2012-infections-of-the-cardiovascular-system
advertisement

Author(s): N. Cary Engleberg
License: Unless otherwise noted, this material is made available under the
terms of the Creative Commons Attribution-ShareAlike 3.0 License:
http://creativecommons.org/licenses/by-sa/3.0/
We have reviewed this material in accordance with U.S. Copyright Law and have tried to maximize your
ability to use, share, and adapt it. The citation key on the following slide provides information about how you
may share and adapt this material.
Copyright holders of content included in this material should contact open.michigan@umich.edu with any
questions, corrections, or clarification regarding the use of content.
For more information about how to cite these materials visit http://open.umich.edu/education/about/terms-of-use.
Any medical information in this material is intended to inform and educate and is not a tool for self-diagnosis
or a replacement for medical evaluation, advice, diagnosis or treatment by a healthcare professional. Please
speak to your physician if you have questions about your medical condition.
Viewer discretion is advised: Some medical content is graphic and may not be suitable for all viewers.
Attribution Key
for more information see: http://open.umich.edu/wiki/AttributionPolicy
Use + Share + Adapt
{ Content the copyright holder, author, or law permits you to use, share and adapt. }
Public Domain – Government: Works that are produced by the U.S. Government. (17 USC § 105)
Public Domain – Expired: Works that are no longer protected due to an expired copyright term.
Public Domain – Self Dedicated: Works that a copyright holder has dedicated to the public domain.
Creative Commons – Zero Waiver
Creative Commons – Attribution License
Creative Commons – Attribution Share Alike License
Creative Commons – Attribution Noncommercial License
Creative Commons – Attribution Noncommercial Share Alike License
GNU – Free Documentation License
Make Your Own Assessment
{ Content Open.Michigan believes can be used, shared, and adapted because it is ineligible for copyright. }
Public Domain – Ineligible: Works that are ineligible for copyright protection in the U.S. (17 USC § 102(b)) *laws in
your jurisdiction may differ
{ Content Open.Michigan has used under a Fair Use determination. }
Fair Use: Use of works that is determined to be Fair consistent with the U.S. Copyright Act. (17 USC § 107) *laws in your
jurisdiction may differ
Our determination DOES NOT mean that all uses of this 3rd-party content are Fair Uses and we DO NOT guarantee that
your use of the content is Fair.
To use this content you should do your own independent analysis to determine whether or not your use will be Fair.
Infections of the
Cardiovascular System
Prepared by
N. Cary Engleberg. M.D.
Professor of Internal Medicine,
Division of Infectious Diseases,
University of Michigan Medical School
This presentation may be used and remixed under the conditions of a
Creative Commones Attribution-ShareAlike 3.0 Unported license (CC BY-SA 3.0)
Cardiovascular infections: Outline
• Viral infections
– acute myocarditis
– acute pericarditis
• Bacterial and fungal infections
– endocarditis
– other intravascular infections
• mycotic aneurysm and aortitis
• septic thrombophlebitis
• indwelling device infections
– tuberculous pericarditis
– spirochetal diseases (syphilis, Lyme disease)
• Parasitic infections
– American trypanosomiasis
• Possible infectious etiology
– endomyocardial fibrosis (EMF)
Acute dypsnea in a young man
• History: A 35 year old previously healthy man complains of
increasing dyspnea with exertion and fatigue over the past week.
Current symptoms were preceded by an episode of fever, myalgia,
and mild diarrhea that began 1-2 weeks ago but resolved in 2 days.
• P.E.:
– Afebrile. HR=105/min with occasional skipped beats at rest.
BP=110/70mmHg, RR= 22/min
– Chest: bibasilar crackles.
– Heart: non-displaced PMI. A soft S3 heard at the apex. No
murmurs or rubs. There is 1+ ankle edema.
• Chest x-ray: Normal heart shadow. Cephalization of pulmonary
vasculature consistent with mild pulmonary edema.
