Respiratory:
Respiratory Failure and ARDS
Marnie Quick, RN, MSN, CNRN
Respiratory Failure- outline
Resp volume/capacity and definition Resp failure
Causes/predisposing factors
Classification
Hypoxemic (causes/mechanisms/s&s)
Hypercapic (causes/s&s)
Dx tests
Rx
RT/artifical airways/mechanical
vent/drugs/medical/nutrition
Nursing (assessment/Nursing Dx- Plan)
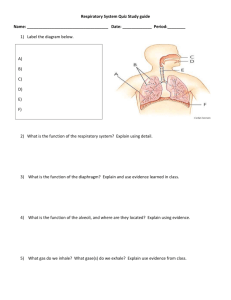
Normal Respirations: Tidal Vol; Inspiratory &
Expiratory reserve Vol; Residual Vol; Vital
Capacity; Anatomical dead space; Blood
Resp Failure:one or both exchanging systems
is inadequate (air to lung or lung to blood)
Blood Supply to Lung
Respiratory Failure
Not a disease process, sign of severe dysfunction
Predisposing Factors (Lewis 1746 Table 68-2)
Airways/alveoli
CNS
Chest wall
Neuromuscular
Commonly defined in terms of ABG’s:
PO2 of less than 60 mmHg
PCO2 greater than 45 mmHg
Arterial pH of less than 7.35
Classification of Respiratory Failure
Hypoxemic Respiratory Failure
Oxygenation failure- inadequate O2 transfer
between alveoli & pulmonary capillary bed
PaO2: 60 mm Hg or less on 60 % O2
Inadequate O2 saturation of hemoglobin
Causes tissue hypoxia> Metabolic acidosis; cell
death; decreased CO; impaired renal function
Common causes: disorders that interfere with O2
transfer into the blood- respiratory or cardiac
system (Lewis p. 1800 Table 68-1)
Hypoxemic Respiratory Failure
Mechanisms that may lead to Hypoxemia:
1. Mismatch ventilation & perfusion (V/Q mismatch)
V/Q: Volume blood perfusing lungs each minute
Each ml of air for each ml of blood
1:1= V/Q ratio of 1
Causes of V/Q mismatch:
Ventilation portion blocked (secretions in
airway/alveoli, airway/alveolar collapse, decreased
movement chest/ventilation)
Perfusion portion blocked (pulmonary embolus)
Hypoxemic Respiratory Failure
Range of ventilation to perfusion (V/Q relationship)
A. Absolute shunt, no
ventilation fluid in alveoli
B. Ventilation partially
compromised- secretions
C. Normal lung unit
D. Perfusion partially
compromised by emboli
obstructing blood flow
E. Dead space: no
perfusion- obstruction of
pulmonary capillary
Hypoxemic Respiratory Failure
Mechanisms that may lead to Hypoxemia:
2. Shunt- Extreme V/Q mismatch
Occurs when blood
leaves heart without gas
exchange
Types:
1. anatomic shunt: O2
blood does not pass
through lungs
2. intrapulmonary shuntalveoli fill with fluid
Treatment: Mechanical
ventilation to force O2
into lungs; treat cause
Hypoxemic Respiratory Failure
Mechanisms may lead to Hypoxemia:
3. Diffusion limitations
Alveoli membrane
thickened or destroyed
Gas exchange across
alveolar-capillary
membrane can’t occur
Classic sign: hypoxemia
present during exercise,
not at rest
Treat the cause such as
pulmonary fibrosis;
ARDS
Hypoxemic Respiratory Failure
Mechanisms may lead to Hypoxemia:
Clinical manifestations of hypoxemia
Specific: Respiratory:
