Foundations in Microbiology
advertisement

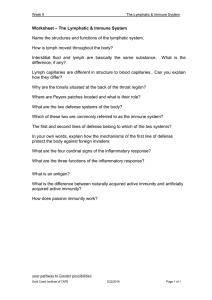
Lecture PowerPoint to accompany Foundations in Microbiology Sixth Edition Talaro Chapter 14 Nonspecific Host Defenses Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Defense Mechanisms of the Host • To protect the body against pathogens, the immune system relies on a multilevel network of physical barriers, immunologically active cells, and a variety of chemicals. – first line of defense – any barrier that blocks invasion at the portal of entry – nonspecific – second line of defense – protective cells and fluids; inflammation and phagocytosis – nonspecific – third line of defense – acquired with exposure to foreign substance; produces protective antibodies and creates memory cells – specific 2 Physical or Anatomical Barriers: First Line of Defense Skin and mucous membranes of respiratory, urogenital, eyes and digestive tracts – outermost layer of skin is composed of epithelial cells compacted, cemented together and impregnated with keratin; few pathogens can penetrate if intact – flushing effect of sweat glands – damaged cells are rapidly replaced – mucous coat impedes attachment and entry of bacteria – blinking and tear production – stomach acid – nasal hair traps larger particles 3 Nonspecific Chemical Defenses • Sebaceous secretions • Lysozyme, an enzyme that hydrolyzes the cell wall of bacteria, in tears • High lactic acid and electrolyte concentration in sweat • Skin’s acidic pH • Hydrochloric acid in stomach • Digestive juices and bile of intestines • Semen contains antimicrobial chemical. • Vagina has acidic pH. 4 5 Genetic Defenses • Some hosts are genetically immune to the diseases of other hosts. • Some pathogens have great specificity. • Some genetic differences exist in susceptibility. 6 Structure and Function of the Organs of Defense and Immunity • • The study of the body’s second and third lines of defense is called immunology. Functions of a healthy immune system: 1. Constant surveillance of the body 2. Recognition of foreign material 3. Destruction of entities deemed to be foreign 7 8 Immune System • • Large, complex, and diffuse network of cells and fluids that penetrate into every organ and tissue Four major subdivisions of immune system are: 1. 2. 3. 4. Reticuloendothelial system (RES) Extracellular fluid (ECF) Bloodstream Lymphatic system 9 10 Reticuloendothelial System (RES) • Network of connective tissue fibers that interconnects other cells and meshes with the connective tissue network surrounding organs • Inhabited by phagocytic cells – mononuclear phagocyte system – macrophages ready to attack and ingest microbes that passed the first line of defense 11 Origin, Composition, and Functions of the Blood • Whole blood consists of plasma and blood cells – red blood cells and white blood cells. – Serum is the liquid portion of the blood after a clot has formed-minus clotting factors. • Plasma – 92% water, metabolic proteins, globulins, clotting factors, hormones and all other chemicals and gases to support normal physiological functions 12 White Blood Cells • Neutrophils- 55-90% - lobed nuclei with lavender granules; phagocytes • Eosinophils – 1-3% - orange granules and bilobed nucleus; destroy eucaryotic pathogens • Basophils, mast cells – 0.5% - constricted nuclei, dark blue granules; release potent chemical mediators • Lymphocytes – 20-35% - large nucleus B (humoral immunity) and T cells (cell-mediated immunity) involved in the specific immune response • Monocytes, macrophages – 3-7%- large nucleus; phagocytic 13 Lymphatic System 1. Provides an auxiliary route for return of extracellular fluid to the circulatory system 2. Acts as a drain-off system for the inflammatory response 3. Renders surveillance, recognition, and protection against foreign material 14 15 Lymphatic Fluid • Lymph is a plasma-like liquid carried by lymphatic circulation • Formed when blood components move out of blood vessels into extracellular spaces • Made up of water, dissolved salts, 2-5% proteins • Transports white blood cells, fats, cellular debris and infectious agents 16 Lymphatic Vessels • Lymphatic capillaries permeate all