Preoperative Assessment in the Older Adult
advertisement

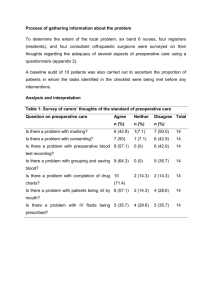
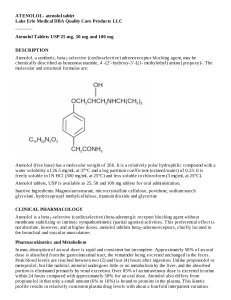
Preoperative Assessment in the Older Adult Lisa Caruso, MD, MPH Section of Geriatrics Boston University Medical Center Goals • To review the most common physiologic changes in the elderly which may impair one’s ability to compensate for operative stress • To describe the purpose of the preoperative assessment • To provide strategies to minimize operative risks Cardiovascular System • Changes in “mechanics” – Decrease in myocytes, increase in collagen resulting in decreased compliance – Autonomic tissue replaced by collagen resulting in conduction abnormalities – Decreased compliance of vascular system leading to increased systolic blood pressure with resulting ventricular hypertrophy Cardiovascular System • Changes in “control mechanisms” – decreased responsiveness to catacholamines due probably to impaired receptor function – decreased heart rate response to changes in circulatory volume may lead to congestive heart failure or hypotension (CO=SV x HR ==>preload dependency) Pulmonary System • Reduced chest wall compliance resulting in – increased work of breathing – reduced maximal minute ventilation • Reduced respiratory response to hypoxia by 50% (? Due to impaired chemoreceptor function) • Decreased ciliary function • Reduced cough and swallowing function Neurologic Changes • Decrease in cortical gray matter, neuronal volume, complexity of neuronal connections, synthesis of neurotransmitters • Neuronal loss and demyelination occur in the spinal cord resulting in changes in reflexes and reductions in proprioception • Vision and hearing loss make information processing more difficult Renal Changes • Decline in renal blood flow--10% per decade after age 50 • Old kidney has difficulty – maintaining circulating blood volume – with sodium homeostasis – removing excess acid – adjusting to hypovolemia, hemorrhage, low cardiac output and hypotension • Renal insufficiency may not be appreciated Adverse Drug Reactions (ADR) • Decrease in lean body mass with increased proportion of body fat • Decreased protein binding of certain drugs • Alterations in renal, CV, hepatic function may change drug concentrations and their duration of action • ADR’s increase with number of drugs administered and linearly with age Preoperative Assessment-Purposes • Not just for “clearance” • To identify factors associated with increased risks of specific complications related to a procedure • To recommend a management plan to minimize these risks Cassel CK, Leipzig RM, Cohen HJ, et al. Geriatric Medicine: An Evidence Based Approach, 4th ed. New York: Springer; 2003. Preoperative Assessment-Components • • • • Functional Assessment Cognitive Assessment Nutritional Assessment Review of advance directives – whether and when to withhold or withdraw support Functional Assessment • American Society of Anesthesiologists (ASA) score – Class I A normal healthy patient for elective operation – Class II A patient with mild systemic disease – Class III A patient with severe systemic disease that limits activity but is not incapacitating – Class IV A patient with incapacitating systemic disease that is a constant threat to life – Class V A moribund patient that is not expected to survive 24 hrs with or without the operation Functional Assessment • Exercise capacity – “inactive” defined as inability to leave the home on one’s own at least twice per week – increased CV risk in patients unable to meet a 4-MET demand during most daily activities • Activities of Daily Living – Correlated with post-op morbidity and mortality Cognitive Assessment • Not done uniformly • Dementia is a major predictor of post-op delirium • Use of Mini-Mental State Exam or orientation and recall testing • Much potential for future research Nutritional Assessment • Poor nutrition is a risk factor for – pneumonia – poor wound-healing – 30-day mortality • Hypoalbuminemia (<3.3mg/dL) – increased length of stay – increased rates of readmission – unfavorable disposition – increased all-cause mortality Corti M. Serum albumin level and physical disability as predictors of mortality in older persons.JAMA 1994;272:1036. Strategies to Minimize Risk • Routine screening is low yield – preop testing should be based on the type of surgery • Manage hypertension – lower blood pressure to under 180/110 • In patients with dementia, consider placement of epidural to control pain without sedation thus minimizing risk for delirium • Avoid long periods without nutrition – little evidence, but should try to improve nutritional status prior to elective surgery Strategies to Minimize Risk • Perioperative use of ß-blockers – Mangano, et al., NEJM 1996, RDBPCT – In patients with or at risk for CAD, does IV atenolol decrease periop CV morbidity and increase overall survival? – Cardiac RF included: age > 65, hypertension, smoking, cholesterol > 240, and diabetes. – 200 pts enrolled; IV atenolol 10 mg given 30 min prior to surgery, 50-100 mg bid POD 1-7 – 192 followed for 2 yrs Strategies to Minimize Risk Two years Overall mortality Placebo 21% Atenolol 10% RRR 52% ARR 11% NNT 9 Event-free survival after hospital discharge at 2 years was 68% in the placebo group and 83% in the atenolol group (p=0.008). Not clear yet if age alone is an indication for use of ßblockers in perioperative period. Strategies to Minimize Risk • Diabetic Postoperative Mortality and Morbidity (DIPOM) study • Perioperative Ischemic Evaluation (POISE) trial • Metoprolol after Vascular Surgery (MaVS) trial Http://www.medscape.com/viewarticle/494679 Reuben DB, et al. Geriatrics at Your Fingertips 2005, 7th edition. New York, American Geriatrics Society, 2005. Summary • Older adults have decreased reserves in multiple organ systems. • Disease burden and functional capacity outweigh age when assessing preoperative risk. • Collaboration among providers helps to identify functional, cognitive and nutritional deficits and to create management plans to minimize these deficits when possible.