Motor units
advertisement

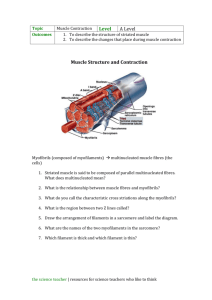
1. What is a hypothesis? Create your own example. 2. How does a conclusion and hypothesis relate? 1. Draw this picture in your notebook and label the pieces you know. 2. What does this have to do with muscles? Structure and Function of Exercising Muscle Three Types of Muscle Tissue • Smooth muscle: involuntary, hollow organs • Cardiac muscle: involuntary, heart • Skeletal muscle: voluntary, skeleton Skeletal Muscle Anatomy • Entire muscle – Surrounded by epimysium – Consists of many bundles (fasciculi) • Fasciculi – Surrounded by perimysium – Consists of individual muscle cells (muscle fibers) • Muscle fiber – Surrounded by endomysium – Consists of myofibrils divided into sarcomeres Structure of Muscle Fibers • Sarcoplasm – Cytoplasm of muscle cell – Unique features: glycogen storage • Transverse tubules (T-tubules) – Carry action potential deep into muscle fiber (highway) • Sarcoplasmic reticulum (SR): Ca2+ storage Run Perpendicular Myofibrils and Sarcomeres • Myofibrils – Muscle fasciculi muscle fiber myofibril – Hundreds to thousands per muscle fiber • Sarcomeres – Basic contractile element of skeletal muscle – End to end for full myofibril length Sarcomeres • Distinctive striped appearance (striations) – – – – A-bands: dark stripes I-bands: light stripes H-zone: middle of A-band M-line: middle of H-zone • Common boundary structure: Z-disk Sarcomere: Protein Filaments • Used for muscle contraction • Actin (thin filaments) – Show up lighter under microscope – I-band contains only actin filaments • Myosin (thick filaments) – Show up darker under microscope – A-band contains both actin and myosin filaments – H-zone contains only myosin filaments Myosin (Thick Filaments) • Two intertwined filaments with globular heads • Globular heads – Protrude 360° from thick filament axis – Will interact with actin filaments for contraction Actin (Thin Filaments) • Actually composed of three proteins – Actin: contains myosin-binding site – Tropomyosin: covers active site at rest – Troponin: anchored to actin, moves tropomyosin • Anchored at Z-disk and Equally spaced out by titin Motor Units • a-Motor neurons innervate muscle fibers • Motor unit – Single a-motor neuron + all fibers it innervates – More operating motor units = more contractile force • Neuromuscular junction – Site of communication between neuron and muscle – Consists of synapse between a-motor neuron and muscle fiber Skeletal Muscle Contraction (Excitation-Contraction Coupling) 1. Action potential (AP) starts in brain 2. AP arrives at axon terminal, releases acetylcholine (ACh) 3. ACh crosses synapse, binds to ACh receptors on plasmalemma 4. AP travels down plasmalemma, T-tubules 5. Triggers Ca2+ release from sarcoplasmic reticulum (SR) 6. Ca2+ enables actin-myosin contraction Role of Ca2+ in Muscle Contraction • AP arrives at SR from T-tubule – SR sensitive to electrical charge – Causes mass release of Ca2+ into sarcoplasm • Ca2+ binds to troponin on thin filament – At rest, tropomyosin covers myosin-binding site, blocking actin-myosin attraction – Troponin-Ca2+ complex moves tropomyosin – Myosin binds to actin, contraction can occur Sliding Filament Theory: How Muscles Create Movement • Process of actin-myosin contraction • Relaxed state – No actin-myosin interaction at binding site – Myofilaments overlap a little • Contracted state – Myosin head pulls actin toward sarcomere center (power stroke) – Filaments slide past each other – Sarcomeres, myofibrils, muscle fiber all shorten Sliding Filament Theory: How Muscles Create Movement • After power stroke ends – Myosin detaches from active site – Myosin head rotates back to original position – Myosin attaches to another active site farther down • Process continues until – Z-disk reaches myosin filaments or – AP stops, Ca2+ gets pumped back into SR Energy for Muscle Contraction • Adenosine triphosphate (ATP) • Binds to myosin head – ATPase on myosin head – ATP ADP + Pi + energy • Necessary for muscle contraction Muscle Relaxation • AP ends, electrical stimulation of SR stops • Ca2+ pumped back into SR – Stored until next AP arrives – Requires ATP • Without Ca2+, troponin and tropomyosin return to resting conformation – Covers myosin-binding site – Prevents actin-myosin cross-bridging 1. Draw this picture in your notebook and label the