicide: 1) Unendurable psychological pain: if you reduce the pain just a little, most suicidal people will choose to live. 2) Frustrated psychological needs: (security, achievement, trust, friendship) 3) Search for a solution: Suicide is never done without purpose --“How do I get out of this?” 4) Attempt to end consciousness: goal is to stop awareness of painful existence. 5) Helplessness & hopelessness: loss of power 6) Constriction of options: Not seeing the broad picture; limited options. 7) Ambivalence: Some is normal--In typical case, victim cuts throat and calls for help. 8) Communication of intent: 80 percent gives clear clues to family & friends 9) Departure: quitting job, running away from home, leaving spouse are all departures but suicide is the ultimate departure. 10) Lifelong coping patterns: look for earlier episodes--often a style of problem solving that is characterized as “cut and run.” LONELINESS Sharon Brehm reports that gender interacts with marital status in the following ways: •Married females report greater loneliness than do married males •Among those never married, males report more loneliness than do females •Among the separated and divorced, males report greater loneliness than do females •Among those whose spouse has died, males report greater loneliness than do females. REASONS for Loneliness 1) Being unattached 2) Alienation: being misunderstood & feeling different 3) Being alone: coming home to empty house 4) Forced isolation: hospitalized or housebound 5) Dislocation: starting new job or school Four major strategies in coping with Loneliness: 1) Sad passivity: sleeping, drinking, overeating, watching TV 2) Social contact: calling friend 3) Active solitude: studying, reading, exercising, going to movie 4) Distractions: spending money, going shopping DRUG TREATMENTS for Depression: Monoamine oxidase inhibitors (MAOIs)- first type of antidepressant developed. brain. MAOIs prevent the removal of removing the neurotransmitters norepinephrine, serotonin and dopamine from the brain., which makes more of these brain chemicals available Diet restrictions because they can cause dangerously high blood pressure *Tricyclic antidepressants: *first to be used--not used as much today. *affect 2 neurotransmitters: norepinephrine & serotonin *side affects: drowsiness & weight gain, increased heart rate, decrease in blood pressure, blurred vision, dry mouth, confusion *SSRI (Selective Serotonin Reuptake Inhibitor) *side effects: nausea, diarrhea, tremors, weight loss, headache *less likely to affect the heart *some people feel more agitated and anxious on SSRIs, and can become increasingly suicidal if not detected and treated. For extreme Depression-Electroconvulsive therapy (ECT) uses small amounts of electricity applied to the scalp to affect neurotransmitters in the brain. TREATMENTS: *Medical model: For bipolar-- lithium carbonate, carbamazepine, and valproate. For depression--tricyclics; the newer selective serotonin re-uptake inhibitors (SSRIs), and monoamine oxidase inhibitors (MAO inhibitors). *Psychoanalysis :unconscious conflicts, intrapscyhic structures *Learning Theories: Observational learning and socaiil roles *Behaviorists: Counterconditoning *Cognitive Therapies: interpersonal therapy (Beck Scales) *Humanistic: client-centered therapies, responsibility, active-listening, emotional support and assistance in recognizing signs of relapse to avert a full-blown episode Show THE MIND #31 Mood Disorders: Mania & Depression #32 Mood Disorders: Hereditary Factors #33 Mood Disorders: Medication and Talk Therapy And THE WORLD OF AbNORMAL PSYCHOLOGY: #8 Mood Disorders Dissociative Disorders Dissociative Disorders Dissociative Disorders – conscious awareness becomes separated (dissociated) from previous memories, thoughts, and feelings 1) PSYCHOGENIC AMNESIA 2) PSYCHOGENIC FUGUE 3) DISSOCIATIVE IDENTITY DISORDER (Multiple Personality Disorder) 4) DEPERSONALIZATION DISORDER Dissociative Disorders 1) Psychogenic Amnesia – Sudden inability to recall important information--NOT as a result of physical “blow” or drug-related. 2) Psychogenic Fugue DUE TO EXTREME STRESS!! – Loss of memory--flees to a new location and establishes new lifestyle – After recovery, events during fugue are not remembered Dissociative Disorders 3) Dissociative Identity Disorder – rare dissociative disorder in which a person exhibits two or more distinct and alternating personalities – formerly called multiple personality disorder *often history of child or sex abuse In 2008, Herschal Walker, the 1982 Heisman Trophy winner from the University of Georgia, released his book “Breaking Free” which related his experiences with DID. He reported not being able to remember winning the Heisman in 1982 or darker events, such as threatening his then-wife. Dissociative Identity Disorder • Dissociative identity disorder (DID) –Multiple personality disorder Understanding Dissociative Identity Disorder • • • • • Genuine disorder or not? DID rates Therapist’s creation Differences are too great DID and other disorders 4) Depersonalization Disorder – Persistent, recurring feelings that one is not real or is detached from one’s own experience or body. Symptoms: *distorted perception of the body *might feel like he or she is a robot or in a dream *some might fear they are going crazy and might become depressed, anxious, or panicky. For some people, the symptoms are mild and last for just a short time. For others, symptoms can be chronic (ongoing) and last or recur for many years, leading to problems with daily functioning or even to disability. People with Dissociative Disorders may experience any of the following: depression, eating disorders mood swings, headaches, suicidal tendencies, amnesias, sleep disorders (insomnia, night terrors, and sleep walking), time loss, panic attacks and phobias (flashbacks, reactions to stimuli or "triggers"), alcohol and drug abuse, compulsions and rituals, psychotic-like symptoms (including auditory and visual hallucinations), trances, and "out of body experiences." self-persecution, self-sabotage violence (both self-inflicted and outwardly directed). Recent research suggests the risk of suicide attempts among people Disorder (PTSD), widely