What is Emphysema? The accepted definition of emphysema is a

EMPHYSEMA
A permanent, abnormal enlargement of gasexchange airways, with destruction of alveolar walls, without fibrosis (2).
SYDONIE STOCK
NCLEX Questions
(6)
All of the following nursing diagnoses are important for a client with chronic pulmonary emphysema (COPD). Which would receive priority when planning nursing interventions?
A. Self-care deficit
B. Activity intolerance
C. Ineffective airway clearance
D. Impaired gas exchange
Answer: D
Which of the following interventions would be a priority in the plan of care for the person with pulmonary emphysema?
¹
A. Intravenous ampicillin therapy
B. Maintaining hydration status
C. Low-flow oxygen via face mask
D. Intravenous aminophylline
Answer: C
RESOURCES
(1) Chronic obstructive pulmonary disease among adults - United States, 2011. (2012). MMWR:
Morbidity & Mortality Weekly Report , 61 938-943.
(2) Huether, Sue & McCance, Kathryn. (2012).
Understanding Pathophysiology (5 th ed) p.693-4.
St. Louis, MO: Elsevier Mosby Inc.
(3) Ladwig, Gail & Ackley, Betty. (2011). Mosby’s guide to nursing diagnosis (3 rd
ed). Maryland
Heights, MO: Mosby Inc.
(4) Lynn, Pamela. (2011). Clinical nursing skills: A nursing process approach (3 rd ed). Philadelphia,
PA: Lippincott, Williams & Wilkins.
(5) Mitzner, W. (2011). Emphysema--a disease of small airways or lung parenchyma? New England
Journal of Medicine , 365 (17), 1637-1639.
(6)Tabloski, Patricia. (1995). NCLEX Review
Questions .
Gerontological Nursing . Chapter 16.
Pearson.
All pictures were found in Google Images. Emphysema patient .
What is Emphysema?
The accepted definition of emphysema is a permanent, abnormal enlargement of acini with destruction of alveolar walls without fibrosis (2).
Etiology There could be two different ways emphysema forms. One way is the commonly accepted explanation: inflammation of the alveoli leads to the destruction of the alveolar walls and the elastic fibers that connect the acini to the terminal bronchiole, which causes airway enlargement and narrowing of the small airway at the bronchiole opening. The other explanation could be that the small airway is narrowed and obstructed by inflammation. The resulting increased pressure in the acini would cause folding and breaking of the alveolar walls and destruction of the elastic fibers (5).
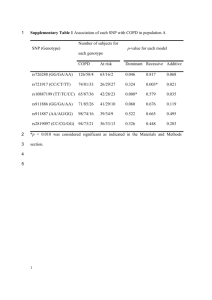
Incidence COPD, the category of pulmonary disorders that emphysema falls under, became the third leading cause of death in 2008. According to a randomized national telephone survey, whose participation average was 74.2%, approximately 15 million people have been diagnosed with COPD by their physician. More than 11.6% of this population was 65 years or older (1).
Risk Factors There are two categories of emphysema: primary and secondary. Primary emphysema is associated with “an inherited deficiency of the enzyme α1-antitrypsin …[which] inhibits the action of many proteolytic enzymes.”
Without this enzyme, there is a greater chance the patient will develop emphysema due to proteolysis in the lung tissue (2). Secondary emphysema is caused by inhalation of cigarette smoke. Other contributing factors are “air pollution, occupational exposure, and childhood respiratory tract infection s” (2).
Pathophysiology With the inhalation of tobacco smoke or chemicals, antiproteases are inhibited while inflammation and protease activity are stimulated. This stimulation promotes alveolar destruction by cellular apoptosis and senescence.
The alveolar destruction produces bullae, large air spaces in the lung parenchyma, and blebs, air spaces by the pleurae. The bullae and blebs do not promote gas exchange and the result is an alteration to the ventilation-perfusion ratio, leading to hypoxemia. The barrel chest appearance is caused by air trapped within the lung, resulting in hyperexpansion of the chest. This stretches the muscles used during respiration and more effort is required during breathing (2).
WHAT IS EMPHYSEMA?
BULLAE
PINK PUFFER CAUSE & EFFECT
DIFFERENCES SHOWN
Lifespan and Cultural Considerations
Emphysema typically affects the older generation. In the survey mentioned previously, 3.2% of those diagnosed with COPD were between the ages of 18 and 44 while more than 11.6% were 65 years or more. The subjects could have been diagnosed with
“COPD, emphysema, or chronic bronchitis” (1). If the younger generation was in fact diagnosed with emphysema, it was most likely primary emphysema
(2).
Culturally, those diagnosed with emphysema would have a history of inhaled tobacco use, additionally they could have had exposure to inhaled chemicals either in their place of employment or simply have lived in a highly polluted area (2).
CLINICAL MANIFESTATIONS
The classic sign of emphysema is the “barrel chest” and a prolonged expiration is always present. The common manifestations are dyspnea and wheezing. Most likely, the patient has a history of smoking. Late in the course of the disease, the patient may present with chronic hypoventilation, polycythemia, or cor pulmonale.
If there is an infection with the emphysema, the patient could have a productive cough as well (2).
COMPLICATIONS
Complications that could be associated with emphysema are related to the increased effort it takes to breathe and to chronic inflammation of the airways. Because there is greater resistance against the respiratory muscles, respiratory fatigue could develop after a while. This fatigue may lead to hypoventilation and hypercapnia.
Inflammation could result in bronchi hyperreactivity and bronchioconstriction, making breathing even more difficult. Chronic inflammation could also have systemic affects.
“Weight loss, muscle weakness, and increased susceptibility to comorbidities, such as infection” could all be caused by chronic inflammation of the airways (2).
NURSING DIAGNOSES
Impaired gas exchange related to ventilationperfusion inequality (3).
The client will verbalize understanding of oxygen supplementation and other therapeutic interventions by day two (3).
Noncompliance related to reluctance to accept responsibility for changing detrimental health practices (3).
The client will review emphysema literature and verbally admit responsibility for the current health state by day five.
Imbalanced nutrition: less than body requirements related to decreased intake because of dyspnea (3).
The client will consume adequate nourishment during at least five meals in one week (3).
SIGNIFICANCE TO NURSING
Emphysema has a significant impact on nursing and respiratory therapists. When treating an emphysema patient, the nurse needs to remember the fragile state the patient’s lungs are in. With any COPD patient, the nurse has to take care not to force too much oxygen into the lungs because this could rupture the already damaged alveoli. The highest level should be no greater than 3 L/min (4). Also, with the advancing age of the “baby boomer” generation, there could be an increase in patients diagnosed with emphysema.
I know a 79 year old male who was diagnosed with emphysema within the last year.