DD meeting notes 8-29
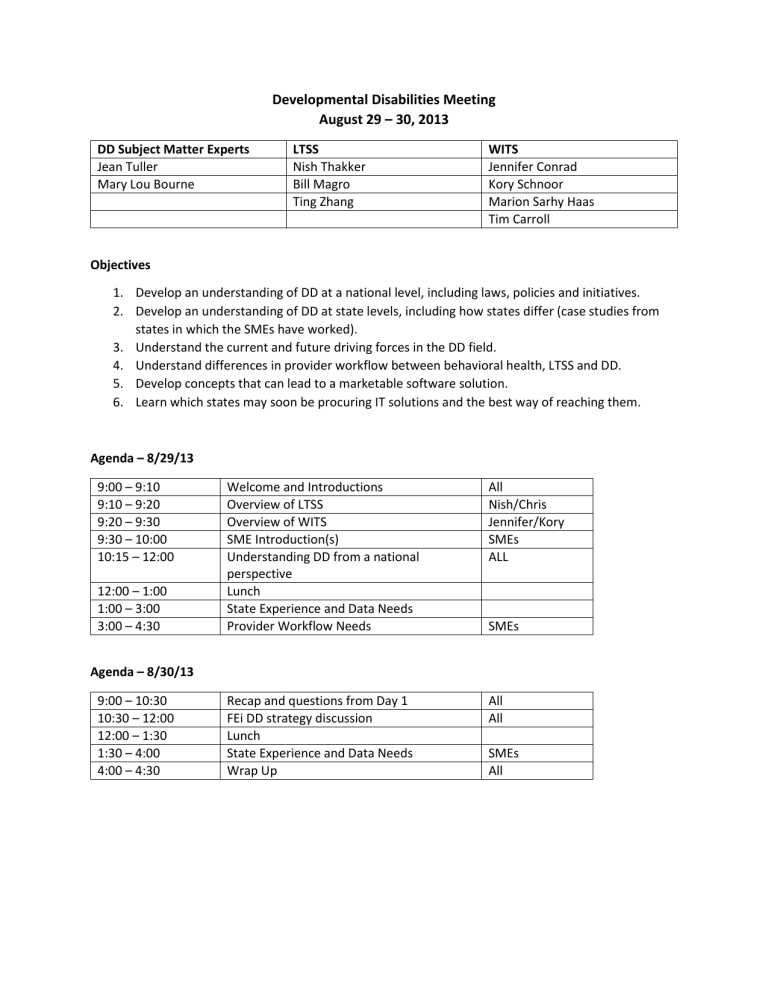
Developmental Disabilities Meeting
August 29 – 30, 2013
DD Subject Matter Experts
Jean Tuller
Mary Lou Bourne
Objectives
LTSS
Nish Thakker
Bill Magro
Ting Zhang
WITS
Jennifer Conrad
Kory Schnoor
Marion Sarhy Haas
Tim Carroll
1.
Develop an understanding of DD at a national level, including laws, policies and initiatives.
2.
Develop an understanding of DD at state levels, including how states differ (case studies from states in which the SMEs have worked).
3.
Understand the current and future driving forces in the DD field.
4.
Understand differences in provider workflow between behavioral health, LTSS and DD.
5.
Develop concepts that can lead to a marketable software solution.
6.
Learn which states may soon be procuring IT solutions and the best way of reaching them.
Agenda – 8/29/13
9:00 – 9:10
9:10 – 9:20
9:20 – 9:30
9:30 – 10:00
10:15 – 12:00
Welcome and Introductions
Overview of LTSS
Overview of WITS
SME Introduction(s)
Understanding DD from a national perspective
Lunch
State Experience and Data Needs
Provider Workflow Needs
All
Nish/Chris
Jennifer/Kory
SMEs
ALL
SMEs
12:00 – 1:00
1:00 – 3:00
3:00 – 4:30
Agenda – 8/30/13
9:00 – 10:30
10:30 – 12:00
12:00 – 1:30
1:30 – 4:00
4:00 – 4:30
Recap and questions from Day 1
FEi DD strategy discussion
Lunch
State Experience and Data Needs
Wrap Up
All
All
SMEs
All
General Questions
1.
What is the scope of services for Developmentally Disabled?
2.
Do all states have a standard definition of DD, including functional, psychological and physical impairments?
3.
How are DD services funded from the Federal government?
4.
What are the general federal reporting requirements?
5.
What are the responsibilities of the State Councils on Developmental Disabilities?
6.
Do states conduct audits/reviews of patient cases? If so, how are those generally conducted?
7.
How do DD agencies coordinate overlap with MFP and BIP
States’ Experience / Use Case (Pick a state(s) and tell its story)
1.
What are the state’s data needs?
2.
What is the state’s interaction with its providers / payers?
3.
What are the eligibility criteria and requirements?
4.
What is a general scenario an individual with DD would go through?
5.
What are the key attributes of states that provide DD services well?
6.
What are the standardized assessments they use, if any?