with trauma There is accepted as a major mental disorders may evidence that illness affecting 8% of the be even higher people with general population in the than among trauma disorders United States, is closely people who have higher rates related to Dissociative have major of alcoholism, Disorders. In fact, 80-100% depression. chronic medical of people diagnosed with a illnesses, and Dissociative Disorder also abusiveness in have a secondary succeeding diagnosis of PTSD generations. Dissociative Disorders are now understood to be fairly common effects of severe trauma in early childhood, most typically extreme, repeated physical, sexual, and/or emotional abuse. Posttraumatic Stress EXAMPLES of Dissociative Disorders: Herschel Walker: DID (Univ. Georgia, Heisman Trophy, Dallas Cowboys) TREATMENTS: *Medical model: therapy to recall the memories, hypnosis or a medication called Pentothal (thiopental) can sometimes help to restore the memories *Psychoanalysis: help an individual deal with the trauma associated with the recalled memories. Fugue--Hypnosis. Dissociative identity disorder-- long-term psychotherapy that helps the person merge his/her multiple personalities into one. *Learning Theories: *Behaviorists: *Cognitive Therapies: irrational interpretations (Depersonalization Dis) *Humanistic: client-centered therapies, responsibility, activelistening. SHOW: Psych in Film, Ver 2, #27, Bourne Identity and #30, Raising Cain Oprah “Dissociative Disorders” SCHIZOPHRENIC DISORDERS (also called Psychotic Disorders) Schizophrenia (Psychotic Disorders) Symptoms of Schizophrenia • Schizophrenia (split mind) = a group of severe disorders characterized by disorganized and delusional thinking, disturbed perceptions, and inappropriate emotions and actions. –Not multiple personalities Schizophrenia literally means “split mind,” meaning a split from reality that shows itself in disorganized thinking, disturbed perceptions and inappropriate emotions and actions. 1874, Medicene, Leipzig & Wurtzburg, Germany The term coined by Emil Kraepelin, who established the diagnostic category “dementia praecox” and Eugen Bleuler, who introduced the term “schizophrenia.” (1857-1939) Medicene, University of Bern PSYCHOTIC: split from reality Schizophrenia • It is a chronic, severe, and disabling brain disorder that has affected people throughout history. About 1 percent of Americans have this illness. • The symptoms of schizophrenia fall into three broad categories: Positive symptoms (psychotic behaviors, thoughts and movements). Negative symptoms (disruptions to normal emotions and behaviors). Cognitive symptoms (poor decision making and concentration, problems with working memory). Symptoms of Schizophrenia Disorganized Thinking • Disorganized thinking – Delusions = false beliefs, often of persecution or grandeur, that may accompany psychotic disorders. – Delusions of Persecution (paranoid) – Delusions of Grandeur – Delusions of Control – Delusions of Reference – A neutral environmental event is believed to have a special and personal meaning. Disorganized Thinking and Speech *Word Salad- random words and phrases *Neologisms- a newly coined word/expression *Echolalia (also known as echologia or echophrasia) is the automatic repetition of vocalizations made by another person Breakdown in selective attention Symptoms of Schizophrenia Disturbed Perceptions • Disturbed perceptions – Hallucinations 6 types • Auditory, Visual, • Tactile, Olfactory, • Gustatory and • Proprioceptive-This was covered under the category of sleep paralysis. These sensations of floating, flying, out-of-body experiences and other dissociative movement events are most likely when in bed before and after sleeping. Symptoms of Schizophrenia Inappropriate Emotions and Actions • Inappropriate Emotions –Flat affect • Inappropriate Actions –Catatonia –Disruptive social behavior Possible symptoms of psychotic illnesses include: *Disorganized or incoherent speech *Confused thinking *Strange, possibly dangerous behavior *Slowed or unusual movements *Loss of interest in personal hygiene *Loss of interest in activities *Problems at school or work and with relationships *Cold, detached manner with the inability to express emotion *Mood swings or other mood symptoms, such as depression or mania CAUSES: •chemical imbalances (“mad as a hatter”) •excess D4 dopamine receptors (in autopsies) (drugs that block dopamine receptors lessen the symptoms) •now researching neurotransmitter glutamate (direct neurons to pass along an impulse) •abnormal brain activity: low in frontal lobes •research shows (during hallucinations) increased activity in thalamus, amygdala, and cortex •greater than normal cerebral cortex tissue loss between ages 13 and 18. •genetics: enlarged, fluid-filled cranial cavities A common finding in the brains of people with schizophrenia is larger than normal lateral ventricles. DIANTHESIS-STRESS HYPOTHESIS: The idea that biological factors may place the individual at risk for schizophrenia (or others), but environmental stressors transform this potential into an actual disorder. Types of Schizophrenia These classicifcations are not in DSM V. 1) DISORGANIZED SCHIZOPHRENIC • confused and incoherent, • jumbled speech • emotionless or flat or inappropriate, even silly or childlike. (flat affect or lack of affect) • disorganized behavior that may disrupt their ability to perform normal daily activities (showering or preparing meals) • hallucinations and delusions Disorganized speech is of two types: NEOLOGISMS: “new words” “I had belly bad luck and brutal and outrageous.” (I have stomach problems and don’t feel good) “I gave all the work money. (I paid tokens for my meal) I was raised in packs (with other people) and since I was in littlehood (little girl) she blamed a few people with minor words (she scolded people). WORD SALAD: “disorganization” The lion will have to change from dogs into cats until I can meet my father and mother and we depart some rats. I live on the front part of Whitton’s head. You have to work hard if you don’t get into bed. She did. She said, “Hallelujah, happy landings.” It’s all over for a squab true tray and there ain’t not squabs, there ain’t no men, there ain’t no music, there ain’t no nothing besides my mother and my father who stand alone upon the Island of Capri where there is no ice, there ain’t no nothing but changers, changers, changers……. 