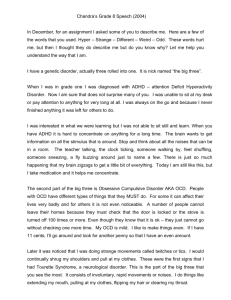
Cunningham-Tourettes-Presentation-edits
advertisement

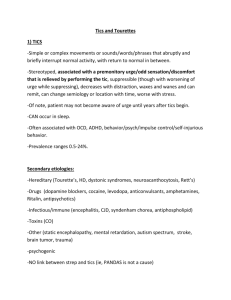
Tourette’s Disorder DSM-V Categorization: Neurodevelopmental motor Disorder: Tic Disorders Characterized with an onset in the developmental period, usually early in development Symptoms of excess as well as deficits/ milestone delays Deficits produce impairments including academic, personal, occupational and social functioning Frequent co-occurrence with other disorders DSM-V Tic Disorders • • • • Based on the presence of motor and or vocal tics Duration of symptoms Age at onset Absence of any other cause (substance use or medical condition) • Hierarchical rank: Tourette’s disorder Persistent motor or vocal tic disorder Provisional tic disorder Specified and unspecified tic disorder DSM-V Tics Tic: sudden, rapid, recurrent, nonrhythmic motor movement or vocalization (DSM-V) Motor Tic Simple motor tics Complex motor tics Video Vocal Tic Simple vocal tics Complex vocal tics Coprolalia- obscene inappropriate words or phrases Echolalia- repeating others’ words Palilalia- repeating own words DSM-V TS Development/ Course • • • • • • • 4-6 average onset Severity around 10-12 then a decline in adolescence (small percentage worsen in adulthood) Across lifespan tic symptoms manifest/ wax and wane idea Muscle groups and vocalizations change over time With age comes a premonitory desire [somatic sensation] followed by a feeling of relief after expressing the tic Particular pattern of tics, desire to express “just right” Vulnerable to co-occurring conditions during “age of risk” and then followed by decline Meeting DSM-V Diagnostic Criteria for TS • A. Both multiple motor and one or more vocal tics have been present at some time during the illness, although not necessarily concurrently. • B. The tics may wax and wane in frequency but have persisted for more than 1 year since first tic onset. • C. Onset is before age 18 years. • D. The disturbance is not attributable to the physiological effects of a substance or another medical condition. DSM-V Prevalence/Cultural influences • Childhood onset is common, but tics are usually transient • 3 to 8 per 1,000 school aged children • Males > females (2:1 to 4:1), no gender differences in kinds of tics • African Americans and Hispanic Americans < identified cases • Race, ethnicity, and culture: no varying clinical characteristics, but instead may influence perception and management of disorder (choice of treatment) CHARACTERISTICS OF TICS • Mild, moderate or severe- dependent on: frequency, forcefulness, complexity and daily life impairment • Frequency does not equal impairment: eye blinking 2030 per minute vs. loud barking several times an hour • Most individuals experience oscillations in severity over weeks and months (waxing and waning) • Involuntary but some report “semi-voluntary” based on suppression ability • Premonitory urges followed by satisfaction after tic is completed • Individuals may disguise tics as purposeful: arm jerk – comb hair DSM-V Risk and Prognostic Factors • • • • • • • Temperamental: Tics are worsened by anxious, excited and exhausted emotions Tics are better when individual experiences calmness and is focused Environmental: Observation of a gesture/sound may result in individual with tic disorder to imitate (can be perceived incorrectly/purposeful) Hinders interaction with authority figures Genetic/Physiological: Expression and severity influenced Risk alleles and rare genetic variants have been identified Obstetrical complications/older paternal age/maternal smoking during pregnancy and lower birth weight associated with tic severity DSM-V Functional Consequences • Many individuals do not experience impairment with their tics and may even be unaware of their tics • More severe cases usually result in daily living impairments (not definitive, some severe cases may function just fine) • Co-occurring conditions can lead to greater impairment • Less often tics lead to social isolation, interpersonal conflict, peer victimization, inability to work/attend school, poor quality of life • Rare complications include: physical injury, orthopedic injury and neurological injury COMORBIDITY • In addition to tics, many experience co-occurring psychiatric and or neuropsychological difficulties • Most frequent: ADHD (50%), related learning disorders, OCD (20-60%), anxiety disorders, affective disorders, sensory integration dysfunction and explosive aggressive behaviors • Not necessarily etiological, many influences possible Genetic/ Physiological Mechanisms Comorbidity: ADHD/OCD Age Tic severity <18 onset of motor/vocal tics Environment Temperament Secondary Features: Neurological, orthopedic, physical