MALE REPRODUCTIVE SYSTEM

MALE REPRODUCTIVE
SYSTEM
Objectives
At the end of the topic, the students should be able to :
Explain the functions of the testis
Discuss spermatogenesis
Describe the characteristics of a normal sperm
Explain the role of FSH and inhibin on spermatogenesis
Discuss the contents of semen and its abnormalities
Explain the functions of testosterone
Explain the control of secretion of testosterone
Main points in male reproductive physiology
Importance of Leydig cells and testosterone in puberty
Role of Sertoli cells,testosterone, DHT, and estrogen in spermatogenesis
How testosterone and inhibin functions in the adult feedback regulation of the Hypothalamic/ Pituitary/
Gonadal Axis
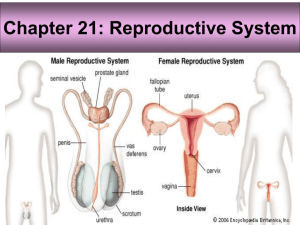
INTRODUCTION
A pair of testes
A pair of accessory glands
Ductal system
Copulatory organ
Male reproductive system
(Lateral view)
Male reproductive system
(Anterior view)
Structure of testis
Seminiferous tubules
FUNCTIONS
Production of spermatozoa after puberty for fertilization with the ovum from the female
Coitus process
Produce androgens
Testis
Originates from indifferent gonads during the embryonic phase
Contains lobules (200-300) separated by septum
Each lobule has 4 seminiferous tubules
Blood supply is from testicular artery and blood drainage is through the Pampiniform plexus into the testicular vein
Seminiferous epithelium contains Sertoli cells (Sustentacular cells) and Germ cells
Leydig cells exist in between tubules
Produce spermatozoa and androgens
Divided into two compartments; extratubular and intratubular
Histology of the testis
ITC
Leydig cells
SCN
ETC
Spermatogonia
Lumen
Compartments
Extratubular – vascular and interstitial divisions (inclusive of lymphatic channels and Leydig cells)
Intratubular – basal and adluminal divisions located in the seminiferous tubules
Spermatogenesis
Spermatogenesis and spermatozoon structure
Epididymis
Blood Testis Barrier
Formed before spermatogenesis commences
Formed by Sertoli cells
Functions :
1.
Stop intratubular spermatozoa from entering systemic and lymphatic circulation
The blood testes barrier is important since sperm (with their unique surface antigens) elicit an immune response if detected by the immune cells in the man’s blood, and the antibodies that are formed against sperm are designed to immobilize and destroy them
A number of events can disrupt the blood testes barrier and allow the immune system to become activated against the sperm.
•
•
•
•
•
These include: trauma to the testes torsion (twisting) of the testes a history of a vasectomy and reversal any other surgery within the scrotum infection within the testes
Allergic orchitis
Inflammation of the testis due to antisperm antibodies
2.
Ensure the intratubular chemical composition is different from the intertubular chemical composition (blood, interstitial fluid and lymph)
As spermatogenesis must occur in a controlled microenvironment, any changes in the chemical composition will affect normal spermatogenesis
Functions of Sertoli cells
Sertoli cells are joined by tight junctions that provides barrier to chemicals (Blood testis barrier)
Nourish developing sperm
Secrete luminal fluid including androgen binding proteins
(ABP)
Phagocytize defective sperm
Mediate testosterone and FSH effects on spermatogenesis
Secrete inhibin which inhibits FSH secretion
Influence Leydig cells via paracrine secretions
Embryonic secretion of Mullerian Inhibiting Substance
(MIS) that ensures male phenotype
Sertoli cells
Spermatogenesis
Process for formation of spermatozoa
The seminiferous tubules produce haploid cells (n)
Involves several steps including mitosis and meiosis
Takes about 64 days in human
1.
2.
3.