2) CATATONIC SCHIZOPHRENIC •Physical symptoms • immobile and unresponsive to the world around them • very rigid and stiff, unwilling to move • waxy flexibility • occasional grimacing or bizarre postures. • might repeat a word or phrase just spoken by another person. • increased risk of malnutrition, exhaustion, or self-inflicted injury. Catatonic excitement: patients become agitated and hyperactive. 3) PARANOID SCHIZOPHRENIC • preoccupied with false beliefs (delusions) about being persecuted or being punished by someone • thinking, speech and emotions, however, remain fairly normal. •the paranoid delusions of persecution or grandiosity (highly-exaggerated self-importance) are less well organized--more illogical--than those of the patient with purely delusional disorder. •delusions are usually auditory 4) UNDIFFERENTIATED SCHIZOPHRENIC * diagnosed when the person's symptoms do not clearly represent one of the other three subtypes. 5) RESIDUAL SCHIZOPHRENIC * suffered from schizophrenia in the past but no hallucinations or delusions • mildly disturbed thinking • emotionally impoverished **6) PARANOID DELUSIONAL DISORDER • characterized by non-bizarre delusions in the absence of other mood or psychotic symptoms •delusions involving real-life situations that could be true, such as being followed, being conspired against or having a disease • delusions persist for at least one month. • non-bizarre refers to situations such as: being followed, being loved, having an infection, or being deceived by one’s spouse • needs to be evaluated with respect to religious and cultural differences. Onset and Development • • • • • Statistics on schizophrenia Onset of the disease Positive versus negative symptoms Chronic (process) schizophrenia Acute (reactive) schizophrenia Understanding Schizophrenia Brain Abnormalities • Dopamine Overactivity –Dopamine – D4 dopamine receptor –Dopamine blocking drugs • Glutamate Understanding Schizophrenia Brain Abnormalities • Abnormal Brain Activity and Anatomy –Frontal lobe and core brain activity –Fluid filled areas of the brain Understanding Schizophrenia Brain Abnormalities • Maternal Virus During Pregnancy –Studies on maternal activity and schizophrenia –Influence of the flu during pregnancy Understanding Schizophrenia Genetic Factors • Genetic predisposition • Twin studies • Genetics and environmental influences The GENAIN QUADRUPLETS (b.1930) were monozygous woman all suffered from schizophrenia, demonstrating a large genetic component to the disease. The girls (Nora, Iris, Myra, Hester) were fictitiously named for NIMH (National Institute of Mental Health). Both parents had mental disorders during their lifetime. Identical Twin studies show: *48% probability of having schizophrenia if your twin does. *single placenta: 6 in 10 chance *separate placentas: 1 in 10 chance *one study showed the older the father, the greater risk of schizophrenia in offspring Understanding Schizophrenia Psychological Factors • Possible warning signs – – – – – – – – Mother severely schizophrenic Birth complications (low weight/oxygen deprivation) Separation from parents Short attention span Poor muscle coordination Disruptive or withdrawn behavior Emotional unpredictability Poor peer relations and solo play TREATMENTS: *Medical model: Start: olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal), or aripiprazole (Abilify)….Then: chlorpromazine, fluphenazine, and haloperidol (Haldol)…. Last resort: Clozapine (Clozaril) (has side effects) *Psychoanalysis: medication, psychological counseling and social support. *Learning Theories: *Behaviorists: medication, psychological counseling and social support. *Cognitive Therapies: *Humanistic: medication, psychological counseling and social support. Tardive dyskinesia is a difficult-to-treat form of dyskinesia, a disorder resulting in involuntary, repetitive body movements. In this form of dyskinesia, the involuntary movements are tardive, meaning they have a slow or belated onset. This neurological disorder frequently appears after long-term or high-dose use of antipsychotic drugs, or in children and infants as a side effect from usage of drugs for gastrointestinal disorders EXAMPLES of Schizophrenia : John Nash: Nobel Prize Winning Mathematician Mary Todd Lincoln: former First Lady of U. S. Alan Alda’s mother: Actor Show MOVIE: Broken Minds And THE WORLD OF AbNORMAL PSYCHOLOGY #9 The Schizophrenias PBS The New Asylums http://www.janssen.com/janssen/mindstorm_video.html Personality Disorders Personality Disorders • Personality disorders = psychological disorders characterized by inflexible and enduring behavior patterns that impair social functioning –Anxiety cluster –Eccentric cluster –Dramatic/impulsive cluster 1) Paranoid Personality Disorder (PPD) 2) Obsessive-Compulsive Personality Disorder(OCPD) 3) Antisocial Personality Disorder 4) Borderline Personality Disorder 5) Schizoid Personality Disorder 6) Schizotypal Personality Disorder 7) Narcissistic Personality Disorder Personality Disorders Personality Disorders *disorders characterized by inflexible and enduring behavior patterns that impair social functioning *usually without anxiety, depression, or delusions **In contrast to other psychological problems, PDs do NOT want to change. They believe the problem lies with the “other” person. 