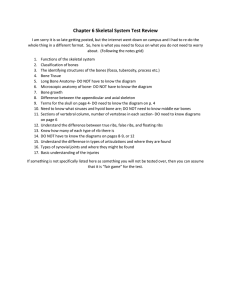
Microanatomy & Physiology Powerpoint in Depth
advertisement

Chapter 7 Skeletal System Subdivision: Micro-anatomy & Physiology 1 Functions of the System: • Protection • Support • Allows for body movement • Produces blood cells • Stores minerals 2 Introduction to the Skeletal System • Components of the Skeletal System= bones, cartilage, ligaments, and tendons • Some definitions: – Cartilage= somewhat rigid, covers the surfaces of bones in/near joints – Tendons= band of strong tissue that connects bones to muscle – Ligaments= band of strong tissue that connects bone to bone – Axial Skeleton=Head to pelvis, main body – Appendicular Skeleton= Everything else Introduction to BONE A. Bones are very active tissues B. Each bone is made up of several types of tissues and so is an organ. C. Bone functions reflect the system 4 Bone Functions (the organ) A. Support and Protection 1. Bones give shape to the head, thorax, and limbs. 2. Bones such as the pelvis and lower limbs provide support for the body. 3. Bones of the skull protect the brain, ears, and eyes. B. Body Movement 1. Bones can act as levers. a. A lever has four components: a rigid bar, a pivot or fulcrum an object that is moved against resistance, and a force that supplies energy. C. Blood Cell Formation 1. Blood cells begin to form through hematopoieses in the yolk sac; they are later manufactured in bone marrow. 2. Two kinds of marrow occupy the medullary cavities of bone. a.Red marrow functions in the formation of red blood cells, white blood cells, and platelets,and is found in the spongy bone of the skull, ribs, sternum, clavicles, vertebrae, and pelvis. b. Yellow marrow, occupying the cavities of most bones, stores fat. D. Storage of Inorganic Salts 1. The inorganic matrix of bone stores inorganic mineral salts in the form of calcium phosphate that is important in many metabolic processes. 2. Calcium in bone is a reservoir for body calcium; when blood levels are low, osteoclasts release calcium from bone. 3. Calcium is stored in bone under the influence of calcitonin when blood levels of calcium are high. 4. Bone also stores magnesium, sodium, potassium, and carbonate ions. 5. Bones can also accumulate harmful elements, such as lead, radium, and strontium. 5 General Bone Structure= Types of Bone Bones differ in size and shape, yet are similar in several ways. – Long = longer than it is wide » Epiphysis= end of a long bone; separated from the main part of the bone from immature cartilage » Diaphysis= shaft of a long bone » Medullary Cavity= hollow space running the length of the diaphysis; has blood, nerves, and marrow » Epiphyseal Line= “Growth Plate”; Where the cartilage is converted to bone as it grows in length Examples: Upper and lower limbs – Short = same length and width » Carpals tarsals – Flat = not wide; flat like a plate » Ribs, sternum, skull, scapulae – Irregular = not distinct shape » Vertebrae, facial 6 More Bone Structure.. Long Bone in depth – Parts 1. Expanded ends of bones that form joints with adjacent bones are called epiphyses. 2. Articular cartilages (hyaline cartilage) cover the epiphyses. 3. The shaft of the bone is the diaphysis. 4. A tough layer of vascular connective tissue, called the periosteum, covers the bone and is continuous with ligaments and tendons. 5. A bone's shape makes possible its function; bony processes or grooves indicate places of attachment for muscles. 6. Compact bone makes up the wall of the diaphysis; the epiphyses are filled with spongy bone to reduce the weight of the skeleton. 7. The diaphysis contains a hollow medullary cavity that is lined with endosteum and filled with marrow. 