• EKG: non-specific T-wave changes; occ. ventricular ectopic beats
• Lab: troponin I level mildly elevated
Acute dyspnea (continued)
• The patient was treated for mild heart failure with
gentle diuresis with furosemide, an ACE inhibitor, and
a beta-blocker. This treatment improved his dypnea.
• After one week of treatment, the patient felt much
better, tachycardia resolved, and diuresis was no
longer necessary. Gradually, the other medications
were withdrawn, and he resumed normal activity
without symptoms.
Myocarditis
• Most often associated with viral infection in the heart
and infiltration of cardiac muscle by T-lymphocytes
• Symptoms are variable:
–
–
–
–
–
prodromal viral illness present in some cases
various degrees of CHF
chest pain
arrhythmias, heart block
sudden death
• Treatment: as for heart failure; avoid NSAIDs
• Prognosis:
– early resolution of sxs (<2 weeks) --> complete recovery
– prolonged symptoms (>2 weeks-months)--> dilated
cardiomyopathy, worsening heart failure, death (or cardiac
transplantation)
(from Cooper LT. New Engl J Med 2009;360:1526-38)
Viruses associated with
acute myocarditis
• Most common:
– enteroviruses (particularly coxsackie B)
• Others
– adenoviruses
– herpesviruses
• CMV
• EBV
• HHV-6
– parvovirus B19
– HIV
– influenza
(Note: acute or chronic
myocarditis can also be noninfectious, e.g., allergic, toxic,
or autoimmune in origin)
Chest pain in a young man
• History: A 26 year old man developed fever, malaise, and
intense, sharp mid-sternal pain that is worse when he lies flat on
his back, bends forward, or coughs. He has been ill for 4-5 days.
• PE:
–
–
–
–
–
Temp= 38.2C, HR=96/min, RR=20/min, BP=120/80 mmHg
Neck: no JV distention
Chest: clear
Heart: a 3-component friction rub is heard at the lower LSB
Extremities: no edema
• Chest x-ray: normal cardiac silhouette
• Lab: CBC and chemistries normal; troponin and CPK-MB: both
normal. Sedimentation rate elevated at 55 mm/hr.
• EKG: (see next slide)
Acute pericarditis: causes
• Infections
– enteroviruses (coxsackievirus, echovirus)
– HIV
– bacteria (S. pneumoniae, S. aureus); note that the
patient with bacterial pericarditis is much more ill,
with shaking chills and high fever
– tuberculosis
– rheumatic fever (rare)
• Non-infectious
– post-MI, post-pericardiotomy, trauma, uremia,
myxedema, radiation therapy, lupus, drugs
(procainamide, hydralazine), neoplasm
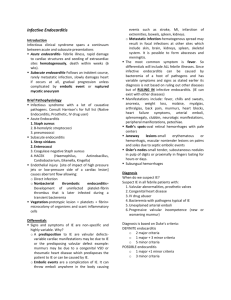
Acute infectious pericarditis
• Treatment:
– Antiinflammatory drugs (NSAIDs, steroids) for suspected
viral pericarditis.
– Monitor for development of pericardial effusion or
tamponade.
– Bacterial infection requires specific antibiotic therapy and
usually requires drainage of pericardial fluid.
• Prognosis:
– Viral pericarditis usually resolves spontaneously.
– Bacterial pericarditis can be severe and result in death if not
promptly treated.
Fever and night sweats
• History:
– A 56 year old woman was admitted to the hospital
after developing an acute onset of left hand
weakness. She gave a history of increasing
fatigue, weight loss, fever, and night sweats during
the preceding 3 months.
– The past history revealed that the patient had a
prolonged febrile illness as a child that involved
multiple painful, swollen joints and dyspnea on
exertion. The illness resolved spontaneously after
about 6 weeks.