15% of the American population are affected with personality disorders (Mayo Clinic)….46.5 million people About one in seven U.S. adults has at least one personality disorder, and many have more than one. Obsessive-compulsive PD Paranoid PD Antisocial PD 3.6% Schizoid PD Schizotypal PD Avoidant PD Borderline PD Histrionic personality disorder Narcissistic PD Dependent PD 8% 4.4% 3.1% 3% 2.4% 2% 1.8% >1% >1% Personality Disorder Types 1) Paranoid Personality Disorder * Belief that others are lying, cheating, exploiting or trying to harm you * Perception of hidden, malicious meaning in benign comments * Inability to work collaboratively with others * Emotional detachment * Hostility toward others CAUSES: *Might be learned…. might be traced back to childhood experiences. *Studies of identical and fraternal twins suggest that genetic factors may also play an important role in causing the disorder. Twin studies indicate that genes contribute to the development of childhood personality disorders. Personality Disorder Types 2) Obsessive-Compulsive Personality Disorder * Excessive concern with order, rules, schedules and lists * Perfectionism, often so pronounced that you can't complete tasks because your standards are impossible to meet Example: * Inability to throw out even broken, worthless objects Howard * Inability to share responsibility with others Hughes * Inflexibility about the "right" ethics, ideas and methods * Compulsive devotion to work at the expense of recreation and relationships * Financial stinginess * Discomfort with emotions and aspects of personal relationships that you can't control ***interferes with daily life A physician in this instance is best sticking with the facts of the presenting problem and underlying disorder rather than offering vague impressions of their opinion. Since the individual with this disorder tends to be meticulous and concerned with details, the treatment regimen -- once accepted -- will likely be adhered to rigorously, without incident. Treatment: Personality Disorder Types 3) Antisocial Personality Disorder • • • • • • • • • • Chronic irresponsibility and unreliability Lack of regard for the law and for others' right Persistent lying and stealing Aggressive, often violent behavior Lack of remorse for hurting others Lack of concern for the safety of yourself and others Intelligent, charming Treatment--Because many people who suffer social skills from this disorder will be mandated to therapy 75% men in a forensic or jail setting, motivation on the Potentially dangerous patient's part may be difficult to find. Therapy Example: Hannibal Lecter in Silence of the Lambs should focus on alternative life issues, such as goals for when they are released from custody, improvement in social or family relationships, learning new coping skills, etc. ….. part of the therapy should be devoted to discussing the antisocial behavior and feelings (or lack thereof). Antisocial Personality Disorder • Antisocial personality disorder = a personality disorder in which the person (usually a man) exhibits a lack of conscience for wrongdoing, even toward friends and family members. May be aggressive and ruthless or a clever con artist. –Sociopath or psychopath • Understanding antisocial personality disorder **Although carriers of this personality disorder are frequently found among street criminals and con artists, they are also well represented among successful politicians and business people who put career, money, and power above everything and everyone. **Two to three percent of the population in the U.S. may have antisocial personality disorder. **Chronic lying, stealing, and fighting are common signs. **Violations of social norms begin early in life-disrupting class, getting into fights, and running away from home. Personality Disorder Types 4) Borderline Personality Disorder * Difficulty controlling emotions or impulses * Frequent, dramatic changes in mood, opinions and plans * Stormy relationships involving frequent, intense anger and possibly physical fights * Fear of being alone despite a tendency to push people away * Feeling of emptiness inside *75% female Treatment: Dialectical Behavior Therapy: teaches the client how to learn to better take control of their lives, their emotions, and themselves through selfknowledge, emotion regulation, and cognitive restructuring. 5) Schizoid Personality Disorder *Lack of interest in social relations *Inability to express feelings • Lack of regard for others' opinions • Extreme introversion • Emotional distance, even from family members • Fixation on your own thoughts and feelings 6) Schizotypal Personality Disorder *Egocentricity, avoidance of others, eccentricity of thought *Oversensitive & frequently see chance events as related to themselves. *Individuals with this disorder usually distort reality more so than someone with Schizoid Personality Disorder. *Indifference to and withdrawal from others * "Magical thinking" — the idea that you can influence people and events with your thoughts * Odd, elaborate style of dressing, speaking and interacting with others * Talking to yourself * Belief that messages are hidden for you in public speeches and displays * Suspicious or paranoid ideas Personality Disorder Types 7) Narcissistic Personality Disorder *Preoccupied with receiving attention & nurturance *Exaggerated sense of self-importance Treatment: Hospitalization of patients with severe Narcissistic Personality occurs frequently, such as those who are quite impulsive or self-destructive, or who have poor reality-testing. Charlie Manson is the most famous NPD. In 1968, he was found guilty of being responsible for the famous Tate-LaBianca murders which he had concocted to start a black-white race war in the U.S. He persuaded his “followers” to brutally kill actress Sharon Tate who was 8 months pregnant with child. Three days later his followers killed Mr. & Mrs. LaBianca in a similar fashion. (see video following) Another famous NPD is Diane Downs who was convicted of attempting to kill her 3 children so she could continue her affair with a man who didn’t want children. She claimed she stopped her car for a man in distress and he came up to the vehicle and shot her children. One daughter died, her son was paralyzed from the waist down, and the third daughter (8 at the time) was in such shock that she refused to speak. Eventually, the third daughter testified against her mother and was adopted by the district attorney who prosecuted the case. (see video following) MOVIE: Small Sacrifices (1989) Personality Disorders • PET scans illustrate reduced activation in a murderer’s frontal cortex Normal Murderer Personality Disorders 35 30 Percentage of criminal offenders 25 20 15 10 5 0 Total crime Childhood poverty Thievery Obstetrical complications Violence Both poverty and obstetrical complications EXAMPLES of Personality Disorders : Adolph Hitler: Anti-Social PD & Narcissistic PD There is some speculation that