bYTEBoss Vag Bleed Pelvic Pain 8
advertisement

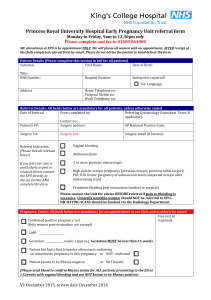
Approach to the First Trimester Patient with Vaginal Bleeding or Pelvic Pain Eric R. Swanson, MD, FACEP Associate Professor, Division of Emergency Medicine Medical Director, AirMed University of Utah Health Sciences Center AirMed Objectives • Provide and evidence based approach to the ED patient with vaginal bleeding and abdominal or pelvic pain • Discuss the diagnostic role of technology (hormonal assays and US) • Provide a guideline algorithm for managing these patients Case Study • HPI: 28 yo female presents to the ED with vaginal bleeding and cramping lower abdominal pain. Onset of pain was gradual & bleeding started as spotting yesterday and became heavy today. LMP 5 weeks ago. • ROS: + Nausea, No fever, chills or urinary symptoms • Exam: BP 128/80 HR 76 RR 16 T 37.5 Abdomen is soft with bilateral lower quadrant and suprapubic tenderness. No CVAT. Pelvic - Os closed, blood is coming from the uterus • What information would be useful to you now? ß-HCG • The nurse informs you that a ß-HCG was not obtained because…. – The pt had her “tubes tied” – The pt was “not sexually active” – The pt was “on her period” ß-HCG • Every female patient of reproductive age with abdominal pain or vaginal bleeding needs to have a pregnancy test. • Pittsburgh study – Unrecognized Pregnancy in ED patients • 6.3% Overall • 13% in women with abd or pelvic complaints • 2.5% with other complaints • What are you worried about in this patient? What are you worried about in this patient? • Ectopic pregnancy • Spontaneous abortion Ectopic Pregnancy • Incidence – Historically 4.5/1000, Current incidence is 20/1000 – Mortality has decreased 90% but still the leading cause of first trimester mortality • Risk Factors – Infertility, history of PID, previous tubal surgeries, previous ectopic and IUD use. Risk factors are present in less than 50% of patients. • Clinical Presentation (Variable) – Abdominal pain - 10% have no pain – Vaginal bleeding - 30% have no bleeding • Exam (25% "normal" pelvic) – Abdominal and adnexal tenderness - 50% – Adnexal mass - 10% – Varying uterine size Spontaneous Abortion • Incidence – 15 -20 % of all known pregnancies • Causes – genetic abnormalities > 50 % • Clinical presentation – Most before 8 or 9 weeks, can occur up to 20 weeks – Spotting proceeding to heavy bleeding with clots or tissue – Pain is usually midline and cramping • Exam – Midline suprapubic tenderness – Os closed – Os open Should a quantitative ß-HCG level influence the decision to perform pelvic ultrasound? • You order a pelvic ultrasound but the radiologist requests a quantitative ß-HCG first. Or… • Radiologist asks if the ultrasound can be done as an outpatient the next day or so Should a quantitative ß-HCG level influence the decision to perform pelvic ultrasound? • Perspective: – Vaginal bleeding, abdominal pain, or both in the first Trimester will result in: • 60% Normal pregnancy • 10% Ectopic • 30% Miscarriage – 50% of ectopic pregnancies that present to an emergency department are not diagnosed at the first visit, yet 70% to 80% are detectable using a combination of transvaginal ultrasound and quantitative ßHCG Discriminatory level of ß-HCG • ß- HCG = 2,000 • Sensitivity 100%, Specificity 98% • PPV 98%, NPV 100% • Radiologist asks why you are getting the US if the ß- HCG is less than 2,000. Literature • Barnhart, Obstet Gynecol 1994: – 59% of ectopics never exceed ß-HCG > 1,500 • Brennan, Acad Emerg Med 1995: – 15% of ectopics will rupture prior to missed menses. – 83% of ectopics will never exceed ß-HCG of 2,000 • (range <100 to > 50,000). – 36% to 50% will have a lower ß-HCG on serial testing Literature • Kaplan, Ann Emerg Med 1996: – Subgroup of patients with ß-HCG < 1,000 had 4X risk of ectopic. – One third of this subgroup were already ruptured. – Initial ED work-up was diagnostic in 79% of patients overall, and 70% of ectopics. • Dart, Ann Emerg Med 1997: – 17% of all patients with ß-HCG < 1,000 have diagnostic US. – 40% of patients with an ectopic and ß-HCG < 1,000 have diagnostic initial US. Clinical Prediction Rule • Buckley, Ann Emerg Med 1999 – Prospective, 915 patients – FHT’s or tissue in os: Never had an ectopic – High Risk: Peritoneal signs, definite CMT • 29% had ectopic – Intermediate Risk: Non-midline pain or tenderness, no FHT’s, no tissue in os. • 7% had ectopic (most patients in this group - 70% of total) – Low Risk: All others • 0.5% (1 of 196 patients) had ectopic (only 20% of total were low risk) • Retrospective, 730 ED pts, Quant ß-HCG & formal US • ß-HCG < 1,500 more than doubled the odds of ectopic • ß-HCG < 1,500 more than 5 times risk of abnormal pregnancy • 158 (22%) had ß-HCG < 1,500, – 25% had ectopic – 16% had normal IUP So……. • High incidence of ectopic in symptomatic first trimester pts in the ED (around 10%) • Exam is generally not helpful – Exceptions are peritoneal signs (ectopic) or presence of tissue (SAB) or FHT’s (Live IUP) • Low ß-HCG doesn’t mean low risk – In