Fever and night sweats (continued)
• Physical Examination:
–
–
–
–
Temp=38.6, HR=110/min, BP=150/60mmHg, RR=28/min
HEENT: multiple carious and broken teeth
Chest: dependent wet rales up to the mid-scapula bilaterally
Heart: Gr II/VI blowing diastolic murmur at the left sternal border, 3rd
intercostal space
– Abdomen: moderate splenomegaly
– Extremities: purplish, tender nodules on the pulps of three fingers;
petechiae over the pre-tibial areas bilaterally; 1+ ankle edema
• Lab results:
–
–
–
–
WBC=8,800/mm3, Hb=7.9 gm/dL, sed rate=78 mm/hr
Creatinine=2.3; BUN=40
Urine: 2+ protein, 5-10 WBCs/hpf, 50-100 RBCs/hpf
Blood cultures: 3 of 3 bottles positive for alpha-hemolytic
streptococci.
Questions for discussion
1.
2.
3.
4.
5.
What is the diagnosis?
What part of the heart is involved?
Why did this area become infected?
What was the childhood illness?
What was the original source of the
infecting bacteria?
6. Why does the patient have a weak left
hand?
7. What caused the abnormal creatinine and
BUN? The blood in the urine?
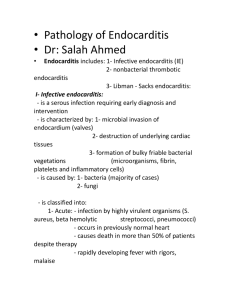
Steps in the pathogenesis of
infective endocarditis
• Pre-existing turbulence in the bloodstream (usually a
aournd a damaged heart valve)
• Minor fibrin and platelet deposition occurs on the low
pressure side of the valve (i.e., non-bacterial
thrombotic endocarditis, or NBTE)
• Bacteremia (transient and common)
– from the mouth = viridans (alpha) streptococci
– from the skin = Staphylococcus aureus
– from the urinary tract = Enterococcus spp.
• Seeding and adherence of the bacteria to the valve
leads to more fibrin and platelet deposition until a
large, potentially destructive vegetation develops on
the valve. (NBTE + bacteria= infective endocarditis)
Vegetations on the mitral valve
CDC/Dr. Edwin P. Ewing, Jr., 1972
Vegetation as seen by
echocardiography in a live patient
Histopathology of a valvular
vegetation
Blue areas
are bacterial
colonies
Pink areas are
composed of fibrin
and platelets
© 1994-2012 by Edward C. Klatt MD, Savannah, Georgia, USA.
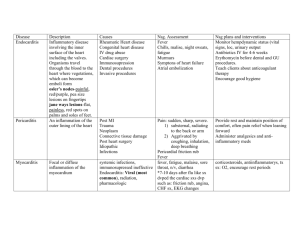
Clinical features of endocarditis
• Subacute endocarditis (due to alpha-streptococci
and other relatively non-virulent bacteria) - symptoms
develop slowly over months
– Symptoms:
•
•
•
•
Fatigue, malaise
Fever, chills, drenching night sweats
Anorexia, weight loss
Back pain
– Signs:
• New or changing heart murmur
• Peripheral manifestations: petechiae, splinter hemorrhages or
fingernals or toenails, Osler’s nodes, Roth spots (in the retina)
• Splenomegaly
• Anemia (pallor)
Clinical features of endocarditis
• Acute endocarditis (due to S. aureus) - symptoms
develop slowly over days to a few weeks
– Symptoms:
• Intense fever, shaking chills
• Exhaustion and prostration
– Signs:
• New or changing heart murmur
• Signs of sepsis syndrome or septic shock (may be rapidly
progressive or fulminant)
• Peripheral manifestations: splinter hemorrhages, peripheral
embolic phenomema, e.g., Janeway lesions, infarctions of toes
or fingers
Peripheral manifestations of
endocarditis
Osler’s
nodes
Splinter
hemorrhages
Janeway
lesions
Conjunctival
petechiae
Mylonakis E and Calderwood S. N Engl J Med 2001;345:1318-1330
Roth’s spots
Varga Z and Pavlu J. N Engl J Med 2005;353:1041
Microbial causes of endocarditis
• Common:
–
–
–
–
–
viridans (alpha) streptococci
enterococci
S. aureus
Other streptococci
coagulase-negative staphylococci (usually restricted
to prosthetic valves or internal devices)
• Less common or rare:
– HACEK group - (Haemophilus, Actinobacillus,
Cardiobacterium, Eikenella, Kingella)
– Gram-negative (e.g., Pseudomonas)
– fungi (e.g., Candida spp.)