Diana, Princess of Wales and Marilyn Monroe both suffered from Borderline PD. TREATMENTS: *Medical model: There's no cure for these conditions, but therapy and medication can help. The symptoms of some personality disorders also may improve with age. *Psychoanalysis: SchizoidPD--individual therapy (brief), SchizotypalPD-the clinician must exercise care to not directly challenge delusional or inappropriate thoughts…warm, supportive, and client-centered environment should be established with initial rapport. *Learning Theories: *Behaviorists: *Cognitive Therapies: BorderlinePD--Dialectical Behavior Therapy: teaches the client how to learn to better take control of their lives, their emotions, and themselves through self-knowledge, emotion regulation, and cognitive restructuring. *Humanistic: Group setting (BPD), client-centered therapies (OCPD), responsibility, active-listening, NarcissisticPD--Small staff-patient groups-feelings are shared and patients' comments taken seriously by staff, constructive work assignments, recreational activities, and opportunities to sublimate painfully conflictual impulses. Show THE MIND #35 The Mind of The Psychopath and THE WORLD OF AbNORMAL PSYCHOLOGY: #5 Personality Disorders Gacy or Bundy BIOPSYCHOSOCIAL DISORDERS 1) 2) 3) 4) 5) CORONARY HEART DISEASE MIGRAINE HEADACHES BREAST CANCER ANOREXIA NERVOSA BULIMIA NERVOSA Biopsychosocial Disorders 1) Coronary Heart Disease (Ch 14, p. 539541) *Lethal blockage of arteries that supply blood to heart muscle *Causes: age, gender, family history, blood pressure, chloresterol, weight, lifestyle, psychological state (type A personality) Biopsychosocial Disorders 2) Migraine Headaches (not in book) *Intensely painful, recurring headache--reduced flow of bloodto certain parts of brain-overarousal of sympathetic nervous system *Causes: stress, change in weather, hormonal changes, neurotransmitter: glutimate *Family history ***Seeing zigzag lines or flashing lights, tingling, numbness in arms & legs. Biopsychosocial Disorders 3) Breast Cancer (Ch 14, p.543-544) *Over 50, no children, family history *Stressful life leads to higher level of the disease Swedish researchers say that being under stress may double a woman's risk of developing breast cancer.They based their findings on surveys of more than 1,400 Swedish women in the late 1960s who were part of a long-term health-care study. They found that women who reported being under stress had twice the risk of developing breast cancer as women who managed to stay cool, calm, and collected. Biopsychosocial Disorders 4) Anorexia Nervosa (Ch 12, p.454-467) *Eating disorder, intense abhorrence of obesity, insistance that one is fat *Loss of 25%+ original body fat *Refusal to maintain normal weight 5) Bulimia Nervosa (Ch 12, p. 464-467) *Unable to stop eating voluntarily *Preoccupation with weight gain *Attempt to lose weight thru binge eating, selfinduced vomiting & overuse of laxatives and diuretics A surplus of serotonin is associated with anorexia EXAMPLES of Biopsychsocial Disorders : Karen Carpenter: Victoria Beckham: Died of anorexia age32 (weighed 80lbs) Alanis Morisette: Jane Fonda: Actress TREATMENTS: *Medical model: Preventative (diet & exercise) *Psychoanalysis: Hypnosis *Learning Theories: guided learning *Behaviorists: *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. 1) 2) 3) 4) 5) INJURY ALZHEIMERS DISEASE WERNICKE - KORSAKOFF’S SYNDROME PARKINSON’S SYNDROME PARKINSON’s DISEASE Neurophysical Disorders 1) Injury (not in book) *Brain trauma 2) Alzheimers (Ch 4, p 177-178) **trouble remembering recent events, activities, or the names of familiar people or things **Age (number of people w/disease doubles every 5 years past age 65 ) **family history (usually occurs between age 30-60 if it’s genetic). . . . One risk factor for this type of AD is a protein called apolipoprotein E (apoE). **Deficiency of acetylcholine Neurophysical Disorders 3) Wernicke’s-Korsakoff’s Syndrome (not in book) *memory disorder caused by a lack of vitamin B1 (thiamine). *affects short-term memory. *Most common cause: alcoholism *A related disorder, Wernicke's syndrome, often occurs before Korsakoff's syndrome. Because they often occur together, the range of symptoms caused by the two diseases is often called Wernicke's-Korsakoff syndrome. The main symptoms of Wernicke's syndrome occur acutely. They include: • Difficulty with walking and balance • Confusion • Drowsiness • Paralysis of some eye muscles Neurophysical Disorders 3) Korsakoff’s Syndrome *Thiamine is necessary for memory and other brain functions. People who drink a lot of alcohol often replace food with alcohol. As a result, they take in fewer vitamins, leading to vitamin deficiencies. In addition, alcohol increases the body's need for B vitamins while interfering with its ability to absorb, store, and use thiamine. *A genetic abnormality may make some people more susceptible to Korsakoff's syndrome when they drink large amounts of alcohol and consume diets low in vitamins. Neurophysical Disorders 4) Parkinson’s Syndrome (not in book) *tremor in hand, foot, mouth, or chin *stiffness or rigidity of the limbs and trunk *bradykinesia (slowness of movement) *postural instability, or impaired balance and coordination *Occurs in about 1% of people over 65, 15% in ages 74-85, and over 50% of people over 85 Neurophysical Disorders • Parkinson’s Disease (not in book) caused by the progressive impairment or deterioration of neurons (nerve cells) in an area of the brain known as the substantia nigra. When functioning normally, these neurons produce a vital brain chemical known as dopamine. Dopamine serves as a chemical messenger allowing communication between the substantia nigra and another area of the brain called the corpus striatum. This communication coordinates smooth and balanced muscle movement. A lack of dopamine results in abnormal nerve functioning, causing a loss in the ability to control body movements. Neurophysical Disorders • Parkinson’s Disease – Why Parkinson’s occurs and how the neurons become impaired is not known. However, increasing evidence suggests that it may be inherited. TREATMENTS: *Medical model: Aricept (alzheimer’s—cholinesterase inhibitors), L-dopa (parkinson’s) *Psychoanalysis: *Learning Theories: *Behaviorists: *Cognitive Therapies: discuss irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. L-dopa (OTC) **naturally-occurring dietary supplement and psychoactive drug commonly found in some foods and herbs. **precursor to the neurotransmitter dopamine, norepinephrine (noradrenaline), and epinephrine (adrenaline). **crosses the blood-brain barrier whereas dopamine cannot. Once into the CNS, it is converted into dopamine. Cholinesterase inhibitors (Aricept, Exelon) **Alzheimer’s causes brain cells die and connections among cells are lost, causing cognitive symptoms to worsen. **cannot stop the damage, however, they may help lessen or stabilize symptoms **prevents the breakdown of acetylcholine EXAMPLES of Biopsychsocial Disorders : Mao Zedong: Mohammed Ali: Chinese leader Prize Fighter /boxer Michael J. Fox: Actor Janet Reno: former U.S. Attorney Geneeral Show THE WORLD OF AbNORMAL PSYCHOLOGY #10 Organic Brain Disorders SUBSTANCE ABUSE DISORDERS 1) 2) 3) 4) 5) ALCOHOL COCAINE METHALAMPHETAMINES NICOTINE ECSTASY Substance Abuse Disorders 1) Alcohol (Ch 7, p.294-304) *Drinking impairs life adjustments *Health, personal relationships, occupational functioning *Strong relationship between alcohol & violence. Am I drinking too much? YES, if you are: ・A woman who has more than seven drinks* per week or more than three drinks per occasion ・A man who has more than 14 drinks* per week or more than four drinks per occasion ・Older than 65 years and having more than seven drinks* per week or more than three drinks per occasion *--One drink = one 12-oz bottle of beer (4.5 percent alcohol) or one 5-oz glass of wine (12.9 percent alcohol) or 1.5 oz of 80proof distilled spirits. Substance Abuse Disorders 2) Cocaine (Ch 7, p.294-304) *Chronic abuse can promote acute psychotic symptoms & hallucinations *Activates the part of the brain as areas of pleasure & rewards (food, sex, water) *Long term effects include: Addiction Irritability and mood disturbances Restlessness Paranoia Auditory hallucinations Substance Abuse Disorders 3) Methamphetamines *synthetic amphetamines or stimulants that are produced and sold illegally in pill form, capsules, powder and chunks. *has a structure similar to dopamine (the brain's pleasure transmitter) and causes neurons to release large amounts of dopamine to produce a high. ……… leads to permanent brain damage as natural dopamine production sites are destroyed - forcing the user to become even more reliant on meth for pleasure. *known as meth, crank, glass, speed, crystal, ice, batu, chalk, shabu, or zip Substance Abuse Disorders 4) Nicotine (Ch 7, p.294-304) *Poisonous substance in cigarettes *450,000 related deaths per year. **Used as a coping device *About 80 percent of nicotine is broken down to cotinine by enzymes in your liver. *Nicotine is also metabolized in your lungs to cotinine and nicotine oxide. *Cotinine and other metabolites are excreted in your urine. Cotinine has a 24-hour half-life, so you can test whether or not someone has been smoking in the past day or two by screening his or her urine for cotinine. Substance Abuse Disorders 4) Nicotine (Ch 7, p.294-304) A synapse is the site where two neurons come into contact. The presynaptic neuron releases a neurotransmitter, which binds to receptors on the postsynaptic cell. This allows signals to be transmitted from neuron to neuron in the brain. Substance Abuse Disorders 4) Nicotine (Ch 7, p.294-304) Nicotine works by docking to a subset of receptors that bind the neurotransmitter acetylcholine. Acetylcholine is the neurotransmitter that (depending on what region of the brain a neuron is in): * Delivers signals from your brain to your muscles * Controls basic functions like your energy level, the beating of your heart and how you breathe * Acts as a "traffic cop" overseeing the flow of information in your brain * Plays a role in learning and memory Substance Abuse Disorders 5) MDMA (ECSTACY) *methylenedioxymethamphetamine *amphetamine family of compounds with stimulant and psychodelic properties. *Short-term effects include feelings of mental stimulation, emotional warmth, enhanced sensory perception, and increased physical energy. *Adverse health effects can include nausea, chills, sweating, teeth clenching, muscle cramping, and blurred vision. Substance Abuse Disorders 5) MDMA (ECSTACY) (cont) *ecstasy contains a number of other drugs, including methamphetamine, caffeine, dextromethorphan, ephedrine, and cocaine. *has potent effects on the cardiovascular system and on the body's ability to regulate its internal temperature……increases the risk of heart damage **increases the activity levels of at least three neurotransmitters: serotonin, dopamine, and norepinepherine. Substance Abuse Disorders 5) MDMA (ECSTACY) (cont) **Compared to methamphetamine, MDMA triggers a larger increase in serotonin and a smaller increase in dopamine. Serotonin is a major neurotransmitter involved in regulating mood, sleep, pain, emotion, and appetite, as well as other behaviors. By releasing large amounts of serotonin, and also interfering with its synthesis, MDMA leads to a significant depletion of this important neurotransmitter. As a result, it takes the human brain a significant amount of time to rebuild the store of serotonin needed to perform important physiological and psychological functions. TREATMENTS: *Medical model: methadone relieves pain. *Psychoanalysis: *Learning Theories: Twelve-Step Programs *Behaviorists: *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. MOUSE PARTY: A Mouse on Drugs http://learn.genetics.utah.edu/content/addiction/drugs/mo use.html Show THE WORLD OF AbNORMAL PSYCHOLOGY: #6 Substance Abuse Disorders The Meth Epidemic Psych in Film, Ver 2, #25, Lost Weekend (alcoholism) SEXUAL DISORDERS 1) GENDER IDENTITY DISORDER (TRANSSEXUALISM) 2) SEXUAL DISFUNCTION 3) PARAPHILIAS Sexual Disorders (Ch 12, p.467-482) 1) Gender Identity Disorder (Transsexualism) *Confusion or uncertainty between biological sex and gender identity. 