fact ß-HCG < 1,500 is 2-4 times risk for ectopic In the Era of ED Ultrasound • Prospective, 1,490 1st trimester ED US – IUP 1,037 (70%) – Demise 127 (8%) – Definite ectopic 24 (2%) – Molar Pregnancy (<1%) – Indeterminate 300 (20%) • 300 Indeterminate Ultrasounds – Demise 158 (53%) – IUP 88 (29%) – Ectopic 44 (15%) American Journal of Emergency Medicine (2007) 25, 591 – 596 Female pt with abdominal pain and/or vaginal bleeding Stable Unstable 2 IV's B-HCG, HCT, Type & Cross FAST Exam Ob/Gyn or Surgery consult B-HCG from triage Clinical Assesment Neg Pos Pelvic exam Os Open Tissue present Excessive bleeding Os Closed Quant BHCG Type & Rh HCT if indicated IV, HCT, Type & Rh consult OB/Gyn Rhogam if indicated ED US indeterminate or No ED US done Quant < 2,000 No IUP Quant > 2,000 Formal US Formal US if anything other than trivial sx's US if risk factors US if clinical suspicion IUP Doppler FHT's or ED US definite IUP No IUP or Ectopic IUP Ectopic D/W Ob/Gyn Rhogam if indicated Repeat Quant in 48 hrs OB/ Gyn Consult Rhogam if Indicated OB/Gyn F/U Rhogam if Indicated Female pt with abdominal pain and/or vaginal bleeding Stable Unstable 2 IV's B-HCG, HCT, Type & Cross FAST Exam Ob/gyn or Surgery consult B-HCG from triage Clinical Assesment Neg Pos Pelvic exam Os Open Tissue present Excessive bleeding IV, HCT, Type & Rh consult OB/Gyn Rhogam if indicated Os Closed? Quant BHCG Type & Rh HCT if indicated ED US indeterminate Doppler FHT's or ED US definite IUP Os Open Tissue present Excessive bleeding Os Closed? Quant BHCG Type & Rh HCT if indicated IV, HCT, Type & Rh consult OB/Gyn Rhogam if indicated ED US indeterminate or No ED US done Quant < 2,000 No IUP Quant > 2,000 Formal US Formal US if anything other than trivial sx's US if risk factors US if clinical suspicion IUP Doppler FHT's or ED US definite IUP No IUP or Ectopic IUP Ectopic D/W Ob/Gyn Rhogam if indicated Repeat Quant in 48 hrs OB/ Gyn Consult Rhogam if Indicated OB/Gyn F/U Rhogam if Indicated Controversy: Does evidence of IUP on ultrasound eliminate the possibility of an ectopic pregnancy? • In general this is true. • General population: The risk of heterotopic pregnancy is 1:30,000 (1948), Now 1:2600 to 1:8000. • Assisted reproduction: The risk is 1:100 to 1:500 – Ultrasound is misleading due to concurrent IUP. – Quantitative ß-HCG is not helpful due to normal fetus making the hormone. – Expectant management is not indicated. Controversy: Does evidence of IUP on ultrasound eliminate the possibility of an ectopic pregnancy? • Point: Use extreme care and involve obstetrics in any pregnant patient with lower abdominal pain or vaginal bleeding and assisted reproduction. Ectopic Pregnancy: Treatment • Unstable – – – – – – Oxygen Volume resuscitation FAST Exam Type specific blood OB/GYN Laparotomy (possibly Laparoscopy) • Stable – Laparoscopy – Methotrexate – Expectant Ectopic Pregnancy: Treatment ACADEMIC EMERGENCY MEDICINE 2007; 14:755–758 Ectopic Pregnancy: Summary • Incidence has increased 4 fold since 1970. • 7% to 13% of pregnant patients presenting to ED’s with abdominal pain or bleeding have an ectopic pregnancy. Ectopic Pregnancy: Summary • History and physical can be misleading in ectopic pregnancy: – 10% no pain – 50% no risk factors – 25% "normal" pelvic 30% no bleeding 90% no adnexal mass 50% misdiagnosed initially • No single test is extremely reliable. An algorithm utilizing physical exam, early transvaginal ultrasound and quantitative ß-HCG seems to be the best. Ultasound Images in Early Pregnancy • In this transvaginal view, a 4.0 week size gestational sac is clearly seen (arrow). The uterus is outlined with arrowheads. Ultasound Images in Early Pregnancy • Gestational Sac Ultasound Images in Early Pregnancy • 4 to 4.5 weeks • Double sac sign, with the decidua capsularis (DC) and decidua parietalis (DP). Ultasound Images in Early Pregnancy • 4-5 weeks • Yolk Sac Ultasound Images in Early Pregnancy • 5 - 6 weeks • Fetal Cardiac Activity • Initially slow (110 bpm), then to 160 at 8 wks, then decreases through rest of first trimester Ultasound Images in Early Pregnancy • 5.5 - 6.5 weeks • Embryo elongation into fetal pole ED US Pitfalls • Pseudogestational sac is seen in 20-50% of ectopic pregnancies. Can be confused with double decidual sign. ED US Pitfalls • Pseudogestational sac ED US Pitfalls • Pseudogestational sac ED US Pitfalls • Twin gestation 7 weeks ED US Pitfalls • Threatened SAB with Clot ED US Pitfalls • Inevitable abortion • In this case the endometrial cavity (En) at the fundus is empty because the gestational sac (arrowheads) has been pushed into the cervix (Cx). Further Reading Summary • All women of reproductive age with GI or GU complaints need a ß-HCG • 7% to 13% of pregnant patients presenting to ED’s with abdominal pain or bleeding have an ectopic pregnancy. • History and physical can be misleading in ectopic pregnancy. • No single test is extremely reliable. An algorithm utilizing physical exam, early transvaginal ultrasound and quantitative ß-HCG seems to be the best. Questions?