injury Functional impairment Problems with teachers, parents and law enforcement DO WE HAVE EVIDENCE IN RESEARCH? PERSPECTIVE IS KEY • Some researchers view TS as a discrete single entity with accompanying syndromes • Others view TS with common causes and varying manifestations more like a spectrum disorder • When reviewing research regarding TS critical to understand population requirements for TS groups ADHD • More than 50% with TS who come to the attention of physician – ADHD • 30% with TS experience school difficulties/learning disabilities • Special care to be taken in medication-stimulants may worsen behaviors/tics • Relationship between ADHD/TS less understood (O’Rourke et al., 2011) • Suggested overlapping neurobiology: ADHD/OCD/TS (O’Rourke et al., 2011) OCD/anxiety OCD: • Many with TS may also have obsessive-compulsive symptoms (OCS) • Disruptive to life and to tics • Need to “even things up”, “feel right”, touching forbidden objects (hot frying pan) • Complex tic or compulsion • Special care to be taken in medication: antipsychotic vs. SSRI Anxiety: • Unknown if genetically related to TS • Avoidance behavior common: reluctance to go to school or other activities (sleepovers) TEMPERAMENTAL INFLUENCES • • • • • • • Individuals with TS- higher levels of aggression, hostility and personality disorder (Robertson et al., 1997) Tics have been “associated” with increased neuroticism/ additional OCD diagnosis also showed low extraversion (Cath et al., 2001) Comorbid ADHD “associated” with emotional instability Severe OCD symptoms-emotional hypercontrol (Balottin et al., 2009) Schizotypical personality traits-more common in TS population (Cavanna, Robertonson, & Critchley, 2007; Comings & Comings, 1987) TS has been “associated” with significant differences in QofL aspects (home, peer and family interactions) (Eddy, Rizzo, Gulisano, Agodi, Parchitta, Cali, et al., 2011) 88% of individuals with TS report tics having an effect on their life-potential to influence perceptions of abilities and feelings about themselves (Eddy, Rickard, Critchley & Cavanna) EXPLOSIVE/AGGRESSIVE BEHAIVOR • 25-70% of patients with TS report outbursts and anger issues (factor analysis accounting for 62.5% of variance) (Budman, Rockmore, Stokes, & Sossin, 2003) • Kicking, screaming, threatening others, biting, hitting, fits of anger/rage, punching holes in walls • Individuals typically afraid of their own behavior • “Run it’s course” nature • Thin barrier between outward expression and impulses/thoughts • Causes problems with teachers, families, and patients themselves Personality Influenced 25 adult outpatients, TS clinic, all fulfilled DSM-IV-TR criteria for TS Comprehensive clinical interviews- National Hospital Interview Schedule for TS Participants completed: Ten Item Personality Index, Beck Depression Inventory, Positive and Negative Affect Schedule, & Yale Global Tic Severity Scale Group scores were compared: TS patients vs. controls, between-group analysis subgroup of ‘pure TS’ to controls Results: No significant differences on: BDI, PANAS positive or negative subscales, or the TIPI agreeableness scores Significant difference between groups for four other TIPI scores (extraversion: MWU = 170.5, p = 0.005; conscientiousness: MWU = 204, p = 0.033; emotional stability: MWU = 130.5, p<0.001; openness: MWU = 196.5, p = 0.022) Correlations: significance for emotional stability scores negatively related to BDI (SR= -0.501, p = 0.011, PANAS negative subscale scores (SR = -0.482, p = 0.015) and positively related to PANAS positive subscale scores (Sr = 0.682, p<0.001). TIPI emotional stability negatively related to BDI scores (Sr = -0.891, p<0.001) and positively related to PANAS positive subscale scores (Sr = 0.619, p = 0.014) Behavioral Influences • Self-Injurious Behaviors (deliberate/repetitive infliction of self-harm) • Skin/scab picking, hair pulling, pinching oneself, selfbiting • Study focused on the relationship between SIB and other behavioral features that commonly co-occur with TS (Mathews et al., 2004) ~300 subjects with TS participating in three genetic studies • Analyzed SIB, obsessions, compulsions, tic severity, attention deficit hyperactivity disorder related impulsivity, risk taking behaviors, and rages Stress Related INFLUENCES • Life events are commonly used for the purpose of measuring stress • • Stressful life events and TS relationship is unclear Tic expression may be involved (Meidinger et al., 2005; Woods & Himle, 2004) • Impact of stressful life events and tic severity is best predicted by parental report (Lin et al., 2007) • Comorbid OCD: more stressful life events than controls (Findley et al., 2003) ENVIRONMENTAL INFLUENCES • • • • • • • • • Literature