parts of the body except the CNS. • Thin walls easily permeated by extracellular fluid which is then moved through contraction of skeletal muscles • Functions to return lymph to circulation; flow is one-direction-toward the hearteventually returning to blood stream 17 Lymphoid Organs and Tissues • Classified as primary and secondary • Primary lymphoid organs – sites of lymphocytic origin and maturation – thymus and bone marrow • Secondary lymphoid organs and tissues – circulatory-based locations such as spleen and lymph nodes; collections of cells distributed throughout body tissues – skin and mucous membranes – SALT, GALT, MALT 18 19 Lymphoid Organs • Thymus – high rate of growth and activity until puberty, then begins to shrink; site of Tcell maturation • Lymph nodes - small, encapsulated, beanshaped organs stationed along lymphatic channels and large blood vessels of the thoracic and abdominal cavities • Spleen – structurally similar to lymph node; filters circulating blood to remove worn out RBCs and pathogens 20 Actions of the Second Line of Defense • • • • • Recognition Inflammation Phagocytosis Interferon Complement 21 Recognition • Protein receptors within cell membrane of macrophages, called Toll-like receptors • Detect foreign molecules and signal the macrophage to produce chemicals which: – stimulate an inflammatory response (nonspecific) – promote the activity of B and T cells (specific) 22 Inflammatory Response Classic signs and symptoms characterized by: • Redness – increased circulation and vasodilation in injured tissue in response to chemical mediators and cytokines • Warmth – heat given off by the increased blood flow • Swelling – increased fluid escaping into the tissue as blood vessels dilate-edema; WBC’s, microbes, debris and fluid collect to form pus; helping prevent spread of infection • Pain – stimulation of nerve endings • Possible loss of function 23 Insert figure 14.13 Events in inflammation 24 Unique Characteristics of Leukocytes • Diapedesis – migration of cells out of blood vessels into the tissues • Chemotaxis – migration in response to specific chemicals at the site of injury or infection 25 26 Fever • Initiated by circulating pyrogens which reset the hypothalamus to increase body temperature; signals muscles to increase heat production and vasoconstriction – exogenous pyrogens – products of infectious agents – endogenous pyrogens – liberated by monocytes, neutrophils, and macrophages during phagcytosis; interleukin-1 (IL-1) and tumor necrosis factor (TNF) • Benefits of fever: – inhibits multiplication of temperature-sensitive microorganisms – impedes nutrition of bacteria by reducing the available iron – increases metabolism and stimulates immune reactions and protective physiological processes 27 Phagocytes and Phagocytosis 3 main types of phagocytes: 1. Neutrophils – general-purpose; react early to bacteria and other foreign materials, and to damaged tissue 2. Eosinophils – attracted to sites of parasitic infections and antigen-antibody reactions 3. Macrophages – derived from monocytes; scavenge and process foreign substances to prepare them for reactions with B and T lymphocytes 28 Phagocytosis General activities of phagocytes: 1. To survey tissue compartments and discover microbes, particulate matter and dead or injured cells 2. To ingest and eliminate these materials 3. To extract immunogenic information from foreign matter 29 30 Interferon • Small protein produced by certain white blood cells and tissue cells – alpha interferon- lymphocytes and macrophages – beta interferon – fibroblasts and epithelial cells – gamma interferon – T cells • Produced in response to viruses, RNA, immune products, and various antigens • Bind to cell surfaces and induce expression of antiviral proteins • Inhibit expression of cancer genes 31 32 Complement • Consists of 26 blood proteins that work in concert to destroy bacteria and viruses • Complement proteins are activated by cleavage. • Classical pathway – activated by the presence of antibody bound to microorganism • Alternative pathway – begins when complement proteins bind to normal cell wall and surface components of microorganisms 33 34 35