7.
Are care plans required for DD individuals? If so, how often are these completed?
8.
How do DD state agencies coordinate / overlap with MFP and BIP?
9.
How do DD clients interact within a health home setup?
Provider Experience / Workflow
1.
Explain the various types of providers involved in DD.
2.
How do DD agencies coordinate overlap with MFP and BIP?
3.
What are the things that are essential to your care plan?
4.
What types of medical interactions do the providers have with the individuals?
5.
What are the interactions between DD and behavioral health?
6.
What are the key functionalities that providers may need to use in a system?
7.
What is the provider interaction with case management entities?
Tribal – Medisked (the system that they selected for a provider in DC)
Understand the universe of social justice, dead heads, 62 yo, very intense, good to have,
Willowbrook state school – look up
Christmas in Purgatory
Syracuse
Halderman v Pennhurst
Even back then, CMS handled the bulk of the funding so more money and better care in these institutions than you would have in MH (where institutions are state run). Some family involvement but much more organized
1970s – Readiness model (continuum of services). Wolfensberger – Normalization and model coherency
People should have same rights in the community they live in
People first – self-advocacy group (self advocates becoming empowered – SABE) – clearinghouse for self help groups (get into the group in MD)
1980s – home like, supported employment, Katie Becket waiver (first DD waiver) – more republican when it comes to closing institutions (because dems favor union labor),
Oregon K Plan (funding for dd that is state driven but supported by feds). Austerity, cuts in funding, give more control to families
Current – mandate for self-direction, contribute to the economy
Describe the people with DD:
1.
Nomenclature a.
People (not patients) b.
There is client language related to a database system c.
Even in an institution they are not called patients
2.
Assessments – is in terms of what they need so that they “can do” (not what they can’t do)
3.
Demographics a.
Onset by age 18 b.
IQ of 70; can have a physical component as well c.
3 of 7 ADLs d.
Diagnoses – could have a diagnosis like autism, but would need the cognitive disability as well
4.
Mixture of funding and services based on the diagnostic mix
5.
Services – a.
School – i.
separate schools if significant behavioral challenges ii.
mainstream in classroom – with IEP
b.
Majority of service providers are parents c.
Case management or services coordination (e.g., install a ramp) d.
Supported living (live on your own but someone comes in to help) e.
Foster care f.
Bartered services (more able person helps the individual 5-9pm, has a day job, gets free room and board) g.
Group home h.
Sheltered workshop i.
Day habilitation (no employment – activities, adl skills) ii.
Day program – contract with an employer to do work iii.
Supported employment iv.
Self directed states, the dd individual hires a friend (who is a qualified provider) to help him instead of a more “official” provider
Payment
Community state plan 1915(k) –
States don’t like the I and k because under federal law you have no limit on slots, so they try to limit the quals on assessment or who can get it. If you need to change it, you have to do an amendment.
1.
State incentive to move c plans over to k plans is a 6 percent match from CMS
2.
OR-All 24-hour residential will be under the K plan
3.
K is new, behaves like ATR, watch the burn rate – a.
Controls – medical financial and technical
4.
Feds – a.
money through CMS b.
HHS- ACL – Administration on Aging, AIDD c.
DOE - Voc Rehab
5.
State – state match
6.
Sometimes counties (depends on state) -
7.
Funding goes to Medicaid who works with state DD agency a.
MD DD agency has their own funding (community and residential) b.
Bill to the state treasury – goes through MMIS system
Issues –
1.
Quality of direct support staff
2.
Fraud, waste and abuse
3.
Punch-in, punch-out
4.
Burn rate monitoring for the more open waivers like CFC
Provider needs:
1.
Billing Medicaid and third party
2.
Tend to be non-profits
3.
Managing vacancies (person in hospital for a set amount of time)
4.
Pharmacy and ePrescribing
5.
Medical complication
6.
Incident reporting
7.
Infection control
8.
There are not that many companies that have real-time (web based) systems a.
Therap – in a lot of states, but not intuitive and user friendly
9.
If the state adopts it, the provider will use it.
10.
State does have the right to see data on individuals, can go do audits, a.
Reporting up on the 6 assurances – driven by the case management agency
Does dd get exempted from Medicaid managed care:
Data reporting requirements – come out of the waiver reporting process –
1.
1915c waiver for HCBS – what are the 6 basic assurances a.
How do they report it – the county puts together the data into a document and submits it, b.
Collect data on what you control c.
Random audit of a number of files on people -
2.
Ideal situation – query on ongoing basis
Case Manager – state or county – or provider
1.
Develop plan of care (and get sign off) a.
May have to send to Medicaid – but mostly not
2.
Make sure it’s implemented
3.
Monitor it
The plan of care will go over services – usually the checks come in with the billing component – when services are billed, were they authorized? Were they in the plan of care? Sometimes will have an ASO to do this portion. Medicaid delegates to the DD agency, but they are on the hook.
Provider system example
1.
Intake done at city/state
2.
Get the client and develop plan of care
3.