Nonspecific: Cerebral, cardiac, other
Treatment: treat cause, O2 and mechanical
ventilation
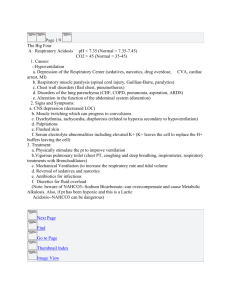
Hypercapic Respiratory Failure
Ventatory failure: Inability of the respiratory system to
ventilate out sufficient CO2 to maintain normal PaCO2
PaCO2 greater than 45 mm Hg, Arterial pH less than 7.35
PCO2 rises rapidly and respiratory acidosis develops,
PO2 drops more slowly
Common causes include disorders that compromise lung
ventilation and CO2 removal- Lewis Table 68-1
(airways/alveoli, CNS, chest wall, neuromuscular)
Clinical manifestations: specific respiratory, nonspecific
of cerebral, cardiac, neuromuscular
Treatment: adeq O2, airway, meds, treat underlying cause,
nutrition
Collaborative Care for Respiratory Failure:
Diagnostic tests
History/physical assessment
Pulse oximetry
ABG analysis
Chest X-ray
CBC, sputum/blood cultures, electrolytes
EKG
Urinalysis
V/Q scan- if pulmonary embolism suspected
Hemodynamic monitor/pulmonary function tests
Collaborative care for Respiratory Failure
Respiratory Therapy
Main treatment- correct underlying cause & restore
adequate gas exchange in lung
Oxygen Therapy (Maintain PaO2 at least 60 mm Hg,
SaO2 90%)
Mobilization of secretions
Effective coughing & positioning
Hydration & humidification
Chest physical therapy
Airway suctioning
Positive pressure ventilation
Noninvasive positive pressure ventilation
Intubation with mechanical ventilation
Collaborative Care for
Respiratory Failure cont
Drug Therapy
Medical supportive therapy
Relief bronchospasm; reduce airway inflam and
pulmonary congestion; treat pulmonary infections;
reduce anxiety, pain
Treat underlying cause
Nutritional therapy
Enteral; parenteral
Protein and energy stores
Collaborative Care: Artifical airwaystracheostomy and endotracheal tubes
Endotracheal tube
Taping and inline suctioning of an
endotracheal tube
Exhaled C02 (ETC02) normal 35-45
Used when trying to wean
patient from a ventilator
Complications of endotracheal intubation
1. Extubation
Restraints
2. Aspiration
Tube at right allows
for subglottal
suctioning
Independent Lung Ventilation
Collaborative Care:
Mechanical Ventilation
Provide adeq gas
exchange
Criteria to put on vent
RR > 35-45
pCO2 >45
pO2 <50
Types- Positive, Neg
Settings- Table 66-10
Modes- Table 66-12
Types: Negative pressure ventilator
Types: Positive pressure mechanical
ventilation with endotracheal tube (PPV) on
left and noninvasive mask on right (CPAP)
Ventilator settings of Modes of PPV
(Table 66-12 p.1706)
Volume Modes
AC; SIMV
Pressure Modes
PSV; PC-IRV
Predetermined tidal volume (TV) is delivered with each
inspiration
Tidal volume (TV) is consistent, airway pressures will vary
Predetermined peak inspiratory pressure
Tidal volume (TV) will vary, airway pressures will be
consistent
Other Modes
PEEP and CPAP
Ventilator settings:
SIMV
PEEP
Alarm settings
Assess your patient – not
the alarm!!!!!