2) Sexual Disfunction *Inhibitions in sexual response Sexual Disorders 3) Paraphilias – Fetishism, zoophilia, pedophila, exhibitionism, voyeurism, masochism, sadism et. al. – Sexual response to unusual objects or situations TREATMENTS: *Medical model: viagra *Psychoanalysis: *Learning Theories: classical conditioning. *Behaviorists: *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. Show THE WORLD OF AbNORMAL PSYCHOLOGY: #7 Sexual Disorders DEVELOPMENTAL (CHILDHOOD) DISORDERS 1) ATTENTION DEFICIT HYPERACTIVITY DISORDER (ADHD) 2) CONDUCT DISORDER 3) SEPARATION ANXIETY DISORDER 4) AUTISM 5) DYSLEXIA 1) Attention Deficit Hyperactivity Disorder (ADHD) (not in book) *Maladaptive behavior that interferes with effective task-oriented behavior *Impulsive, excessive motor activity, exaggerated muscular activity, difficulty maintaining attention *controversial diagnosis *Critics claim ADHD is overdiagnosed (i.e.)blame children for unskilled parents or teachers. *drug treatment includes stimulants *stimulant drug therapy combined with behavioral therapy can improve attention and diminished hyperactivity in 70% of ADHD children. *Strattera -- a drug used for ADHD is a norepinephrine reuptake inhibitor One of the theories as to why Ritalin (stimulants) helps people with ADHD is that they may have more dopamine transporters than others. The excess of transporters removes dopamine from the synapse before it can reach a dopamine reward receptor in the receiving neuron, so the attention circuitry in the ADHD brain is under stimulated. By blocking transporters, Ritalin allows more dopamine to reach receptors, thus increasing attention signaling, which helps people with ADHD to focus. Ritalin, when taken orally, slowly raises dopamine levels over the course of an hour or so. 2) Conduct Disorders (not in book) *Persistant, repetitive violation of rules and disregard for rights of others *Fighting, defiance, disobedience, destruction of property, attention seeking, inattentiveness, overaggressive behavior, bullying, physical aggression, cruel behavior toward people and pets, destructive behavior, lying, truancy, vandalism, and stealing. *ODD--Oppositional Defiant Disorder: disobedient, hostile behavior towards authority figures *clinically significant impairment in social, academic, or occupational functioning. 3) Separation Anxiety Disorder (not in book) *Excessive anxiety about separation from people to whom the child is attached *Unrealistic fears, oversensitivity, selfconsciousness, nightmares, chronic anxiety 4) Autism (p. 147-148, 424, 668) *Pervasive developmental disorder occurring in infancy or childhood—1 in 88 children (as of 2008 *Qualitative impairment in reciprocal social interaction & communication--restricted repertoire of activities & interests Example: Sally and Ann are playing together, when Sally puts a piece of candy in a box and leaves the room. While Sally is gone, Anne opens the box, removes the candy and stashes it in her purse. When Sally comes back, where will she look for the candy? Normal children will say that Sally will look in the box. Autistic children are most likely to say (if they communicate at all) that Sally will look in the purse. The autistic child lacks “theory of mind”. Severely autistic children cannot imagine themselves in Sally’s place. 5) Dyslexia *reading difficulties *affects 1 of 5 children *involves the abnormalities in the brain’s language-processing circuits. Another cause may be language itself: *English: bizarre spelling menagerie, containing 1120 ways to spell only 40 different sounds, are more likely to be dyslexic than *Italian: 33 combinations of letters for 25 sounds. TREATMENTS: *Medical model: Stimulants (ADHD), Ritlan, Strattera *Psychoanalysis: *Learning Theories: Token Economy *Behaviorists: *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. Show THE WORLD OF AbNORMAL PSYCHOLOGY: #11 Behavior Disorders of Childhood Psych in Film, Ver 2, #26, Mercury Rising (autism), #15, Parenthood (special needs child) ADJUSTMENT DISORDERS ADJUSTMENT DISORDERS: Other conditions that may be a focus of clinical attention. *mild depression *physical complaints *marital problems *academic problems *job problems *parent-child problems *bereavement *malingering (faking an illness) TREATMENTS: *Medical model: *Psychoanalysis: *Learning Theories: *Behaviorists: *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. TREATMENTS: *Medical model: *Psychoanalysis: *Learning Theories: *Behaviorists: *Cognitive Therapies: irrational interpretations *Humanistic: client-centered therapies, responsibility, active-listening. Rates of Disorder Rates of Disorder • Mental health statistics • Influence of poverty • Other factors (2008 data, NIMH) Rates of Psychological Disorders Percentage of Americans Who Have Ever Experienced Psychological Disorders Ethnicity Gender Disorder White Black Hispanic Men Women Totals Alcohol abuse or dependence 13.6% 13.8% 16.7% 23.8% 4.6% 13.8% Generalized anxiety 3.4 6.1 3.7 2.4 5.0 3.8 Phobia 9.7 23.4 12.2 10.4 17.7 14.3 Obsessive-compulsive disorder 2.6 2.3 1.8 2.0 3.0 2.6 Mood disorder 8.0 6.3 7.8 5.2 10.2 7.8 Schizophrenic disorder 1.4 2.1 0.8 1.2 1.7 1.5 Antisocial personality disorder 2.6 2.3 3.4 4.5 0.8 2.6 Questions for Review 1) RECALL In Rosenhan’s study, who discovered that the “pseudopatients” were feigning mental illness? a) psychiatrists b) psychologists c) Nurses and aides working on the ward d) Other patients e) Other physicians 2) APPLICATION Which of the following symptoms most clearly suggests the presence of abnormality? a) hallucinations b) worries c) Unusual behavior d) creativity e) distraction 3) RECALL Hippocrates proposed that mental disorder was caused by a) Possession by demons b) An imbalance in four bodily fluids c) A fungus growing on rye grain d) Traumatic memories in the unconscious e) The taking of potions. 