Authorization received for authorizations
4.
Tracking a.
Staff b.
Clinical notes c.
Inventory of staff and supplies
5.
Billing
6.
Reporting (key performance indicators, dashboards, budget, historical)
Service plan –
1.
Addresses the intensity of person’s service needs
2.
One service plan per person
3.
Usually there is a template at the state level, this is filled out by the state
OR Homegrown functional needs assessment (ADL – IADL measurement)
Supports and intensity scale
RIA – expensive and time consuming
MediSked
1.
Providers, trying to get into the state market. Trying to get into state (good relationship with
ARC)
2.
Ease of use
3.
Could interface with financials
4.
They build around the schedule for the person – different than other competitors.
5.
Forces staff to stick to the schedule
6.
Included pharmaceutical – prescribe
7.
Healthcare information can be uploaded
8.
Track measurable objectives for each person (goals in the ISP – track if they were met)
9.
Dedicated staff who worked with the provider to bring this up; train the trainer
10.
Gave “new” things for free; charge for the rest
Mark Fenton (MA)
Family support
School admin
Family referrals
ARC agencies
Send them through the intake process – info, application, verification, confirmation, Medicaid eligibility, waiver eligibility, assessment tool – devel temporary ISP
Template – ISP
Very person focused
Dates
Pull in functional needs assessments
State (OR) has functional needs assessment – and can use that to provide the approval for services
Billing electronic – checked against authorization
State level challenges:
1.
Not universal record systems
2.
No audit tools that are easily electronic
3.
Billing interface with providers – need it smooth
4.
Triggers for Medicaid compliance
5.
Don’t have a system that is more integrated (except maybe PA and MA)
6.
Outcomes – not many
How would a state pay for a system – federal grants – elevated admin match to install IT, year end savings, legislative allocation
Oregon
Vermont and NH – independent agencies that are providers
NC/MI – DD waiver
Vermont is the future of DD – ahead of the curve
Graystone CES (Focus innovations) – DD software product. South Dakota, family support waiver, ISP, spend down/burn rate monitoring
Look at self-directed states – worker hours, etc.
Rushmore-group.com – possible partner company
Vancouver – costing outcomes in DD -
Family portal - the words you use here will be more important – think instead of client and case, how would I talk about myself; in dropdowns, think through
NOTES FROM 8/30/13
1.
WITS – the idea of agencies managing their own staff set up is great but isn’t found anywhere
2.
DD provider entry tends to be all over the place - so the idea of templating plans and notes is a very good one because the usually it is disorganized and therefore too much is required.
Mary lou slides
She has a presentation on BH and DD and how they intersect – we need her to give this to us in another meeting
1.
Preferences – what’s important to me
2.
Status in life
3.
Plan centered like facebook
4.
Not really medical model, dx is not very important
5.
CMS – person centered planning,
6.
Person centered planning – preferences of the individual, not just the health and safety; 4 models are out there.
7.
State required care plan, min goals, services, frequency and duration, and provider – most states go beyond that
8.
Build person centered care into the system – not much unlike ROSC - resiliency and recovery – in
SA
State ideas:
1.
Collaborate with states – with the DD people and the Medicaid people – what is the relationship?
2.
Are they compliance focused? Or are they learning focused?
3.
Are the providers suppliers or minions? Do they involve them in the discussion about needs?
4.
Are community advocates partners or angry?
5.
Getting DD out of their own corner and providing more integration could be very good.
6.
MH issues are higher in people who have DD; SA less so.
7.
Service coordination is important and gets complicated because of turf issues.
Linking into pharmacy is an immediate need.
Access to records and interchange (but remember that providers in DD are not medical providers). Still covered by HIPAA
IT system would help to identify the ability to measure outcomes (benchmark data around satisfaction –
HSRI – 32 states use it NASDDI has access. Reporting benchmarks across states (finally). This is an opportunity because it needs to be done, but its not really being done
EVV, audit capability, authorized services,
Recertification for the
Assessment of the persons needs and of the services – SIS is one that is taking off (it is proprietary); this crosswalks to funding better than others do.
What are they interested in learning, what do we do to get them there, how do we measure that from an outcomes,
Service delivery - progress on goals, documentation,
Other DD System components:
Provider qualification and enrollment
Incident management (reportable events)
Quality management - cms assurances and reports
Financial structure
Self-directed services (family is provider)
Training and staff development
++++
Needs assessment is typically done after individual comes off the waitlist
This is the full on assessment – that determines full on services that are needed by the individual
That’s when you can begin building the ISP
Need to be able to easily update the contact info and the collateral contacts
Health risks
Preferences
Support
Services
Goals/actions
Time to redo assessment and plan at the same time from a provider standpoint
How dd agencies overap with mfp and bip? (so mfp is so different on a state to state basis)
+++++++++++++
FOCoS – Julie Jester – is CEO (have been in conversations with HI DD for a while)
They have also been talking with Rushmore group in SD
Harkins – IA is the only senator who cares.