Consists of three stages:
Spermacytogenesis – formation of spermatid from spermatogonia
Spermiogenesis – formation from spermatid to spermatozoa
Spermiation – the release of spermatozoa into the epididymis
Spermacytogenesis
Mitosis stage spermatogonia type Ad give rise to a pair of spermatogonia type Ad or Ap spermatogonia type Ap give rise to a pair of spermatognia type Ap or B mitosis of the germ cells occurs in the basal compartment incomplete cytokenesis of committed cells (type Ap) results in the cells being linked by cytoplasmic bridges until spermatozoa is form this linkage results in a synchronous development of the cells within a given region of the tubule
-
-
-
-
Types of cells
germ cells - - spermatogonia (types A and B): spermatogonia type A - for spermatogenic lineage (type A dark (Ad) or A pale (Ap), type Ad are true stem cells) spermatogonia type B - progenitor cell for primary spermatocyte primary spermatocyte (46 chromosomes, 4N DNA): first meiotic division from these cells result in secondary spermatocyte (23 chromosomes, 2N DNA) second meiotic division from these cells results in spermatids spermatids (23 chromosomes, 1N DNA) – undergoes modifications in many parts and gives rise to spermatozoa spermatozoa, within the seminiferous tubules (and distally) the flagella is not motile
Spermiogenesis
-
-
spermatid phase: spermatids develop into spermatozoa in 4 stages:
Golgi phase
-
-
development of the acrosomal granule from the Golgi complex forming the acrosomal vesicle at the nascent apex (anterior) of cell positioning of centrioles at the nascent base of flagella initiation of formation of axonemal complex from one of the centrioles
Cap phase development of acrosomal cap over nucleus and condensation of chromatin development of flagellum from axonemal complex acrosome contains hydrolases (proteases, hyaluronidase, neuramidase, acid phosphatase) important in penetration of the oocyte membrane during fertilization
Spermiogenesis
-
-
-
-
-
Acrosome phase - spermatid re-orients so tail
(flagellum) projects into the lumen of the tubule and the acrosome towards the base of the epithelium further condensation of chromatin flattening and elongating of nucleus at the anterior of the cell movement of cytoplasm to the posterior of cell further development of flagellum linkage of flagellum to nucleus via the connecting piece developed from a centriole
Maturation phase - residual body of cytoplasm shed (cell linkages lost) and the cells released by Sertoli cell into lumen of tubule
Spermiation
released spermatid moved with fluid via peristaltic action of myoid cells transporting it to the straight tubule sperm cannot move yet will develop motility in epididymis
1 germ cell produces 64 spermatozoa
Process takes ~2 months (56 – 64 days ) to complete
100 million sperm produced each day
Not all are normal i.e., abnormal % increases with alcohol, heat, cigarettes, drugs
Temperature sensitivity…
Spermatogenesis is temperature sensitive, optimal
34 o C
Achieved by the descent of the testes out of the abdomen
Arteries and veins supplying the testes intertwine, efficiently exchanging heat (from artery to veins) to further cool testes
Scrotum
Originates from labioscrotal swellings and urethral fold
Pouch that houses the testes
Main function is to provide an environment which is 1-8 0 F lower than the body temperature and also to control testicular temperature
Testicular temperature needs to be controlled for spermatogenesis to occur normally
Control and regulation of testicular temperature (1)
-
Two muscle system – cremaster external and tunica dartos
Cremaster external muscle passes along inguinal canal and attaches to tunica vaginalis
Pulls tunica vaginalis as it contracts when the environmental temperature drops
Tunica dartos muscle attaches to scrotal skin and forms a septum separating the scrotum
- Pulls scrotal skin as it contracts when the environmental temperature drops
Control and Regulation of testicular temperature (2)
Pampiniform plexus
– consists of convoluted veins and arteries which follow the spermatid cord into the inguinal canal.
Arterial branch comes from spermatid artery and venous part enters the spermatid vein
- controls temperature by dissipating heat from the aortal blood through the convolutions before reaching the testis
-
-
-
-
The testes is located in the abdominal cavity during the fetal stage
Only descents into scrotum at 7 months of pregnancy
Sometimes do not descend and when born, two conditions may occur i.e., cryptochidism or monochidism
Crypotochidism – cryptochids are males with both testes in inguinal canal/abdominal cavity usually sterile may either be hereditary or due to lack of hormones undescended testes are associated with reduced fertility , increased risk of testicular cancer and psychological problems when the boy is grown undescended testes are also more susceptible to testicular torsion , infarction and inguinal hernias
Monochidism – monochids are males with only one testis descended into scrotum, the other remained in inguinal canal/abdominal cavity
- usually fertile as one testis still functioning normally therefore spermatogenesis is not impaired
Approximately 3% of full-term and 30% of premature infant boys are born with at least one undescended testis , making monochidism/cryptorchidism the most common birth defect of male genitalia
However, most testes descend by the first year of life (the majority within three months), making the true incidence of cryptorchidism around 1% overall.