Never turn alarms off
Alarms sound when you
have low pressure or high
pressure in the ventilator
Note “alarm silence” and
“alarm reset” on picture
to the right
Lewis 1705 Table 66-11
Low Pressure
•Circuit leaks
•Airway leaks
•Chest tube leaks
•Patient disconnect
from vent or tube
High Pressure
•Patient coughing
•Secretions or mucus in
the airway
•Patient biting tube
•Airway problems
•Reduced lung
compliance (as a
pneumothorax)
•Patient fighting the
ventilator
•Accumulation of water
in the tube
•Kinking of tube
Complications/Nursing Care of
Positive Pressure Mechanical ventilation
Cardiovascular: decreased CO; inc intrathoracic pressure
Pulmonary: Barotrauma; Volutrauma; alveolar
hypoventilation/hyperventilation; ventilator-associated
pneumonia
Sodium and water imbalance
Neurological: impaired cerebral bl flow>IICP
Gastrointestional: stress ulcer/GI bleed; gas; constipation
Musculoskeletal: dec muscle tone; contractures; footdrop;
pressure ulcers from BR
Psychosocial: physical & emotional stress; fight vent
Other problems
when on mechanical ventilation
Machine disconnection or malfunction
Nutrition needs
Weaning from ventilator/ extubation
Spontanenous breathing trial (SBT) Hospital
protocol
Document progress
Table 66-13 p.1712- readiness/assessment
Nursing assessment specific to
Respiratory Failure
Assess both airway and
lungs- note picture to
right
Refer to hypoxic and
hypercapnic respiratory
failure symptoms
Table 68-4 p. 1751
Subjective data
Objective data
Relevant Nursing Problems related to
Respiratory Failure
Prevention of acute respiratory failure
Nursing Care Plans
Gerontology considerations
Nursing Care Plans Mechanical ventilation
Suctioning procedure and oral care
(p.1701-8)
ADRS- outline
Normal patho/Definition
Causes/predisposing factors
Phases/patho
Clinical progression/s&s/chest X-ray
Complications
Rx
Injury/exudate
Reparative/poliferation
Fibrotic
RT-vent & proning-CLRT
Medical support- monitor CO/tissue perfusion & nutrition/fluids
Nursing (assessment/Nursing Dx-Plan)
Acute Respiratory Distress Syndrome
ARDS
Sudden progressive form of
acute respiratory failure
Follows various pulmonary or
systemic conditions
Alveolar capillary membrane
becomes damaged & more
permeable to intravascular
fluid
Results in noncardiac
pulmonary edema and
progressive refractory
hypoxemia
ARDS is NOT primary!
Most common cause- Sepsis
Stages of Edema Formation in
ARDS
A, Normal alveolus and
pulmonary capillary
B, Interstitial edema
occurs with increased
flow of fluid into the
interstitial space
C, Alveolar edema
occurs when the fluid
crosses the blood-gas
barrier
Fig. 68-8
Copyright © 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.
Pathophysiology of ARDS
Surfactant keeping alveoli open
Fibrotic lung
Clinical progression of ARDS
Insidious onset- sym dev 24-48 hrs post
initial insult (direct or indirect lung injury)
Course determined by nature of initial
injury, extent & severity of coexisting
disease, and pulmonary complications
50% who develop ARDS die- even with
aggressive treatment
Clinical manifestations of ARDS
Progressive refractory hypoxemia> Hallmark sign
Noncardiac pulmonary edema
Early symptoms- labored R- dyspnea, tachypnea,
anxiety/restless, dry-nonproductive cough
Later symptoms- cyanosis, adventitious breath
sounds, use of accessory muscles with retractions
and decreased mental status
Diagnosis of ARDS
ABG’s> refractory
hypoxemia
Chest X-ray infiltrates>
white out/snow storm.
Note progression picture
to right
Pulmonary artery wedge
18 mm Hg & no
evidence of heart failure
Identification of a
predisposing condition
for ARDS within 48 hrs
of clinical manifestations
Complications of ARDS
Hospital-acquired pneumonia
Barotrauma
Volu-pressure trauma
Physiologic stress ulcer
Renal failure
Collaborative Care for ARDS
Respiratory therapy & medical support
Oxygen
Mechanical ventilationmain treatment
Positioning strategies
Proning
CLRT-lateral rotation
bed
Maintenance of CO &
tissue perfusion (fluids)
Maintenance of nutrition
& fluid balance
Treat underlying cause
Rotoprone bed
Benefits to Proning >
Nursing assessment specific to ARDS &
Relevant nursing problems R/T ARDS
Assessment
Refer to respiratory failure assessment
Assess for clinical progression and clinical
manifestations as stated above
Nursing care plans- refer to resp failure
Goals for recovery from ARDS
PaO2 within normal limits on room air
SaO2 greater 90%
Patent airway
Lungs clear on auscultation