8 More Bone Structure.. Flat, Short, Irregular Bones • Flat bones – No diaphyses, epiphyses – Sandwich of cancellous (spongy bone tissue) between compact bone tissue • Short and Irregular bone – Compact bone that surrounds cancellous bone tissue center – No diaphyses and not elongated Microscopic Structure of Bone Bone matrix (chemical components): component of bone Organic: collagen and proteoglycans Inorganic: Calcium & Phosphate non-living Bone Tissue: Compact bone tissue: dense/hard Spongy bone tissue: porous ‘like a sponge’ Bone cells= living part of bone Stem cells or osteoprogenitor cells Osteoblasts- make new bone; immature bone cell Osteocyte- mature bone cell; maintains tissue Osteoclasts- breaks down and re-absorbs of old, damaged, or diseased tissue bone 10 Microscopic Structure of Bone • Compact bone tissue – Haversian system—osteons (functional unit of tissue) – Contain living bone cells – Delivery of nutrients & removal of waste • • • • • Lamellae Lacunae Canaliculi Haversian canal Volkmann’s canals 12 Microscopic Structure of Bone Spongy (Cancellous) Bone – Consists of trabeculae (bony plates) – Oriented along lines of stress CopyrightThe McGraw-Hill Companies, Inc. Permission required for reproduction or display. Bone Growth & Development A. Bones form by replacing connective tissues in the fetus. B. Some form within sheetlike layers of connective tissue (intramembranous bones), while others replace masses of cartilage (endochondral bones). Intramembranous Bone Development 1.The flat bones of the skull form as intramembranous bones that develop from layers of connective tissue. 2.Osteoblasts deposit bony tissue around themselves. 3. Once osteoblasts deposit bone are located in lacunae, they are called osteocytes. 4. Cells of the membranous connective tissue that lie outside the developing bone give rise to the periosteum. *Basically it is when matrix gets deposited on the surface of existing bone, this causes a growth in diameter 14 Endochondral Bone Development 1. Most of the bones of the skeleton fall into this category. 2. They first develop as hyaline cartilage models and are then replaced with bone. 3. Cartilage is broken down in the diaphysis and progressively replaced with bone while the periosteum develops on the outside. 4. Cartilage tissue is invaded by blood vessels and osteoblasts that first form spongy bone at the primary ossification center in the diaphysis. 5.Osteoblasts beneath the periosteum lay down compact bone outside the spongy bone. 6.Secondary ossification centers appear later in the epiphyses. 7. A band of hyaline cartilage,the epiphyseal plate,forms between the two ossification centers. 8.Layers of cartilage cells undergoing mitosis make up the epiphyseal plate. 9.Osteoclasts break down the calcified matrix and are replaced with bone building osteoblasts that deposit bone in place of calcified cartilage. 10. Epiphyseal plates are responsible for lengthening bones while increases in thickness are due to intramembranous ossification underneath the periosteum. 11. A medullary cavity forms in the region of the diaphysis due to the activity of osteoclasts. * Basically, occurs in the epiphyseal plates, the cartilage is covered to bone as the cartilage becomes calcified (filled with calcium) causing it to get hard. The growth occurs from the middle outward to increase length (growth in height) 15 16 17 Factors Affecting Bone Growth • Nutrition – Vitamin D • Necessary for absorption of Ca from intestines • Insufficient causes rickets and osteomalacia – Vitamin C • Necessary for collagen synthesis by osteoblasts • Deficiency results in scurvy • Hormones – Growth hormone from anterior pituitary – Thyroid hormone required for growth of all tissues – Sex hormones as estrogen and testosterone18 Homeostasis of Bone ‘Remodeling Bone’ REQUIRES only certain bone cell Review of Types of Bone Cells: Osteoclast Osteoblast Osteocyte Process: Osteoclasts tear down and osteoblasts build bone throughout the lifespan with the processes of resorption and deposition, with an average of 3% to 5% of bone calcium exchanged annually. 19 How does bone repair from injury? Bone Repair Day of Accident 2-3 Days 4 to 6 Weeks After 6 Weeks Weeks to Months Bone Repaired Broken Bone A clot forms in the damaged area Blood Vessels and cells invade the clot and produce which is a callus a fibrous network between the broken bones Osteoblasts enter callus and begin to form spongy bone or cancellous bone Spongy bone is slowly remodeled to form compact bone Bone healed stronger around the surrounding area 20