– Coxiella burnetii
Complications of Endocarditis:
Cardiac Consequences
• Congestive heart failure due to valvular
destruction and incompetency
• Perivalvular abscess
• Infection of the conduction with arrhythmias
and/or heart block
• Acute myocardial infarction (due to coronary
embolization)
• Pericarditis->hemopericardium->tamponade
• Cardiac fistulas due to erosion from one area
of the heart to another
Paravalvular abscess with regurgitation in a patient
with rheumatic disease who presented with fever.
Didier D et al. Radiographics 2000;20:1279-1299
©2000 by Radiological Society of North America
Complications of Endocarditis:
Embolic Consequences
• Infarction of any organ
• Splenic infarction +/- abscess can
cause prolonged unremittent fever and
pain radiating to the left shoulder
• Pulmonary septic emboli from rightsided vegetations
Pulmonary septic emboli on a chest x-ray (left) and
chest CT (right) originating from tricuspid endocarditis
Septic emboli have cavitated and now show
air-fluid levels within the cavities that
communicate with the pulmonary airways.
Chen J and Li Y. N Engl J Med 2006;355:e27
Complications of Endocarditis:
Neurological Consequences
• Neurologic complications in 20-40% at
presentation (less common after
antibiotics)
• New stroke with fever (think
“endocarditis”)
• Complications include:
– mycotic aneurysms
– meningitis
– intracranial hemorrhage
Mycotic
aneurysms
Intracerebral hemorrhage
Mycotic aneurysms occur when bacteria
invade blood vessel walls via the vasa
vasorum. They infect and weaken the
walls allowing an aneurysm to form, and
eventually rupture with hemorrhage in
the area of the aneurysm, and with
greatest consequence in the brain.
Diagnosis of endocarditis:
Duke criteria
• Major criteria:
– Two, separate, positive blood cultures with typical organisms
– Evidence of a compatible cardiac lesion
•
•
•
•
new murmur
vegetation by echocardiogram
myocardial abscess
detachment (dehiscence) of a prosthetic valve.
• Minor criteria:
– Intravenous drug abuse
– Fever of 38.0 or greater
– A compatible vascular phenomenon (e.g., Janeway lesion, splinter
hemorrhages, stroke, splenic infarct)
– A compatible immunologic phenomenon (Osler’s node, Roth spot,
glomerulonephritis, positive rheumatoid factor)
– Positive blood cultures not meeting major criteria (one culture, etc...)
– Minor echo finding (e.g., valve thickening without definite vegetation)
Diagnosis of endocarditis:
Duke criteria
• The diagnosis is made with:
– 2 major criteria
– 1 major and 3 minor criteria, OR
– 5 minor criteria
Treatment of endocarditis:
Principles
• Therapy must be microbicidal, not
static.
