Red Blood Cell Physiology: Erythron & Respiratory Pigments
advertisement

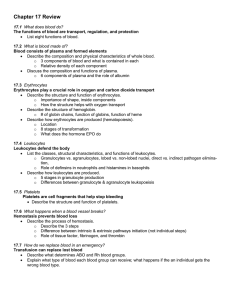
Physiology of red blood cells. Erythron. Respiratory pigments Blood system Blood system firstly was proposed by Lung in 1936. It consist of - blood circulated through the blood circulatory system - blood forming organs - blood destroying organs - regulatory apparatus. Blood Blood is a fluid connective tissue. Blood consist of - plasma - blood cells: 1. erythrocytes, 2. leucocytes, 3. platelets. Function of blood Functions of blood 1. Breathing function of blood. 2. Trophic function of blood. 3. Excretory function of blood. 4. Hormonal regulation. 6. Temperature regulation. 7. Maintaining the acid-base balance of tissues. 8. Supporting the water-electrolytic balance. 9. Homeostasis function. 10. Protecting the body from bacteria and other organisms that can cause diseases or other abnormal conditions. Functions of Blood Transport of: – Gases, nutrients, waste products – Processed molecules – Regulatory molecules Regulation of pH and osmosis Maintenance of body temperature Protection against foreign substances Clot formation Production of Erythrocytes: Erythropoiesis Quantity (volume) of blood, the concept of its deposit In adult in normal blood, relative to total body weight, is 6.8%. Newborns - 15%. Part of the blood is in the depot: liver - 20%, in the skin, subcutaneous vascular plexus - up to 10%, in the spleen - up to 1.52% of blood. Deposited blood in comparison with blood circulating in the vessels is 10-20 times slower than blood cells. . Human blood smear X 500 Quantity of cells, their changing Erythrocytes In men – 4,0-5,1 Tera/L; in women – 3,7-4,7 Tera/L. The quantity of erythrocytes may be increase – in pregnancy, in physical training, mental work, in newborn or decrease. Leukocytes - 4-9 Giga/L. The number of leukocytes can increase – physical work, emotional load, in newborn, inflammation or decrease. Platelates - 180-320 Giga/L. Blood cells Plasma Water – 90 % Solids – 10 % Inorganic chemicals: sodium, calcium, potassium, magnesium, chloride, bicarbonate, phosphate, sulfate – 0,9 % Organic chemicals: Proteins: serum albumin, serum globulin, fibrinogen – 8 % Others: – 1,1 % Nonprotein nitrogenous substances: urea, uric acid, creatine, creatinine, ammonium salts, amino acids Nonnitrogenous substances: glucose, fats, cholesterol hormones Gases: oxygen, carbon dioxide, nitrogen Components of Whole Blood Plasma (55% of whole blood) Buffy coat: leukocyctes and platelets (<1% of whole blood) 1 Withdraw blood 2 Centrifuge and place in tube • Hematocrit • Males: 40-48% • Females: 36- 42% Erythrocytes (45% of whole blood) Formed elements Proteins One liter of plasma has 65-85 gram of proteins. Concentration of albumins is 35-50 g/L; globulins is alpha-1-globulins – 1-4 g/L, alpha-2-globulins – 4-8 g/L, beta-globulins – 6-12 g/L, gamma-globulins – 8-16 g/L; fibrinogen – 2-4 g/L. Plasma which are not contain fibrinogen called serum (it is necessary for understanding the immunology, therapy etc.) Functional significance of plasma proteins Albumin: 80% defines oncotic pressure transfer bilirubin, urobilin , fatty acids , antibiotics , sulfonamides , are formed in the liver , 17 g per day. Globulin. In a fraction of α1- globulins are proteins associated with carbohydrates. The fraction of α2- globulins include protein ceruloplasmin, thyroxine binding protein , vitamin B12 -binding globulin , angiotensin . By β- globulins include transfer of lipids, polysaccharides and iron. Antibodies are mainly γ- globulins. Globulins are synthesized in the liver , bone marrow , spleen and lymph nodes. By day 5 grams of globulin synthesized Fibrinogen . (2-4 g / L) takes part in the formation of a blood clot . Formed exclusively in the liver. Buffer systems of blood Maintaining a constant acid-base balance of blood provided by buffer systems: 1. Bicarbonate buffer: Н2СО3 + ОН– ⇄ НСО3– + Н2О, НСО3– + Н+ ⇄ Н2СО3 2. Phosphate buffer: Н2РО4– + ОН– ⇄ НРО42– + Н2О, НРО42– + Н+ ⇄ Н2О4– 3. The protein buffer: RСООН + ОН– ⇄ RООС– + Н2О, RСОО– + Н+ ⇄ RООН 4. Hemoglobin buffer. Essentially, there are two hemoglobin buffers - one based on reduced hemoglobin: NNb/Nb- and the other based on oxyhemoglobin: NHbO2/HbO2. First prevails in the venous blood, and the second - in the arterial: НHb + ОН– ⇄ Нb– + Н2О; НHbО2 + ОН– ⇄ НbО2– + Н2О, Нb– + Н+ ⇄ ННb; НbО2– + Н+ ⇄ ННbО2 Evaluation of acid-base balance is performed on the following parameters: 1. pH (from Eng. power Hydrogen - the power of hydrogen), which is equal to 7,35-7,45. 2. Tension of CO2 - pCO2, which is normally 5,3-6,1 kPa (4046 mm Hg). 