review Antecedent vs. Consequence Factors Fatigue and social activities- exacerbate tics Concentration, studying, relaxation- attenuate tics Limited to applying these findings to population or even other clinical samples because of self-report issues and reported in aggregate form Negative consequences reported to have negative or neutral outcomes Positive consequences resulting in positive outcomes Consequences were parent reported Generalizability unclear, overall however, stressful frustrating or anxiety provoking events reported to exacerbate tics ENVIRONMENTAL INFLUENCES • ‘tic-talk’ condition found to increase frequency of vocal but not motor tics (Woods, Watson, Wolfe, Twohig, & Friman, 2001) • Tics found to increase in presence of certain people (teacher, custodian, father, mother, examiner) (Malatesta, 1990) • Videotaping of children watching emotional video- most severe tics at specific emotional states, least severe in anger/happiness LIMITATIONS IN UNDERSTANDING CONTEXTUFAL FACTORS • The studies reviewed examined the relationship in experimental settings • Isolating certain variables would be most helpful in applying these findings to treatment interventions • Little information about the premonitory ‘urge’ in the development of the disorders • Most interesting but still unknown: Is it tics themselves that are impacted by contextual factors or is it the suppression/inhibitory behaviors that are being changed? GENETIC INFLUENCES • • • • • Previous studies have sought to identify several chromosomal regions associated with the susceptibility loci for TS TS and Chronic motor tics among first-degree relatives 2.0% and 12.0% (respectively) Morbid risk for TS among relatives: 9.8%-15% When replicated, results typically do not hold Difficult to extract out comorbid ADHD in findings, unable to conclude TS specific findings (< 10% of patients account for ‘pure’ TS population (Ozonoff et al., 1998; Mahone et al., 2002) Neurological influences • Suggested involvement of the frontal cortex connections to subcortical regions including basal ganglia through the frontal cortico-striatal-thalamocortico circuits (Mink, 2001; Singer, 2005; Albin and Mink, 2006) • Suggested abnormality in brain systems that effect neural transmission from limbic to motor systems deficit in regions involved with motivation and action (Jeffries et al., 2002) • Involvement with frontal cortex including response inhibition and selective attention (Bornstein et al., 1991; Johannes et al., 2001; Channon et al., 2003) GENETIC/ PHYSIOLOGICAL INFLUENCES • rs-fcMRI used to explore the possible disruption of brain systems in patients with TS (Fair et al., 2007a, 2008; Fransson et al., 2007) • Defects in neural circuits from the cerebral cortex through the structures constituting the basal ganglia and back to the cerebrum (Olson, 2004). • Cingulo-opercular network: maintenance of tasks sets across events within task period • Fronto-parietal network: rapidly adaptive online control • TD: strength of correlation coefficients ‘between’ differences in control networks seem to be stronger in children and decline with age (Fair et al., 2007) • Consideration of TS behaviors lead to theory of 3 GENTIC/ PHYSIOLOGICAL INFLUENCES • Largest off-curve differences found mostly in fronto-parietal network (adaptive control-/ controlling settings from one event to the next) • Immaturity in connections may be related to adaptive control network being more vulnerable to distraction while cinguloopercular network (set-maintenance) stable and resistant GENTIC/ PHYSIOLOGICAL INFLUENCES • Results for TS showed underdevelopment in 10-15 year olds, instead reflecting 7-9 year old • Groups of adolescents TD and with TS: 34 functional connections (p < 0.05) but after Benjamini and Hochberg False Discovery Rate correction, no emphasis produced • Connections examined using rs-fcMRI show weaker functional connections WHAT DO These DIFFERENCES MEAN? • As mentioned, fronto-parietal network is associated with supporting online task-control while allowing for adaptive change from one event to the next (disruption here might make sense for the increase in severity in different environments that produce a change in emotion (going from calm to excitement, > frequency and severity of tics) • The fronto-parietal network has also been hypothesized as being more susceptible to distraction which would make transient control impaired • Adolescents with TS (10-15) may have less Genetic influences • 6 family studies have previously looked into familial related conditions in TS (5- US & Europe, 1-Japan) • Interviews from first degree family members • Found morbid risk of 9.8-15% among relatives • 15-20% for other tics • Age correct rates among