Pulmonology and Respiratory
advertisement

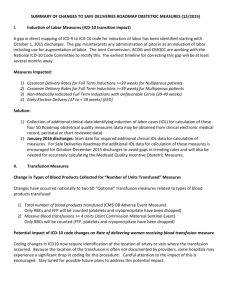
UHS, Inc. ICD-10-CM/PCS Physician Education Pulmonology and Respiratory 1 ICD-10 Implementation • October 1, 2015 – Compliance date for implementation of ICD-10-CM (diagnoses) and ICD-10-PCS (procedures) – Ambulatory and physician services provided on or after 10/1/15 – Inpatient discharges occurring on or after 10/1/15 • ICD-10-CM (diagnoses) will be used by all providers in every health care setting • ICD-10-PCS (procedures) will be used only for hospital claims for inpatient hospital procedures – ICD-10-PCS will not be used on physician claims, even those for inpatient visits 2 Why ICD-10 Current ICD-9 Code Set is: – Outdated: 30 years old – Current code structure limits amount of new codes that can be created – Has obsolete groupings of disease families – Lacks specificity and detail to support: • Accurate anatomical positions • Differentiation of risk & severity • Key parameters to differentiate disease manifestations 3 Diagnosis Code Structure 4 ICD-10-CM Diagnosis Code Format 5 Comparison: ICD-9 to ICD-10-CM 6 Procedure Code Structure ICD-10-PCS Code Format 8 ICD-10 Changes Everything! • ICD-10 is a Business Function Change, not just another code set change. • ICD-10 Implementation will impact everyone: – Registration, Nurses, Managers, Lab, Clinical Areas, Billing, Physicians, and Coding • How is ICD-10 going to change what you do? 9 ICD-10-CM/PCS Documentation Tips 10 ICD-10 Provider Impact • Clinical documentation is the foundation of successful ICD10 Implementation • Golden Rule of Documentation – If it isn’t documented by the physician, it didn’t happen – If it didn’t happen, it can’t be billed • The purpose in documentation is to tell the story of what was performed and what is diagnosed accurately and thoroughly reflecting the condition of the patient – what services were rendered and what is the severity of illness • The key word is SPECIFICITY – Granularity – Laterality • Complete and concise documentation allows for accurate coding and reimbursement 11 Gold Standard Documentation Practices 1. Always document diagnoses that contributed to the reason for admission, not just the presenting symptoms 2. Document diagnoses, rather that descriptors 3. Indicate acuity/severity of all diagnoses 4. Link all diseases/diagnoses to their underlying cause 5. Indicate “suspected”, “possible”, or “likely” when treating a condition empirically 6. Use supporting documentation from the dietician / wound care to accurately document nutritional disorders and pressure ulcers 7. Clarify diagnoses that are present on admission 8. Clearly indicate what has been ruled out 9. Avoid the use of arrows and symbols 10. Clarify the significance of diagnostic tests 12 ICD-10 Provider Impact The 7 Key Documentation Elements: 1.Acuity – acute versus chronic 2.Site – be as specific as possible 3.Laterality – right, left, bilateral for paired organs and anatomic sites 4.Etiology – causative disease or contributory drug, chemical, or non-medicinal substance 5.Manifestations – any other associated conditions 6.External Cause of Injury – circumstances of the injury or accident and the place of occurrence 7.Signs & Symptoms – clarify if related to a specific condition or disease process 13 ICD-10 Documentation Tips Do not use symbols to indicate a disease. For example “↑lipids” means that a laboratory result indicates the lipids are elevated – or “↑BP” means that a blood pressure reading is high These are not the same as hyperlipidemia or hypertension 14 ICD-10 Documentation Tips Site and Laterality – right versus left –bilateral body parts or paired organs Example – frontal sinusitis Stage of disease –Acute, Chronic –Intermittent, Recurrent, Transient –Primary, Secondary –Stage I, II, III, IV Example – stage of pressure ulcer: – L89.011 Pressure ulcer of right elbow, stage 1 – L89.021 Pressure ulcer of left elbow, stage 1 15 ICD-10 Documentation Tips Asthma – Specificity • • • • Intermittent [less than or equal to two times per week] Mild persistent [more than two times per week] Moderate persistent [daily-may restrict physical activity] Severe persistent [throughout the day-frequent severe attacks that limit the ability to breathe] – Type / Form • • • • • • • • • • • Childhood Exercise induced Extrinsic allergenic Late onset Allergic Allergic bronchitis Allergic rhinitis w/ asthma Atopic asthma Extrinsic allergic asthma Intrinsic non-allergic asthma Idiosyncratic asthma 16 ICD-10 Documentation Tips Asthma continued – Acuity •With acute exacerbation •With status asthmaticus – Tobacco Exposure •Exposure to environmental tobacco smoke •History of tobacco use •Occupational exposure to tobacco smoke – Cause and Effect – environmental •Detergent •Coal workers •Miners •Wood 17 ICD-10 Documentation Tips COPD – Type • • • • Chronic obstructive bronchitis Chronic bronchitis with airway obstruction Chronic bronchitis with emphysema Chronic obstructive tracheobronchitis – Acuity • With acute exacerbation • With acute lower respiratory infection – Specificity • With asthma • With bronchitis • With emphysema – Tobacco Exposure • Exposure to environmental tobacco smoke • History of tobacco use • Occupational exposure to tobacco smoke 18 ICD-10 Documentation Tips Influenza – Organism, document as known or suspected • Avian influenza • H1N1 influenza – Link associated conditions / manifestations • • • • • • Influenza with secondary gram negative pneumonia Laryngitis Pleural effusion Influenzal encephalopathy Influenzal myocarditis Influenzal otitis media 19 ICD-10 Documentation Tips Lung Cancer – Location • Detailed location of lesion site • Left, Right, Bilateral – Morphology • • • • Malignant, Benign Primary , Secondary In situ Uncertain behavior, Unspecified behavior – Histology • Identified by cytology, histology or pathology findings – Stage / Metastatic • Different, distinct locations – Different primaries – Metastatic sites 20 ICD-10 Documentation Tips Lung Cancer continued – Is patient being admitted for treatment of the neoplasm or an adverse reaction / complication? • Treatment - surgery, chemotherapy, immunotherapy, radiation • Adverse reaction of treatment – neutropenic fever secondary to chemo • Complication of the disease – anemia due to malignancy – Document if a complication is part of the disease process or an adverse effect of treatment • Anemia due to malignancy or due to chemotherapy – History of • Malignancies previously removed and no longer receiving active treatment • Clearly document for follow-up and medical surveillance 21 ICD-10 Documentation Tips Pneumonia – Type – bacterial, viral, fungal, aspiration, drug-induced – Organism, document as known or suspected • Viral – adenoviral, respiratory syncytial, parainfluenza, human metapneumovirus, viral unspecified • Bacterial – streptococcus, hemophilus, E coli, klebsiella, pseudomonas, staphlococcus, MRSA, MSSA, mycoplasma, bacterial unspecified – Link associated conditions / underlying conditions • Influenza with secondary gram negative pneumonia • Sepsis due to pneumonia • Acute respiratory failure due to pneumonia – Aspiration • Due to solids or liquids • Due to anesthesia during L/D or procedure • Due to anesthesia during puerperium – Laterality of lung involvement – left, right, both – Note whether ventilator associated (VAP) 22 ICD-10 Documentation Tips Respiratory Failure – Acuity - acute, chronic, acute on chronic – Specificity – with hypoxia or hypercapnia – Tobacco Use • Exposure to environmental tobacco smoke • History of tobacco use • Occupational exposure to tobacco – Does the patient require continuous home oxygen or is dependent on home oxygen – Differentiate pulmonary collapse from therapeutic collapse – Respiratory distress and respiratory insufficiency are NOT respiratory failure 23 ICD-10 Documentation Tips Respiratory Failure Criteria Acute Chronic Symptoms – difficulty breathing, shortness of breath, dyspnea, tachypnea, respiratory distress, labored breathing, use of accessory muscles, cyanosis, unable to speak Symptoms – severe COPD, chronic lung disease such as cystic or pulmonary