pieces you know. 2. What does this have to do with muscles? Muscle Fiber Types • Type I – ~50% of fibers in an average muscle – Peak tension in 110 ms (slow twitch) • Type II – Peak tension in 50 ms (fast twitch) – Type IIa (~25% of fibers in an average muscle) – Type IIx (~25% of fibers in an average muscle) Type I Versus Type II Differentiation • Speed of myosin ATPase varies – Fast myosin ATPase = fast contraction cycling – Slower myosin ATPase = slower contraction cycling • Muscle biopsy – Small (10-100 g) piece of muscle removed – Frozen, sliced, examined under microscope • Gel electrophoresis – Type I versus II fibers have different types of myosin – Separates different types of myosin by size Muscle Biopsy Type I Versus Type II • Sarcoplasmic reticulum – Type II fibers have a more highly developed SR – Faster Ca2+ release, 3 to 5 times faster Vo • Motor units – Type I motor unit: smaller neuron, <300 fibers – Type II motor unit: larger neuron, >300 fibers Type I Versus Type II: Peak Power • Peak power: type IIx > type IIa > type I – Effects of different SR, motor units, etc. – Single muscle fiber recording • Regardless of fiber type, all muscle fibers reach peak power at ~20% peak force Single Muscle Fiber Peak Power Distribution of Fiber Types: Type I:Type II Ratios • Each person has different ratios • Arm and leg ratios are similar in one person – Endurance athlete: type I predominates – Power athlete: type II predominates • Soleus: type I in everyone Type I Fibers During Exercise • High aerobic endurance – Can maintain exercise for prolonged periods – Require oxygen for ATP production – Low-intensity aerobic exercise, daily activities • Efficiently produce ATP from fat, carbohydrate Type II Fibers During Exercise • Type II fibers in general – Poor aerobic endurance, fatigue quickly – Produce ATP anaerobically • Type IIa – More force, faster fatigue than type I – Short, high-intensity endurance events (1,600 m run) • Type IIx – Seldom used for everyday activities – Short, explosive sprints (100 m) Fiber Type Determinants • Genetic factors – Determine which a-motor neurons innervate fibers – Fibers differentiate based on a-motor neuron • Training factors – Endurance versus strength training, detraining – Can induce small (10%) change in fiber type • Aging: muscles lose type II motor units Muscle Fiber Recruitment • Also called motor unit recruitment • Method for altering force production – Less force production: fewer or smaller motor units – More force production: more or larger motor units – Type I motor units smaller than type II • Recruitment order: type I, type IIa, type IIx Orderly Recruitment and the Size Principle • Recruit minimum number of motor units needed – Smallest (type I) motor units recruited first – Midsized (type IIa) motor units recruited next – Largest (type IIx) motor units recruited last • Recruited in same order each time • Size principle: order of recruitment of motor units directly related to size of a-motor neuron Fiber Type and Athletic Success • Endurance athletes—type I predominates • Sprinters—type II predominates • Fiber type not sole predictor of success – – – – Cardiovascular function Motivation Training habits Muscle size Types of Muscle Contraction • Static (isometric) contraction – Muscle produces force but does not change length – Joint angle does not change – Myosin cross-bridges form and recycle, no sliding • Dynamic contraction – Muscle produces force and changes length – Joint movement produced Dynamic Contraction Subtypes • Concentric contraction – Muscle shortens while producing force – Most familiar type of contraction – Sarcomere shortens, filaments slide toward center • Eccentric contraction – Muscle lengthens while producing force – Cross-bridges form but sarcomere lengthens – Example: lowering heavy weight Generation of Force • Motor unit recruitment – Type II motor units = more force – Type I motor units = less force – Fewer small fibers versus more large fibers • Frequency of stimulation (rate coding) – Twitch – Summation – Tetanus Generation of Force • Length-tension relationship – Optimal sarcomere length = optimal overlap – Too short or too stretched = little or no force develops • Speed-force relationship – Concentric: maximal force development decreases at higher speeds – Eccentric: maximal force development increases at higher speeds