first degree relatives 2.0-12% • More recently, researchers suggest inheritance Problems with Genetic association/linkage studies ASSOCIATION: • Case control or family based • Limited by many irrelevant markers appearing to be disease associated • High rates of false positives • Population stratification- cases and controls differ not only with phenotype of interests but overall population genetic ancestry • Difficult to find appropriate control group Problems with Genetic association/linkage studies • LINKAGE (Pauls, 2003): • Members of the Tourette Syndrome Association International Consortium on Genetics (TSAICG) conducted all initial linkage studies • 31 multigenerational families were studied • > 800 genetic marker loci were screened • No strong positive evidence found for linkage with TS • Re-conducted by TSAICG in sib-pair study of 76 families • 64 had only two affected siblings • 10 had three effected siblings Review • Temperament, environment, & genetics/physiology in relation to TS commonly produced inconclusive research findings • Tic severity may to be influenced by awareness, context, age, & comorbidity • Immature connectivity throughout neurological regions have been measured and may influence the inability to inhibit unwanted behaviors • Research findings of TS struggle to be Neuroanatomical/ Genetic Substrates Comorbidity ADHD/OCD Age Awareness of Behaviors Motor Tics/ (simple or complex) Vocal Tics Socialization/ Peer- acceptance/ Quality of relationships Academic/ Behavioral Functioning Stress/Anxiety/ Fatigue/Inattentio n Inhibitory deficits Tic Severity Cunningham TS Model 2013 Self-Injury Inattentiveness Aggression Functional Impairment Deficits in relationships REFERENCES American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. Balottin, U., Rossi, M., Rossi, G., Vigano, L., Salini, S., Lanzi, G, et al. The rorscharch test and gilles de la tourette’s syndrome: A pilot case control study. Brain Development, 31, 657-665. Bloch, M. H., & Leckman, J. F. (2009). Clinical course of tourette syndrome. Journal of Psychosomatic Research, 67, 497-501. Brito, G. N. O. (1997). A neurobiological model for tourette syndrome centered on the nucleus accumbens. Medical Hypotheses, 49, 133-142. Budman, C. L., Rockmore, L., Stoke, J., & Sossin, M. (2003). Clinical phenomenology of episodic rage in children with tourette syndrome. Journal of Psychosomatic Research, 55, 59-65. Cath, D. C., Spinhoven, P., Landman, A. D., & van Kempen, G. M. J. (2001). Psychopathology and personality characteristics in relation to blood serotonin in tourette’s synfrome and obsessive-compulsive disorder. Journal of Psychopharmochology, 15, 111-119. Church, J. A., Fair, D. A., Dosenbach, N. U. F., Cohen, A. L., Miezin, F. M., Peterson, S. E., & Schlaggar, B. L. (2009). Control networks in paediatric tourette syndrome show immature and anomalous patterns of functional connectivity. Brain, A Journal of Neurology, 132, 225-238. Conelea, C. A., & Woods. D. W. (2008). The influence of contextual factors on tic expression in tourette’s syndrome: A review. Journal of Psychosomatic Research, 65, 487-496. Eddy, C. M., Rickards, H. E., Critchley, H. D., & Cavanna, A. E. (2013). A controlled study of personality and affect in tourette syndrome. Comprehensive Psychiatry, 54, 105-110. Findley, D. B., Leckman, J. F., Katsovich, L., Lin, H., Zhang, H., Grantz, H. et al. (2003). Development of the yale children’s global stress index (YCGSI) and its application in children and adolescents with tourette syndrome and obsessive-compulsive disorder. Journal of American Academy of Child Adolescent Psychiatry, 42, 450-457. Jeffries, K. J., Schooler, C., Schoenbach, C., Herscovitch, P., Chase, T. N., & Braun, A. R. (2002). The functional neuroanatomy of tourette’s syndrome: An fdg pet study III: Functional coupling of regional cerebral metabolic rates. Neuropsychopharmacology, 27, 92-104. Leckman, J. F. (2002). Tourette’s syndrome. The Lancet, 360, 1577-1586. Lin, H., Katsovich, L., Ghebremichael, M., Findley, D. B., Grantz, H., Lombroso, P. J., et al. (2007). Psychosocial stress predicts future symptom Child severities in children and adolecents with tourette synfrome and/or obsessive compulsive disoder. Journal of Psychology and Psychiatry, 48, 157-166. Pauls, D. L. (2003). An update on the genetics of gilles de la tourette syndrome. Journal of Psychosomatic Research, 55, 7-12. Robertson, M. M., Banerjee, S., Hiley, P.J. F., & Tannock, C. (1997). Personality disorder and psychopathology in tourette’s syndrome: A controlled study. Br J Psychiatry, 171, 283-286. Steinberg, T., Shmuel-Baruch, S., Horesh, N., & Apter, A. (2013). Life events and tourette syndrome. Comprehensive Psychiatry, 54, 467-473.