fibrosis Ph < 7.35 & pCO2 > 50 or pO2 < 55 & FIO2 > 28 % pO2 < 55 or pCO2 > 50 Hypoxemia Hypercapnia pO2 < 60 mmHg OR pO2 / FIO2 ratio < 300 OR 10 mmHg decrease in baseline pO2 pCO2 > 50mmHg with pH < 7.35 OR 10 mmHg increase in baseline pCO2 24 ICD-10 Documentation Tips Drug Under-dosing is a new code in ICD-10-CM. – It identifies situations in which a patient has taken less of a medication than prescribed by the physician. • Intentional versus unintentional – Documentation requirements include: • The medical condition • The patient’s reason for not taking the medication – example – financial reason – Z91.120 – Patient’s intentional underdosing of medication due to financial hardship 25 ICD-10 Documentation Tips Codes for postoperative complications have been expanded and a distinction made between intraoperative complications and postprocedural disorders •The provider must clearly document the relationship between the condition and the procedure – Example: • D78.01 –Intraoperative hemorrhage and hematoma of spleen complicating a procedure on the spleen • D78.21 –Post-procedural hemorrhage and hematoma of spleen following a procedure on the spleen 26 ICD-10 Documentation Tips Intra-operative Post-procedural Accidental puncture / laceration Timing: •Post-procedure •Late effect Same or different body system Classify as: •An expected post-procedural condition •An unexpected post-procedural condition, related to the patient’s underlying medical comorbidities •An unexpected post-procedural condition, unrelated to the procedure •An unexpected post-procedural condition related to surgical care (a complication of care) Blood product Central venous catheter Drug: •What adverse effect •Drug name •Correctly prescribed •Properly administered Encounter: •Initial •Subsequent •Sequelae 27 ICD-10 Documentation Tips ICD-10-PCS does not allow for unspecified procedures, clearly document: • Body System – general physiological system / anatomic region • Root Operation – objective of the procedure • Body Part – specific anatomical site • Approach – technique used to reach the site of the procedure • Device – Devices left at the operative site ICD-10 Documentation Tips Most Common Root Operations: Control – stopping or attempting to stop Excision – cutting out or off without replacement a portion of a body part Repair – restoring, to the extent possible, a body part Restriction – partially closing an orifice or lumen of a tubular body part Dilation – expanding Extirpation – taking or an orifice or the lumen cutting out solid of a tubular body part matter Replacement – putting in a biological /synthetic material that takes the place or function Supplement – putting in a biological/ synthetic material to reinforce / augment Division – cutting into a body part to transect the body part Insertion – putting in a non-biological appliance Reposition – moving to Transfer – moving, its normal location without taking out, all or a portion of a body part to another location Drainage – taking or letting out fluids &/or gases Release – freeing a body part from an abnormal physical constraint Resection – cutting out or off without replacement all of a body part Transplantation – putting in all or a portion of a living part from another 29 individual or animal ICD-10 Documentation Tips Most Common Device Types: Diaphragmatic pacemaker lead Endobronchial valve Intraluminal device: plain, drug-eluting, or radioactive Drainage device Endotracheal airway Monitoring device Extraluminal device Infusion device Tracheostomy device Radioactive element 30 Summary The 7 Key Documentation Elements: 1.Acuity – acute versus chronic 2.Site – be as specific as possible 3.Laterality – right, left, bilateral for paired organs and anatomic sites 4.Etiology – causative disease or contributory drug, chemical, or non-medicinal substance 5.Manifestations – any other associated conditions 6.External Cause of Injury – circumstances of the injury or accident and the place of occurrence 7.Signs & Symptoms – clarify if related to a specific condition or disease process 31