4) RECALL The behavioral perspective emphasizes the influence of __, while the cognitive perspective emphasizes __. a) Genetics / conscious processes b) Conscious processes / unconscious processes c) Heredity / environment d) Medical factors / psychological factors e) The environment / mental process 5) UNDERSTANDING THE CORE CONCEPT Which of the following would be least likely to be noticed by a clinician using strictly the medical model of mental disorder? a) delusions b) Severe disturbances in affect c) An unhealthy family environment d) A degenerative brain disease e) hallucinations 6) RECALL The DSM IV is based on the a) Cognitive perspective b) Behavioral perspective c) Eclectic view d) Psychoanalytic view e) medical model 7) RECALL Which disorder involves extreme swings of mood from elation to depression? a) Panic disorder b) Bipolar disorder c) schizophrenia d) Unipolar depression e) PTSD 8) APPLICATION According to the preparedness hypothesis, which one of the following phobias would you expect to be most common? a) Fear of snakes (ophidiophobia) b) Fear of books (bibliophobia) c) Fear of horses (equinophobia) d) Fear of the number 13 (triskaidekaphobia) e) Fear of water (aquaphobia) 9) RECALL Which of the following disorders involves a deficiency in memory? a) phobia b) Antisocial personality c) Dissociative fugue d) obsessive-compulsive diorder e) schizophrenia 10) RECALL Which of the following is a disorder in which the individual displays more than one distinct personality? a) schizophrenia b) Depersonalization disorder c) Bipolar disorder d) phobia e) Dissociative identity disorder 11) RECALL Which of the following is primarily a disorder of young American women? a) Bipolar disorder b) schizophrenia c) Anorexia nervosa d) Antisocial personality disorder e) Dissociative identity disorder 12) RECALL Hallucinations and delusions are symptoms of a) schizophrenia b) Somatoform disorders c) Anxiety disorders d) Depersonalization disorders e) Panic disorders 13) RECALL Which category of disorder is most common? a) schizophrenia b) Dissociative disorder c) Eating disorders d) The adjustment disorders and “other conditions that may be a focus of clinical attention” e) Mood disorders 14) UNDERSTANDING THE CORE CONCEPT The DSM-IV groups most mental disorders by their a) treatments b) causes c) symptoms d) theoretical basis e) cures 15) UNDERSTANDING THE CORE CONCEPT Which unfortunate consequence of diagnosing mental disorders is emphasized chapter? a) The inaccuracy of diagnosis b) Stigmatizing those with mental disorders c) Adding to the already overcrowded conditions in mental hospitals d) That some cultures do not recognize mental disorders e) The importance of the insanity defense. 16) RECALL Which one of the following statements is true? a) Mental disorders have a similar prevalence in all cultures b) In general, biology creates mental disorder, while culture merely shapes the way a person experiences it. c) Culture-specific stressors occur primarily in developing countries d) Cultures around the world seem to distinguish between people with mental disorders and people who are visionaries or prophets. e) Mental disorders are more prevalent in Eastern culture. 17) RECALL Insanity is a) Psychological term b) Psychiatric term, found in DSM-IV under “psychotic disorders.” c) Legal term d) Term that refers either to “neurotic” or “psychotic” symptoms e) A classification for those seeking treatment. 18) RECALL A long-standing pattern of irresponsible behavior that hurts others without causing feelings of guilt or remorse is typical of a) An obsessive-compulsive disorder b) An antisocial personality disorder c) A narcissistic personality disorder d) Paranoid schizophrenia e) Dissociative fugue. 19) APPLICATION A young woman wanders into a hospital, claiming not to know who she is, where she is from, or how she got there. Her symptoms indicate that she might be suffering from a(n) ____ disorder a) anxiety b) affective c) personality d) dissociative e) mood 20) RECALL ____ has been called the “common cold of psychopathology” because it occurs so frequently and because almost everyone has experienced it, at least briefly, at some time. a) Obsessive-compulsive disorder b) Bipolar disorder c) Depression d) Paranoid schizophrenia e) Autism 21) RECALL A person who suffers from ____ cannot eat normally but engages in a ritual of “binging”--periodic binges of overeating--followed by “purging” with induced vomiting or use of laxitives. a) Anorexia nervosa b) Bulimia nervosa c) Inhibition d) Mania e) Depression 22) RECALL The ____ type of schizophrenia is characterized by delusions. a) residual b) catatonic c) paranoid d) undifferentiated e) disorganized 23) RECALL Rosenhan believes that his “pseudopatients” were not recognized as normal because a) The staff members in the mental hospital were incompetent b) The staff members in the mental hospitals were just as disturbed as the patients c) Mental illness is a myth d) Staff members did not expect patients to be normal e) He denied the existance of psychological disorders 24) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism B ____Extreme disorders of thinking, involving persistent false beliefs. 25) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism J developmental disorder marked by _____A disabilities in language and social interaction. 26) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism D A class of disorders including bipolar _____ disorder. 28) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism E A class of disorders including panic _____ disorder. 29) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism I A disorder characterized by an unstable _____ personality given to impulsive behavior for which includes remorse after the fact. 30) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism G A class of disorders including _____ depersonalization disorder. 31) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism F A class of disorders including conversion _____ disorder. 32) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism A False sensory experiences that may _____ suggest a mental disorder. 33) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism C The view that mental disorders are _____ diseases that have objective physical causes and require specific treatments. 34) MATCHING a) b) c) d) e) Hallucinations Delusions Medical model Mood disorders Anxiety disorders f) Somatoform disorders g) Dissociative disorders h) Diathesis-stress hypothesis i) Borderline personality disorder j) Autism H The proposal that genetic factors place the _____ individual at risk while environmental stress factors transform this potential into schizophrenic disorder. Show #21, Zimbardo, Psychopathology