• Antibiotics should be given in maximal
doses, usually intravenously
• . . . and given for a long time (several
weeks)
Treatment of endocarditis:
Antibiotic therapy
• Subacute (alpha-strep)
– duration depends on the isolate’s degree of sensitivity to
beta-lactam antibiotics
– Sensitive strains treated with ceftriaxone 2gm IV daily x 2-4
weeks PLUS gentamicin 1mg/kg q12h x 2 weeks
• Acute (Staphylococcus aureus)
– (for MSSA) High-dose semisynthetic penicillin x 4-6 weeks
– (for MRSA) Vancomycin IV dosed to maintain 15-20mcg/ml
trough levels x 6 weeks
• Enterococcal endocarditis
– High-dose penicillin or ampicillin PLUS gentamicin 1mg/kg
q12h x 6 weeks (for drug susceptible strains)
For a more detailed discussion, see treatment guidelines from the
UK: Gould et al. J Antimicrob Chemother 2012; 67: 269-289
US: Baddour et al. Circulation 2005; 111: e394-e434
Treatment of endocarditis:
Indications for surgery
• Persistent positive blood cultures despite maximal
antibiotic therapy
• Recurrent embolism (>2 episodes)
• Valvular dysfunction leading to severe heart failure
• Myocardial abscess - heart block, fistulas, arrhythmias
• Fungal endocarditis (usually cannot be cured with
antibiotics alone)
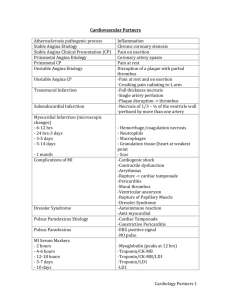
Infections of arteries
• Arteries
– Mycotic aneurysms
• almost always a complication of endocarditis
• yhey may rupture in spite of antibiotic treatment
– Aortitis
• rare infection following bacteremia in older
persons with extensive atherosclerotic disease
of the aorta
• associated with staphylococci (from
contaminated IVs) or with Salmonella (from
bacteremic intestinal infection)
Infections of veins:
septic thrombophlebitis
Syndrome
Veins
Predisposition
Microbiology
Treatment
Lemierre’s
syndrome
Internal
jugular v.
Prior exudative
pharyngitis
Fusobacterium
necrophorum
IV Penicillin G
Pylephlebitis
Portal v.
Diverticulitis; other
intraabdominal
infections
B. fragilis, other
intestinal bacteria
Broad-spectrum
IV therapy;
heparin
Septic pelvic
thrombophlebitis
Ovarian v.
and others
Post-partum
Intestinal flora
Broad-spectrum
IV therapy;
heparin
Line-related septic
phlebitis
Any small
or great
vein
Infection indwelling
IV catheters
usually Staph.
IV anti-staph
antibiotics;
excision of
purulent small
veins
Tuberculosis and the heart
• Active TB can present with pericarditis
• Usually associated with concurrent
pulmonary disease
• Treated as pulmonary TB with addition of
corticosteroids (to prevent scarring)
• Constrictive pericarditis is the dreaded longterm complication
– Causes impaired filling of the ventricles limited in
expansion by the stiff and unyielding pericardium
– Pericardiectomy may be necessary
Spirochetes and the Heart
• Syphilis:
– Heart involvment occurs in the tertiary stage of
disease, many years after acquisition
– Small numbers of spirochetes invade the aortic
root and induce destructive granulomatous
inflammation
– Long-standing disease causes enlargement of the
aortic root and aortic valve insufficiency
– Older adults with acquired aortic root dilation
and/or aortic insufficiency should have syphilis
serology performed.
Cardiovascular syphilis:
syphilitic aortitis
Source unknown
Any adult with aortic root dilation or aortic valve insufficiency
should have serologic testing for syphilis and receive treatment
for tertiary syphilis if confirmed positive.
Spirochetes and the Heart
• Lyme disease:
– caused by Borrelia burgdorferii (N. America) and
Borrelia afzeli (Europe)
– transmitted by Ixodes spp. tick bites
– Expanding, ring-like skin lesions occur at the bite
sites (“erythema chronicum migrans” or ECM)
– ECM followed by dissemination with self-limited
fever, arthralgia, neurologic and/or cardiac
manifestations after weeks to months.
– Long-standing, untreated disease may result in
chronic, recurrent arthritis or persistent CNS
symptoms.