3. Standard bicarbonate, international designation SB (standart bikarbonate) - estimated. At standard conditions is 20-27 mg / dL. 4. True, actual bicarbonate, international designation AB (actual bikarbonate), is 190-25 mg / dL. 5. Excess (deficiency) framework, international designation CE (D) (base ecxess (deficit) equals ± 2,3 mmol / l. 6. The sum of the bases of all the blood buffer systems, international designation BB (batter bases) is 40-60 mg / dL. Destruction of red blood cells The destruction of hemoglobin EXCHANGE IRON IN THE BODY The basic amount of iron in the body (57.6%) is part of hemoglobin in red blood cells and is found. Iron enters the body in the food (meat, liver, fish, rice, peas, raisins, apricots). It is best absorbed iron, which is part of the food in the form of heme. The functions of red blood cells Transport function. Red blood cells carry: O2, CO2, NO, adsorbed proteins, drugs, physiologically active substances. Provide acid-base balance. Maintaining the ionic composition of the plasma. Hemostatic. The structure of erythrocyte Human erythrocytes nuclear-cells that are shaped like concave discs 4,5-10,5 microns in diameter (average diameter of erythrocyte 7,55 m). With this form of erythrocyte, its surface is greater than it would be in spherical form. Scheme of hematopoiesis Mechanisms regulation of erythropoiesis Regulation of erythropoiesis carried out by neural and humoral mechanisms, sympathetic innervation stimulates hematopoiesis and parasympathetic - brakes. Of great importance is the regulation of erythropoiesis erythropoietin. Hematopoiesis is enhanced by hormones front of the pituitary gland, adrenal glands, thyroid gland. Male sex hormones stimulate, increasing the sensitivity of bone marrow to erythropoietin, and women - inhibit erythropoiesis. The body formed substances that inhibit erythropoiesis inhibitors of erythropoiesis. Their content increases with the number of red blood cells, which do not meet the needs of the tissues for oxygen. Inhibitors of erythropoiesis lengthen cycle division erythroid cells, they inhibit the synthesis of hemoglobin. Regulation and Requirements for Erythropoiesis Circulating erythrocytes – the number remains constant and reflects a balance between RBC production and destruction – Too few red blood cells leads to tissue hypoxia – Too many red blood cells causes undesirable blood viscosity Erythropoiesis is hormonally controlled and depends on adequate supplies of iron, amino acids, and B vitamins Regulation of erythropoiesis Respiratory pigments Hemoglobin Erythrocytes derive their colour from a complex protein called hemoglobin. This substance is composed of a pigment, heme, containing iron, and the protein glohin. Hemoglobin has the power to attract oxygen molecules and to hold them in a loose chemical combination known as oxyhemoglobin. It is said, therefore, to have a chemical affinity for oxygen. HEMOGLOBIN Respiratory pigments Myoglobin Hem is also part of the structure of myoglobin, an oxygen-binding pigment found in red (slow) muscles and in the respiratory enzyme cytochrome c. Porphyrins other than that found in hem play a role in the pathogenesis of a number of metabolic diseases (congenital and acquired porphyria, etc.) It may be the reserve pigments, which give the tissue oxygen in a small oxygen condition. MYOGLOBIN Methods for determination of hemoglobin To determine hemoglobin levels proposed many different methods: Gas metric method - measuring the amount of bound oxygen (1 g Hb can connect 1.36 ml of oxygen); Iron metric - measuring iron levels in the blood (iron content in Hb is 0.34%); Colorimetric - comparing the color of the solution to the color of the blood of the standard solution. Types of hemolysis of erythrocytes Osmotic Mechanical Thermal Biological Chemical Osmotic resistance of erythrocytes The minimum osmotic resistance of erythrocytes observed in fresh blood 0,50-0,45% NaCl, maximum - to 0,340,32% NaCl. The viscosity of the blood It is the friction that occurs between layers of fluid moving at different speeds. As in the bloodstream at different rates move blood cells and plasma, the viscosity just depends on them. Determine the figure using viscometer. Normally, blood viscosity is about 5 (as the viscosity of water is 1). Hematocrit Volume ratio of blood cells called plasma and hematocrit. Normally it is men 0,400,48 l / l (40-48%) in women - 0,36-0,42 l / l (36-42%). Erythrocyte sedimentation rate (ESR) Density or specific gravity of erythrocytes (1,098) is higher than plasma (1.027) and therefore in vitro with blood clot devoid of ability, they slowly settle to the bottom. Erythrocyte sedimentation rate in healthy male is 2-10 mm per hour, and a woman - 2-15 mm per hour. In newborns, it is only 1.2 mm per hour. Intensive physical work leads to decreased ESR. Pregnant sedimentation rate can reach 45 mm per hour.