Ductal System
Originates from Wolffian ducts (mesonephric kidney)
Mullerian ducts = rudiments in prostate gland (prostatic utricle/uterus masculinus) – non-functional but can grow when there is estrogen influence causing prostate cancer
Mesonephric tubules = vasa efferentia
Mesonephric ducts = epididymis, vas deferens and seminal vesicles
Urogenital sinus = prostatic, cavernous and membranous urethra, prostate glands and Bulbo-urethral gland (Cowper’s gland)
Rete testis in the testis = efferentia ducts and then becomes epididymis and vas deferens
Epididymis
Originates from mesonephric ducts
Divided into caput (head), corpus (body) and cauda (tail)
Extra fluid from sperm is reabsorbed to concentrate spermatozoa 100X
Presence of high concentrations of testosterone/ DHT in the tubule causes epididymis to secrete a motility- inducing protein that binds to the cell membrane of sperm cells
Secrete mucoproteins/glycoproteins that coats the head of the sperm
Also secretes carnitine, glycerolphosphorycholine, fructose and glycoproteins
Transit time for spermatozoa to attain maturation and the ability to move/motility is about 6 – 12 days
Spermatozoa can move forward and has the ability to fertilize ovum once has entered cauda epididymis
Morphological and biochemical changes also occur
Caput
Corpus
Cauda
Vas deferens
Developed from Wolffian ducts
Vas deferens have a lot of muscle layers (inner and outer longitudinal muscle layer with circular layers in between this muscles – layers are important for sperm motility
Vas deferens form the ampulla near the bladder
Sperm enters vas deferens from epididymis
Acts as a reservoir to store spermatozoa
Also acts as a conduit between testes and urethra
Mature sperm stored in the Vas Deferens and can remain viable for up to 3 months
If no ejaculation occurs, sperm will dribble into terminal ampulla into urethra
Copulatory organ - penis
-
-
-
-
-
Originates from genital tubercle
Provides an outlet for both urine and the copulatory ejaculate
(spermatozoa and seminal plasma)
Histology/anatomy of penis varies from species to species and from region to region within the same species
Body of the penis consists of: the urethra erectile tissue (corpora cavernosa penis and corpora cavernosum urethra), cavernous bodies act as erectile tissues where it can be engorged with blood to erect the penis touch and pressure receptors (Pacinian corpuscles) a dense connective tissue capsule (tunica albuginea tip of penis is called glans penis and in humans it is mushroomshaped
Penis
Accessory glands
A pair of seminal vesicles, prostate glands and bulbo-urethral glands (Cowper’s glands)
Originates from urogenital sinus and mesonephric ducts
Produces seminal plasma which is the fluid component of semen
-
-
-
-
-
-
-
-
-
-
seminal vesicle empties contents into ampulla tubuloalveolar gland yellowish secretory product and contains fructose, citrate, ascorbic acid, inositol, prostaglandins and proteins fructose is an important energy source for spermatozoa
70% of ejaculate (semen) derives from the seminal vesicles secretory activity stimulated by testosterone prostrate gland empties contents into the prostatic urethra prostrate is a branched tubuloalveolar gland secretions include acid phosphatase, amylase, and fibrinolysin gland wraps around prostatic urethra and empties into it glycoprotein deposits develop and can become calcified, these are called prostatic concretions or corpora amylacea and are a characteristic feature of the adult prostrate secretory activity stimulated by testosterone hyperplasia occurs within the gland with increasing age, gradually decreasing the diameter of the urethra and slowing urine voiding
-
-
bulbourethral (Cowper’s) gland empty into the postprostatic urethra tubuloalveolar glands that secrete a lubricating mucous that contains galactose, galactosamine, galacturonic acid, sialic acid, and methylpentose secretions precede other ejaculatory products and release involves the oxytocin axis secretory activity of epithelia stimulated by testosterone
Seminal plasma
Three functions:
1) as a media that provides the suspension/vehicle and also activation to spermatozoa
2) provides electrolytes, nitrogen, citric acid, fructose etc for nutrition
3) provides an alkaline pH to semen to combat acidity of vagina
Spermatozoa
A very simple cell but highly adapted for reaching and penetrating the ovum