Lyme carditis
Lyme carditis is the most common cause of reversible heart block
ECM
Sagar et al. Lancet
2012; 379: 738-47
Complete heart block associated with the disseminated phase
of Lyme disease. Note the dissociation of the atrial P-waves
(black arrows) from the ventricular QRS complexes (red
arrows)
American trypanosomiasis:
Chagas’ disease
Transmitted by the reduviid bug (triatomine)
– blood-sucking insect, lives in roof thatch or cracks in mud walls of
substandard rural housing in South and Central America
– the bug defecates while taking a blood meal; the pathogen,
Trypanosoma cruzi, is in the insect feces and is scratched into the
bite site by the victim.
CDC/World Health Organization, 1976 Public Health Image Library #2538
CDC/Alexander J. da Silva, PhD/Melanie Moser, 2002. Public Health Image Library #3384
American trypanosomiasis:
Chagas’ disease
Trypanosome seen in blood during
acute febrile infection x 4-6 weeks
CDC/Dr. Mae Melvin. 1977, Public
Health Image Library #3014
Intracellular, multiplying form of the
parasite; here seen in heart muscle
CDC/ Dr. L.L. Moore, Jr.,1969, Public
Health Image Library #470
After many decades of chronic infection, heart muscle is damaged by
mostly autoimmune mechanisms. Result = dilated cardiomyopathy,
arrhythmias, CHF
Similarly, parasites induce damage to myenteric plexus obliterating
peristalsis in the GI tract. Result = megacolon, megaesophagus
American trypanosomiasis:
Chagas’ disease
• After many decades of chronic infection, heart muscle is
damaged by mostly autoimmune mechanisms. Result =
dilated cardiomyopathy, arrhythmias, CHF
• Similarly, parasites induce damage to myenteric plexus
obliterating peristalsis in the GI tract. Result = megacolon,
megaesophagus
Madiha, 2011, posted on
www.about-child.com
Infection and EMF
(endomyocardial fibrosis)
• EMF occurs in tropical regions worldwide
• causes fibrosis of the endomyocardium with obliteration of the
either (or both) ventricular chambers--> CHF
• often preceded by profound eosinophilia
• true etiology of EMF ???
from Mocumbi et al. NEJM 2008; 359:43-9
Cary Engleberg, 2009
Infection and EMF
• Infections suspected of being
associated with EMF:
– Invasive helminth infections with chronic
massive eosinophilia
– Toxoplasmosis
– Myocarditis
– Malaria
– Acute rheumatic fever
Cardiovascular infections:
summary
• Acute myocarditis is usually due to enterovirus
infection
– causes symptoms of CHF
– brief episodes (<2 weeks) usually resolve completely
– extended episodes may result in chornic dilated
cardiomyopathy
• Acute pericarditis is usually also due to enterovirus
infection
– causes positional chest pain and characteristic EKG
changes
– usually self-limited
Cardiovascular infections:
summary (continued)
• Endocarditis is usually bacterial (Staph/Strep)
–
–
–
–
may be acute (Staph) or subacute (alpha-Strep)
usually a pre-disposing valvular abnomality is present
the valve becomes infected after bacteremia
diagnosis depends mostly on:
• presence of persistent bacteremia with a compatible organism
• evidence of a vegetation on a valve
– treatment requires high-dose, intravenous antibiotic therapy
for an extended time (usually 4-6 weeks)
• Arteries may become infected during endocarditis (mycotic
aneurysms) or after other bacteremias is patient with
atherosclerosis (aortitis)
• Septic thrombophlebitis occurs in several different veins.
Treatment involves high-dose antibiotics +/- heparin
Cardiovascular infections:
summary (continued)
• Tuberculous pericarditis is a extrapulmonary
form of active TB
– may scar and cause constrictive pericarditis
– treat as for TB with corticosteroids added to prevent scarring
• Tertiary syphilis can cause aortic root dilation
and aortic insufficiency
• Disseminated phase of Lyme disease is may
cause a reversible heart block
• Untreated American trypanosomiasis can
cause chronic dilated cardiomyopathy after
decades