Basically have head, midpiece and tail
Different sizes in different species
Head shape may be paddle (human, rabbit, bull, ram), cylindrical (cockerel) or hooked (rodent species)
Acrosome in the head contains hydrolytic enzymes for digesting cells around ovum; can also digests sperm upon death
Carries the necessary package for fertilization (enzymes and chromosomes)
Needs to travel light as main function is for fertilization
Tail contains mitochondria that provides ATP for energy for increased motility to reach ovum before sperm dies
Tail have 9 + 2 doublets arrangement called axoneme
Has no energy reserves, hence has a limited life span once released (48 – 72 hrs)
Dies by degeneration (hydrolytic enzymes in acrosome destroy sperm upon death)
Spermatozoa
Rat sperm Rabbit sperm
Human sperm Chicken sperm
Sperm motility
Semen
Ejaculate - spermatozoa and seminal plasma
By volume <10 % sperm
Accessory Glands: 60 % seminal vesicle,
10 % bulbourethral, 30 % prostate
Usually ph 7 to 7.4
Coagulate after ejaculation in human
Coagulation is important so that sperm number that enters vagina is maintained
Liquefaction of semen occurs usually before 30 mins
Liquefaction is due to enzyme-substrate interaction
The liquefaction time denotes semen quality: the longer the liquefaction time, the lower is the quality. WHY? As the life span of sperm is only about 72 hours, the sperm will need to break free from the gel ASAP to enable it to swim up to meet the ovum
Normal semen values
(WHO,1999)
Volume 2 – 3 ml
Liquefaction time ideally 30 mins)
Colour
Viscosity
Milky
Fairly watery pH
Motility
7 – 7.2
50 – 60%
Count > 20 million/ml
Viability > 50%
Normal morphology variable 30%
Terms
Normospermia/normozoospermia (normal semen values)
Azoospermia – no sperm found in sample
Oligospermia – less than 20 million/ml sperm
Asthenozoospermia – sperm present but non-motile
Necrozoospermia – high number of dead sperm
Teratozoospermia – high number of abnormal sperm
Regulation of spermatogenesis
Prepubertal LH and FSH are low, thus testes activity is low
Between the ages of 13 and 20 the hypothalamic/ pituitary/ gonadal axis is reactivated (puberty)]
The precise trigger is not known…
– could be percentage body adipose tissue
– could be pineal gland/ melatonin involvement
Regulation of testicular function
GnRH released every 2- 3 hours
Results in a pulsatile release of LH and FSH
Testosterone from Leydig cells inhibits both the release of LH and GnRH
Inhibin from Sertoli cells inhibits the release of
FSH (but not LH or GnRH).
Hormonal influence
GnRH from hypothalamus goes to anterior pituitary – FSH and LH are released
LH (Interstitial Cell Stimulating Hormone/ICSH) goes to Leydig cells to initiate production of testosterone
FSH and testosterone stimulates Sertoli cell (Sustentacular cells) to increase enzyme activity (5
-reductase, aromatase) and synthesis Androgen Binding
Proteins (ABP)
ADP will bind to testosterone causing level of testosterone in lumen of seminiferous tubules to rise
Sustentacular cells also produce inhibin (a peptide hormone)
FSH and LH only acts on testis but testosterone influences testis and initiate development of sexual organs and male secondary sexual characteristics
Control of testosterone secretion
When testosterone and inhibin levels in the blood are high, two negative feedback mechanisms are initiated to regulate the spermatogenic process
When levels of circulating testosterone are high in the blood, this high testosterone will send a negative feedback mechanism to hypothalamus to inhibit LH release
Control of sperm production
When there are >20 million spermatozoa in the testicles, inhibin will send a negative feedback mechanism to the hypothalamus to inhibit the release of FSH
This two negative feedback mechanisms are terminated when level of testicular spermatozoa falls below 20 million and testosterone level falls below required level for normal spermatogenesis
Functions of testosterone
-
-
-
-
Produced by the Interstitial cells of Leydig under influence of LH and GnRH
Testosterone has a number of functions
Promotes maturation of sperm cells
Maintains male 2nd sex organs
Determines secondary male characteristics ( wide shoulders, narrow hips, body hair patterns, enlargement of thyroid cart of larynx, deepens voice)
Stimulates bone and muscle growth, epiphysial closure, protein metabolism